Back
Poster Session A
Vasculitis
Session: (0458–0497) Vasculitis – Non-ANCA-Associated and Related Disorders Poster I: Giant Cell Arteritis
0478: Sonographic Prevalence of Subclinical GCA in Newly Diagnosed PMR
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- CK
Colm Kirby, MD
Tallaght University Hospital
DUBLIN, Dublin, Ireland
Abstract Poster Presenter(s)
Colm Kirby1, Rachael Flood1, Ronan Mullan1, Grainne Murphy2 and David Kane1, 1Tallaght University Hospital, Dublin, Ireland, 2Cork University Hospital, Cork, Ireland
Background/Purpose: It has been reported that 20-50% of patients with PMR have subclinical GCA. The natural history of US-defined subclinical GCA in PMR is not known.
Methods: Twenty five newly-diagnosed PMR patients who met a clinical diagnosis for PMR, verified by 2 rheumatologists, were examined by US. US of all 6 branches of the superficial temporal arteries and both axillary arteries was performed using a GE P9 device. Sonographic abnormalities considered indicative of vasculitis in the temporal arteries included the halo sign (Fig. 1) and non-compressible arteries with a thickened intima-media complex. In the axillary arteries, a halo sign and an intima-media thickness of >1.0mm was considered positive. Follow-up consultations after 1 year were undertaken to review the clinical diagnosis. In our subclinical GCA group, a PMR-dose steroid taper was used in those with a prompt clinical response, a GCA-dose steroid taper was initiated for those who subsequently flared and Tocilizumab was initiated in the event of a second flare.
Results: Our cohort consisted of 64% females (n=16) with a mean age of 67 years (range 50-84). 2012 ACR/EULAR classification criteria were met in 16/25 patients (primarily due to prior corticosteroid use in primary care resulting in normal ESR/CRP).
Five patients (20%) were identified as having subclinical GCA on US (5/5 met 2012 ACR/EULAR PMR classification criteria, 0/5 met ACR GCA classification criteria). Temporal artery involvement was identified in 5/5, with axillary involvement in 1/5. Mean halo count was 3 (range 1-5) and mean halo score was 21.2 (range 17-29).Two patients were managed with an initial PMR-dose of prednisolone but relapsed. Three patients were treated with an initial GCA-dose of steroids, all of whom relapsed.
At a median of 12 months follow up 1/20 (5%) of the PMR-only cohort had developed clinical signs of GCA. 5/5 (100%) of the subclinical GCA cohort had developed a clinical diagnosis of GCA with 3/5 requiring an increase in steroid dose and 2/5 requiring Tocilizumab. At 12 months follow up 0% of patients had developed ischaemic complications.
Conclusion: Our study indicates that a single screening US of temporal and axillary arteries accurately identified 83.3% of patients with subclinical GCA in an inception PMR cohort. Our experience indicates that these patients are likely to be resistant to PMR-dose steroids and ultimately may require biologic therapy.
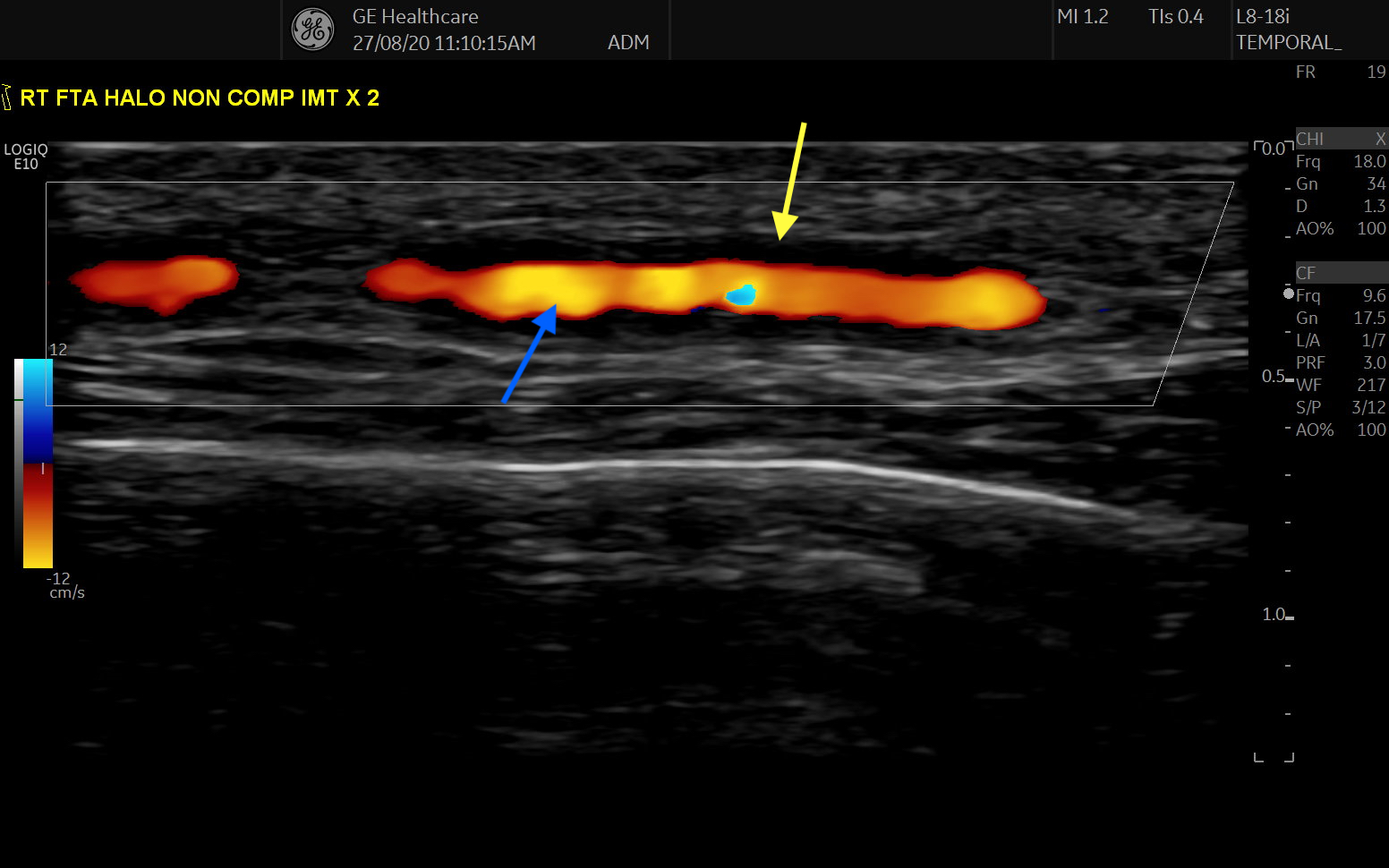 Figure 1: Longitudinal view of the frontal branch of the superficial temporal artery, demonstrating a halo sign, as indicated by the anechoic region (yellow arrow) surrounding the inner Doppler (blue arrow) signal.
Figure 1: Longitudinal view of the frontal branch of the superficial temporal artery, demonstrating a halo sign, as indicated by the anechoic region (yellow arrow) surrounding the inner Doppler (blue arrow) signal.
Disclosures: C. Kirby, None; R. Flood, None; R. Mullan, None; G. Murphy, AbbVie/Abbott; D. Kane, AbbVie/Abbott.
Background/Purpose: It has been reported that 20-50% of patients with PMR have subclinical GCA. The natural history of US-defined subclinical GCA in PMR is not known.
Methods: Twenty five newly-diagnosed PMR patients who met a clinical diagnosis for PMR, verified by 2 rheumatologists, were examined by US. US of all 6 branches of the superficial temporal arteries and both axillary arteries was performed using a GE P9 device. Sonographic abnormalities considered indicative of vasculitis in the temporal arteries included the halo sign (Fig. 1) and non-compressible arteries with a thickened intima-media complex. In the axillary arteries, a halo sign and an intima-media thickness of >1.0mm was considered positive. Follow-up consultations after 1 year were undertaken to review the clinical diagnosis. In our subclinical GCA group, a PMR-dose steroid taper was used in those with a prompt clinical response, a GCA-dose steroid taper was initiated for those who subsequently flared and Tocilizumab was initiated in the event of a second flare.
Results: Our cohort consisted of 64% females (n=16) with a mean age of 67 years (range 50-84). 2012 ACR/EULAR classification criteria were met in 16/25 patients (primarily due to prior corticosteroid use in primary care resulting in normal ESR/CRP).
Five patients (20%) were identified as having subclinical GCA on US (5/5 met 2012 ACR/EULAR PMR classification criteria, 0/5 met ACR GCA classification criteria). Temporal artery involvement was identified in 5/5, with axillary involvement in 1/5. Mean halo count was 3 (range 1-5) and mean halo score was 21.2 (range 17-29).Two patients were managed with an initial PMR-dose of prednisolone but relapsed. Three patients were treated with an initial GCA-dose of steroids, all of whom relapsed.
At a median of 12 months follow up 1/20 (5%) of the PMR-only cohort had developed clinical signs of GCA. 5/5 (100%) of the subclinical GCA cohort had developed a clinical diagnosis of GCA with 3/5 requiring an increase in steroid dose and 2/5 requiring Tocilizumab. At 12 months follow up 0% of patients had developed ischaemic complications.
Conclusion: Our study indicates that a single screening US of temporal and axillary arteries accurately identified 83.3% of patients with subclinical GCA in an inception PMR cohort. Our experience indicates that these patients are likely to be resistant to PMR-dose steroids and ultimately may require biologic therapy.
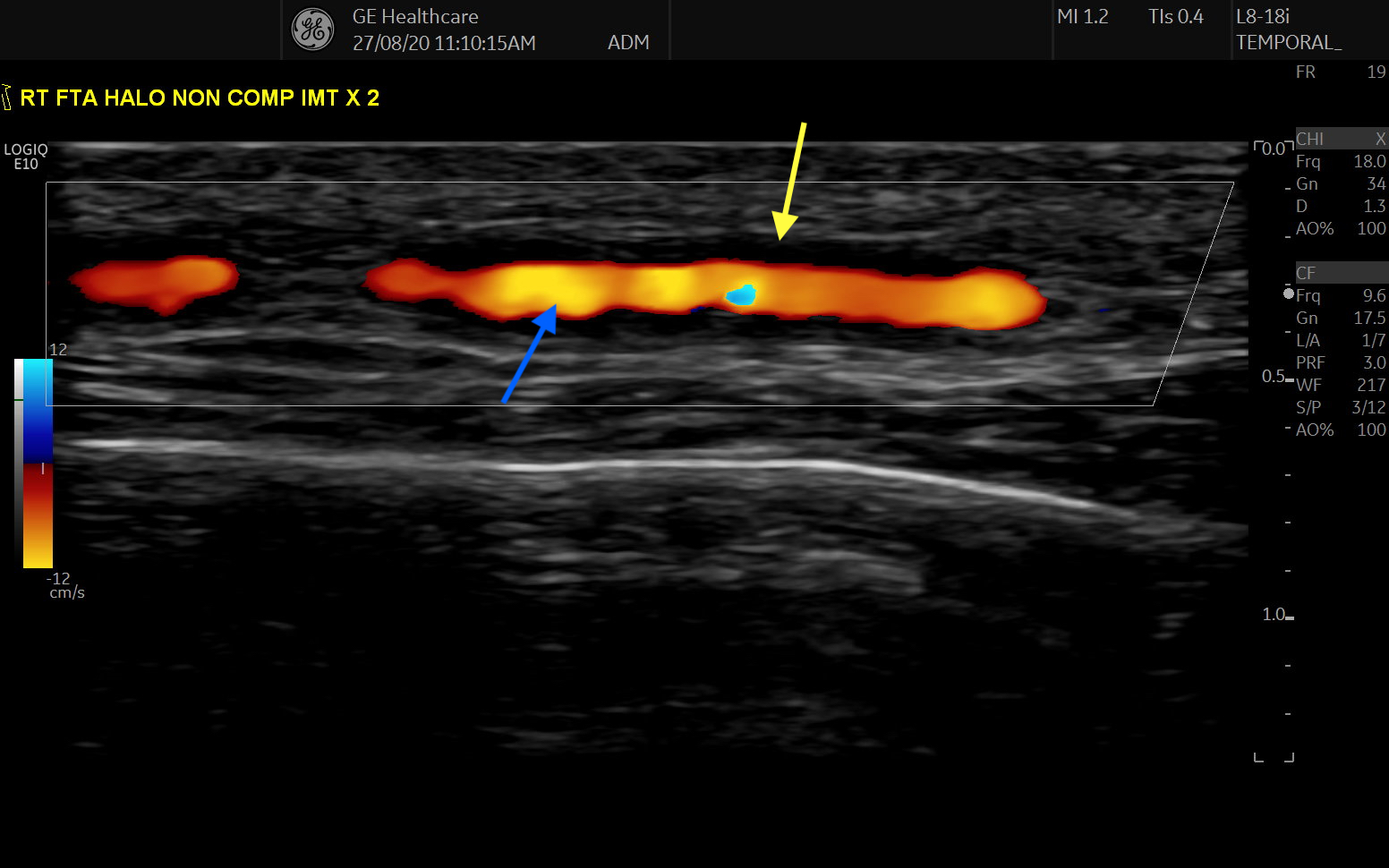 Figure 1: Longitudinal view of the frontal branch of the superficial temporal artery, demonstrating a halo sign, as indicated by the anechoic region (yellow arrow) surrounding the inner Doppler (blue arrow) signal.
Figure 1: Longitudinal view of the frontal branch of the superficial temporal artery, demonstrating a halo sign, as indicated by the anechoic region (yellow arrow) surrounding the inner Doppler (blue arrow) signal.Disclosures: C. Kirby, None; R. Flood, None; R. Mullan, None; G. Murphy, AbbVie/Abbott; D. Kane, AbbVie/Abbott.

