Back
Poster Session A
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (0372–0402) Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster I
0402: Opioid Use and Healthcare Utilization in Adults with PsA and AS
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
.png)
Alexis Ogdie, MD
Rheumatologist, Associate Professor of Medicine
University of Pennsylvania
Philadelphia, PA, United States
Abstract Poster Presenter(s)
Alexis Ogdie1, Sofia Pedro2, Jean Liew3 and Kaleb Michaud4, 1Department of Medicine, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, 2Forward, The National Databank for Rheumatic Diseases, Wichita, KS, 3Boston University, Boston, MA, 4University of Nebraska Medical Center, Omaha, NE
Background/Purpose: Opioid use among individuals with spondyloarthritis is common, reported to be ~20-30% in some cohorts. Data on whether this subset of patients have higher utilization of the healthcare system are lacking. Our objective was to examine the association between opioid use and healthcare utilization and costs among patents with psoriatic arthritis (PsA) and ankylosing spondylitis (AS).
Methods: This retrospective cohort study included adult participants enrolled in the FORWARD Databank. Patients who were diagnosed with PsA or AS and completed ≥ 1 questionnaire with Health Assessment Questionnaire Disability Index (HAQ-DI) and/or Bath Ankylosing Spondylitis Disease Activity Index (BASDAI; added in 2018) from January 2010 to December 2019 were included. PsA and AS were studied separately and among the available questionnaires available, the most recent observation period was used. Patient report of opioid use was the exposure of interest, and the outcomes were healthcare utilization and prescription costs over the course of one year. Student's t-tests or Chi-squared tests were used when appropriate to examine differences in costs by group. To measure the association between opioid use and the utilization outcomes, we used negative binomial regressions and report both models adjusted for age and sex, and additionally adjusted for hospitalization. To model the association between opioid use and costs, we used generalized linear models with gamma distribution and log link function.
Results: Of 828 PsA patients, 21.3% (177) used opioids. Of 334 AS patients, 27.4% (91) used opioids. Opioids users had more comorbidities, higher prevalence of smoking, and worse disease activity (by HAQ-DI or BASDAI) in both cohorts. They also tended to have higher use of any anti-rheumatic drug class (Table 1). Opioid users were more likely to have higher health care utilization and medical costs, specifically medical visits, diagnostic tests, direct medical costs and pharmacy costs (biologics and other drugs) (Tables 2 and 3). PsA opioid users had a 33% more medical visits annually when compared those not using opioids (results adjusted for age, sex, and hospitalizations). Similarly, patients with AS utilizing opioids had a 32% increase in medical visits compared to patients not using opioids. Annual number of diagnostic tests were similarly elevated for opioid users: 56% (PsA) and 68% (AS). Patients using opioids spent more on medical visits annually compared to those not using opioids: 28% more among those with PsA (3464.7 USD) and similarly among those with AS (4576.2 USD). Opioid users (PsA or AS patients) also tended to spend more on medications including biologics, csDMARDs, and other drug costs.
Conclusion: Compared to patients not using opioids, patients with PsA and AS who used opioids had higher healthcare utilization and higher costs. New care pathways for these patients are needed to improve care and reduce costs.
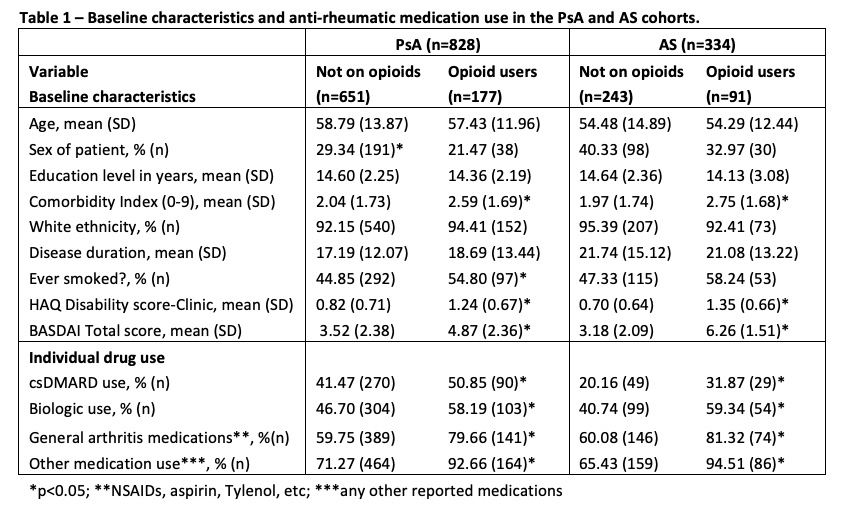 Table 1. Baseline characteristics and anti-rheumatic medication use in the PsA and AS cohorts.
Table 1. Baseline characteristics and anti-rheumatic medication use in the PsA and AS cohorts.
.jpg) Table 2. Mean (SD) of the annualized healthcare utilization and costs by diagnosis and opioid use.
Table 2. Mean (SD) of the annualized healthcare utilization and costs by diagnosis and opioid use.
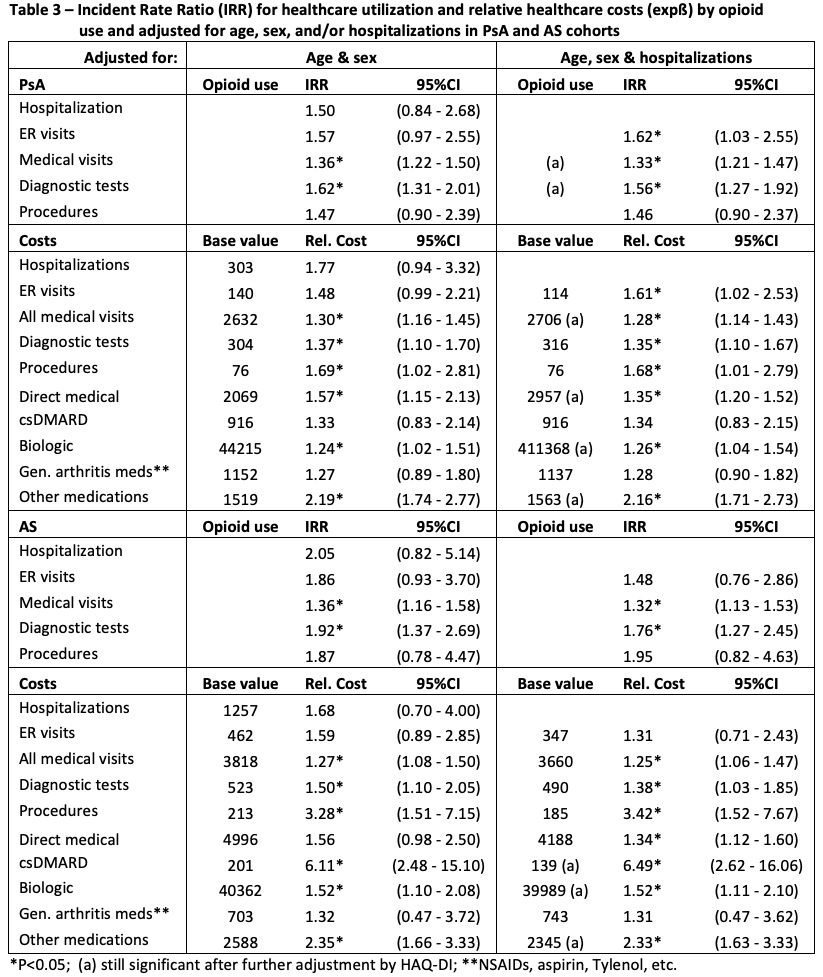 Table 3. Incident Rate Ratio (IRR) for healthcare utilization and relative healthcare costs (expß) by opioid use and adjusted for age, sex, and/or hospitalizations in PsA and AS cohorts
Table 3. Incident Rate Ratio (IRR) for healthcare utilization and relative healthcare costs (expß) by opioid use and adjusted for age, sex, and/or hospitalizations in PsA and AS cohorts
Disclosures: A. Ogdie, AbbVie, Amgen, Novartis, Pfizer Inc, Bristol-Myers Squibb, Celgene, Janssen, CorEvitas, Gilead Sciences, Eli Lilly, GlaxoSmithKline, Happify Health, UCB; S. Pedro, None; J. Liew, None; K. Michaud, None.
Background/Purpose: Opioid use among individuals with spondyloarthritis is common, reported to be ~20-30% in some cohorts. Data on whether this subset of patients have higher utilization of the healthcare system are lacking. Our objective was to examine the association between opioid use and healthcare utilization and costs among patents with psoriatic arthritis (PsA) and ankylosing spondylitis (AS).
Methods: This retrospective cohort study included adult participants enrolled in the FORWARD Databank. Patients who were diagnosed with PsA or AS and completed ≥ 1 questionnaire with Health Assessment Questionnaire Disability Index (HAQ-DI) and/or Bath Ankylosing Spondylitis Disease Activity Index (BASDAI; added in 2018) from January 2010 to December 2019 were included. PsA and AS were studied separately and among the available questionnaires available, the most recent observation period was used. Patient report of opioid use was the exposure of interest, and the outcomes were healthcare utilization and prescription costs over the course of one year. Student's t-tests or Chi-squared tests were used when appropriate to examine differences in costs by group. To measure the association between opioid use and the utilization outcomes, we used negative binomial regressions and report both models adjusted for age and sex, and additionally adjusted for hospitalization. To model the association between opioid use and costs, we used generalized linear models with gamma distribution and log link function.
Results: Of 828 PsA patients, 21.3% (177) used opioids. Of 334 AS patients, 27.4% (91) used opioids. Opioids users had more comorbidities, higher prevalence of smoking, and worse disease activity (by HAQ-DI or BASDAI) in both cohorts. They also tended to have higher use of any anti-rheumatic drug class (Table 1). Opioid users were more likely to have higher health care utilization and medical costs, specifically medical visits, diagnostic tests, direct medical costs and pharmacy costs (biologics and other drugs) (Tables 2 and 3). PsA opioid users had a 33% more medical visits annually when compared those not using opioids (results adjusted for age, sex, and hospitalizations). Similarly, patients with AS utilizing opioids had a 32% increase in medical visits compared to patients not using opioids. Annual number of diagnostic tests were similarly elevated for opioid users: 56% (PsA) and 68% (AS). Patients using opioids spent more on medical visits annually compared to those not using opioids: 28% more among those with PsA (3464.7 USD) and similarly among those with AS (4576.2 USD). Opioid users (PsA or AS patients) also tended to spend more on medications including biologics, csDMARDs, and other drug costs.
Conclusion: Compared to patients not using opioids, patients with PsA and AS who used opioids had higher healthcare utilization and higher costs. New care pathways for these patients are needed to improve care and reduce costs.
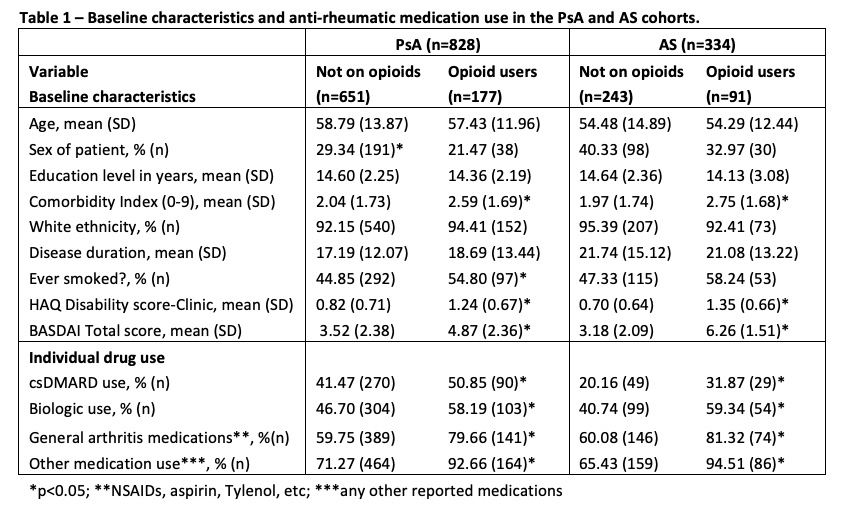 Table 1. Baseline characteristics and anti-rheumatic medication use in the PsA and AS cohorts.
Table 1. Baseline characteristics and anti-rheumatic medication use in the PsA and AS cohorts. .jpg) Table 2. Mean (SD) of the annualized healthcare utilization and costs by diagnosis and opioid use.
Table 2. Mean (SD) of the annualized healthcare utilization and costs by diagnosis and opioid use.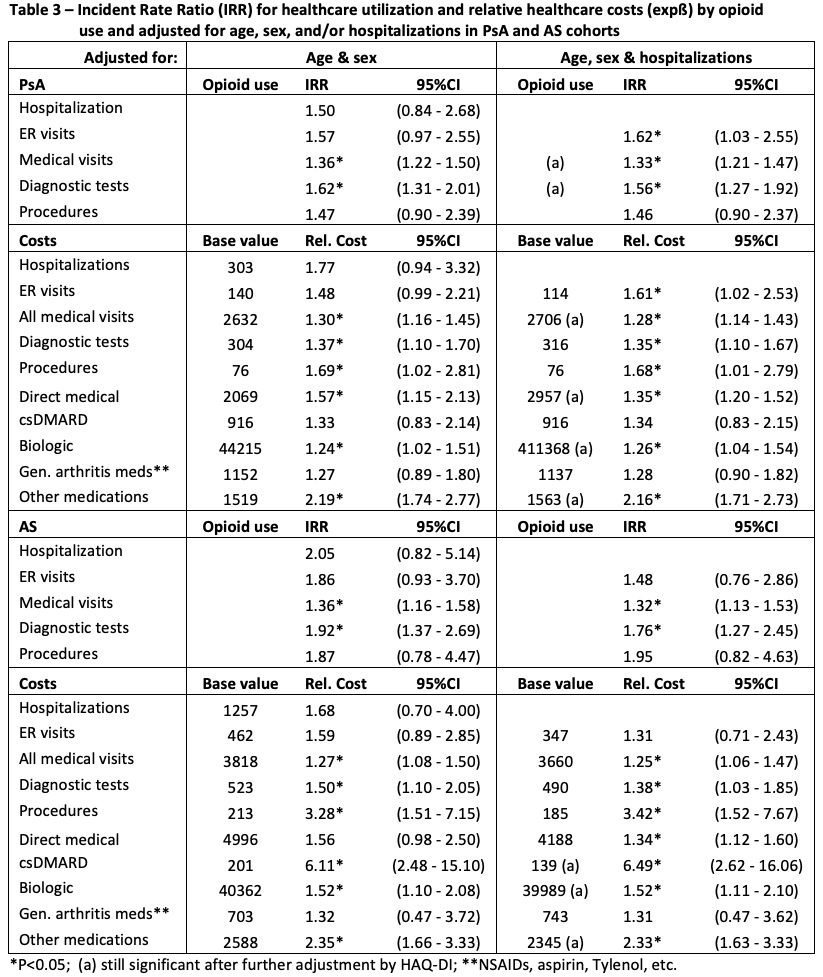 Table 3. Incident Rate Ratio (IRR) for healthcare utilization and relative healthcare costs (expß) by opioid use and adjusted for age, sex, and/or hospitalizations in PsA and AS cohorts
Table 3. Incident Rate Ratio (IRR) for healthcare utilization and relative healthcare costs (expß) by opioid use and adjusted for age, sex, and/or hospitalizations in PsA and AS cohorts Disclosures: A. Ogdie, AbbVie, Amgen, Novartis, Pfizer Inc, Bristol-Myers Squibb, Celgene, Janssen, CorEvitas, Gilead Sciences, Eli Lilly, GlaxoSmithKline, Happify Health, UCB; S. Pedro, None; J. Liew, None; K. Michaud, None.

