Back
Poster Session D
Osteoarthritis (OA) and related disorders
Session: (1888–1923) Osteoarthritis – Clinical Poster
1896: Alkylresorcinol, a Biomarker for Whole Grain Intake, and Its Association with Osteoarthritis: The MOST Study
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- JZ
Juan-Pablo Zertuche, MD
Boston University
Boston, MA, United States
Abstract Poster Presenter(s)
Juan-Pablo Zertuche1, Gabriela Rabasa1, Alice H. Lichtenstein2, Nirupa R. Matthan2, Michael Nevitt3, James Torner4, Cora E. Lewis5, Devyani Misra6 and David Felson1, 1Boston University, Boston, MA, 2Tufts University, Boston, MA, 3University of California at San Francisco, Orinda, CA, 4University of Iowa, Iowa City, IA, 5University of Alabama at Birmingham, Birmingham, AL, 6Beth Israel Deconess Medical Center, Boston, MA
Background/Purpose: Whole grains, particularly wheat, are an important source of dietary fiber in the US. By providing a fermentable source, whole grains can modify the gut microbiome preventing and improving dysbiosis, and have been reported to protect against chronic disease, including incident symptomatic OA and worsening knee pain.
Alkylresorcinol (AR) (1,3-dihydroxy-5-n-alkylbenzene) is a phenolic lipid with five homologues (C17:0, C19:0, C21:0, C23:0, C25:0) found in high amounts in most whole grains. Plasma AR concentrations remain stable up to 3.9 years, making it a good biomarker of long-term whole grain intake. Biomarkers, as a proxy of dietary intake, can overcome misclassification of dietary exposure base on self-reported dietary intake.
We examined whether fasting AR levels of the predominant AR homologues (C19:0, C21:0), as well as the sum of C17:0 through C25:0, were associated with the development of OA.
Methods: Participants from the Multicenter Osteoarthritis study (MOST) at risk of developing or with knee OA were studied. Knee x-rays and knee symptoms were assessed at baseline and through a 60-month follow-up period. Aliquots of plasma stored at -80°C from the baseline visit were analyzed for AR homologues and total AR using an established (UPLC-QTOF-MS) method.
We carried out two nested case-control studies using risk-set sampling, one for incident radiographic OA (new onset KL >= grade 2) and one for incident symptomatic OA (combination of knee pain on most days + radiographic OA) and examined the relationship between baseline plasma ARs and incident OA at 60 months. Given individual's changing diets, we also tested baseline AR levels with 30-month OA outcomes.
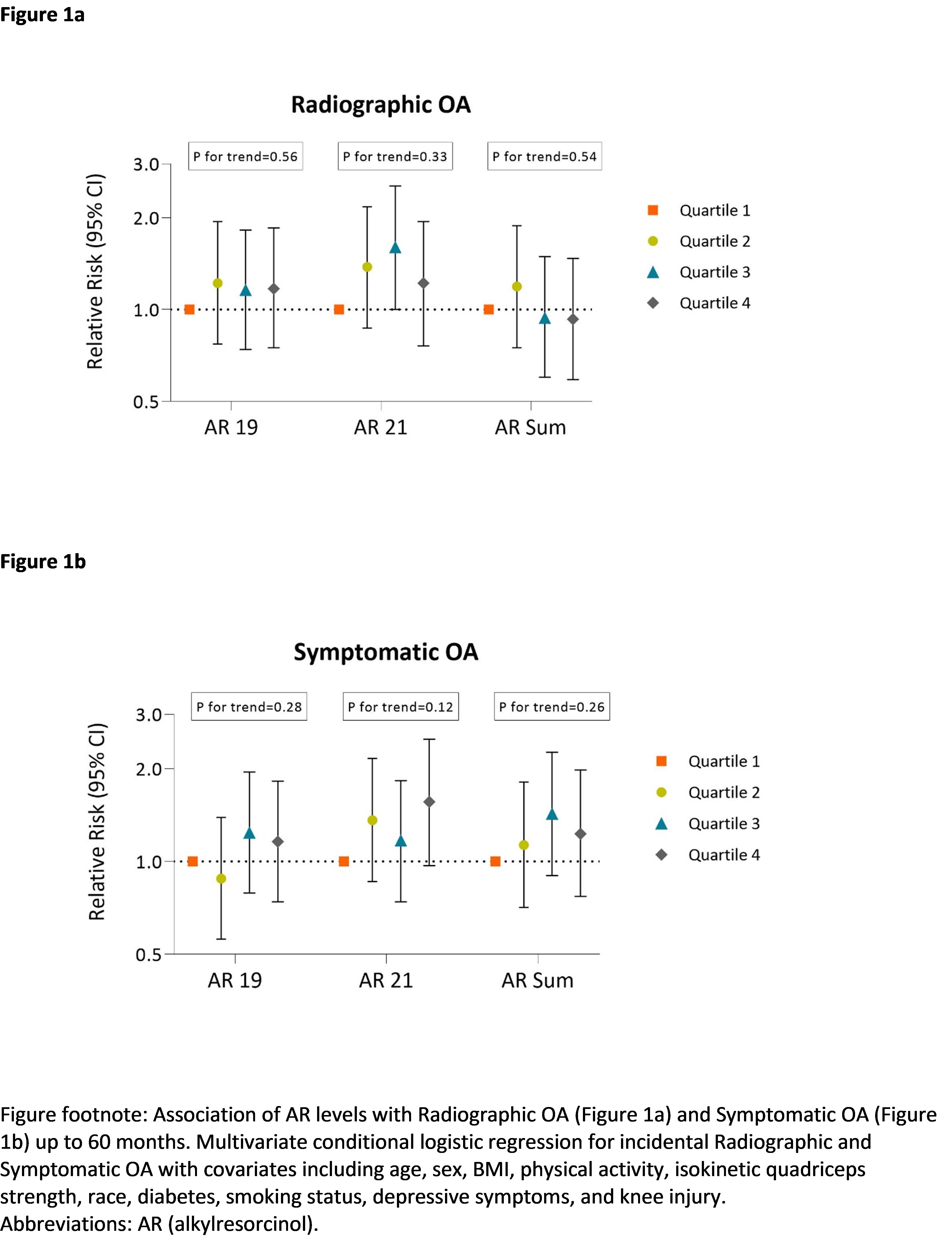
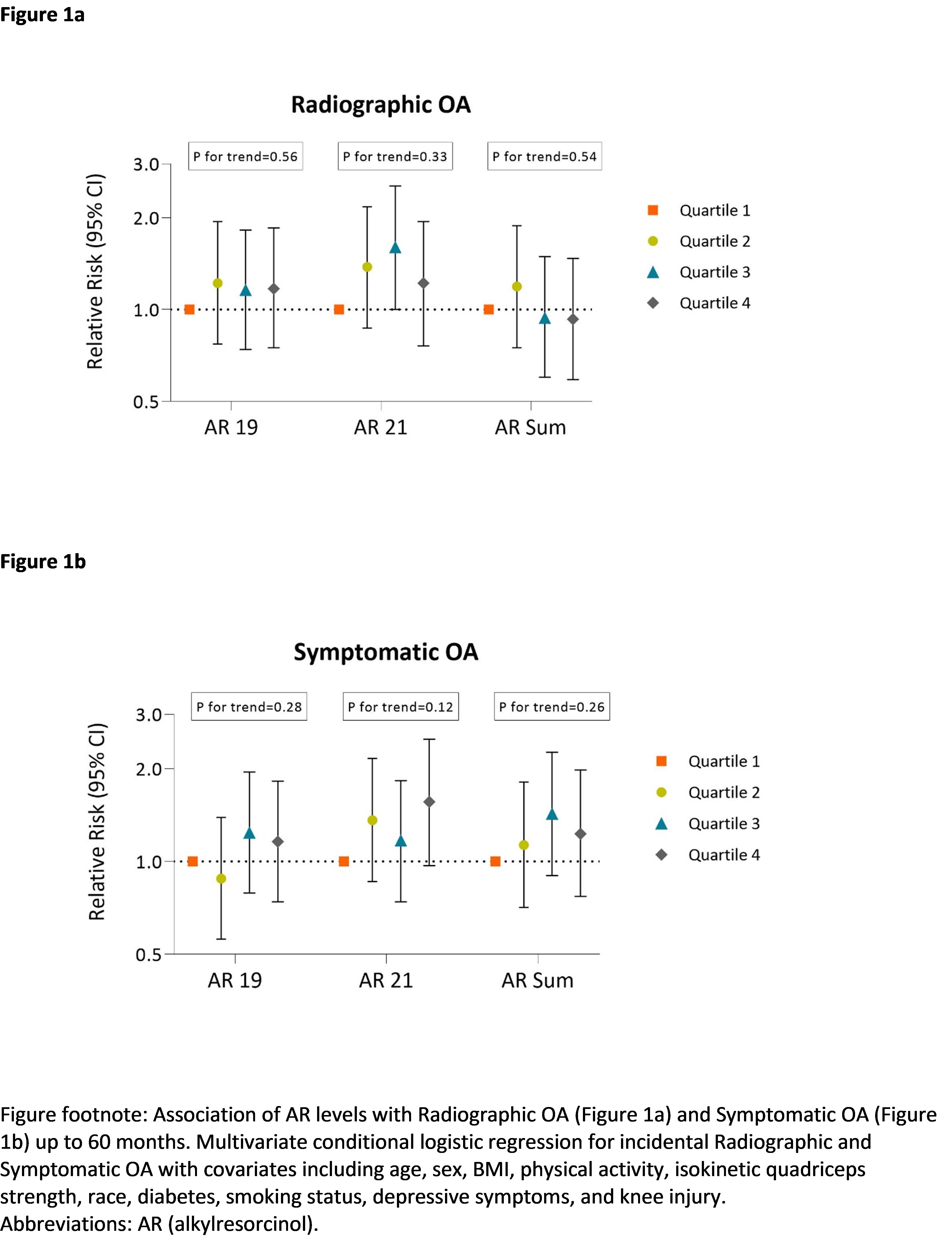
Multivariable conditional logistic regression with covariates including age, sex, BMI, physical activity (using PASE 39), isokinetic quadriceps strength, smoking status, depressive symptoms (using CES-D scale), self-reported race, clinic site, diabetes and knee injury history was performed to examine the association of baseline AR levels with incident OA outcomes up to 60 months. Sensitivity analysis limiting incidence to 30-month follow-up was also performed.
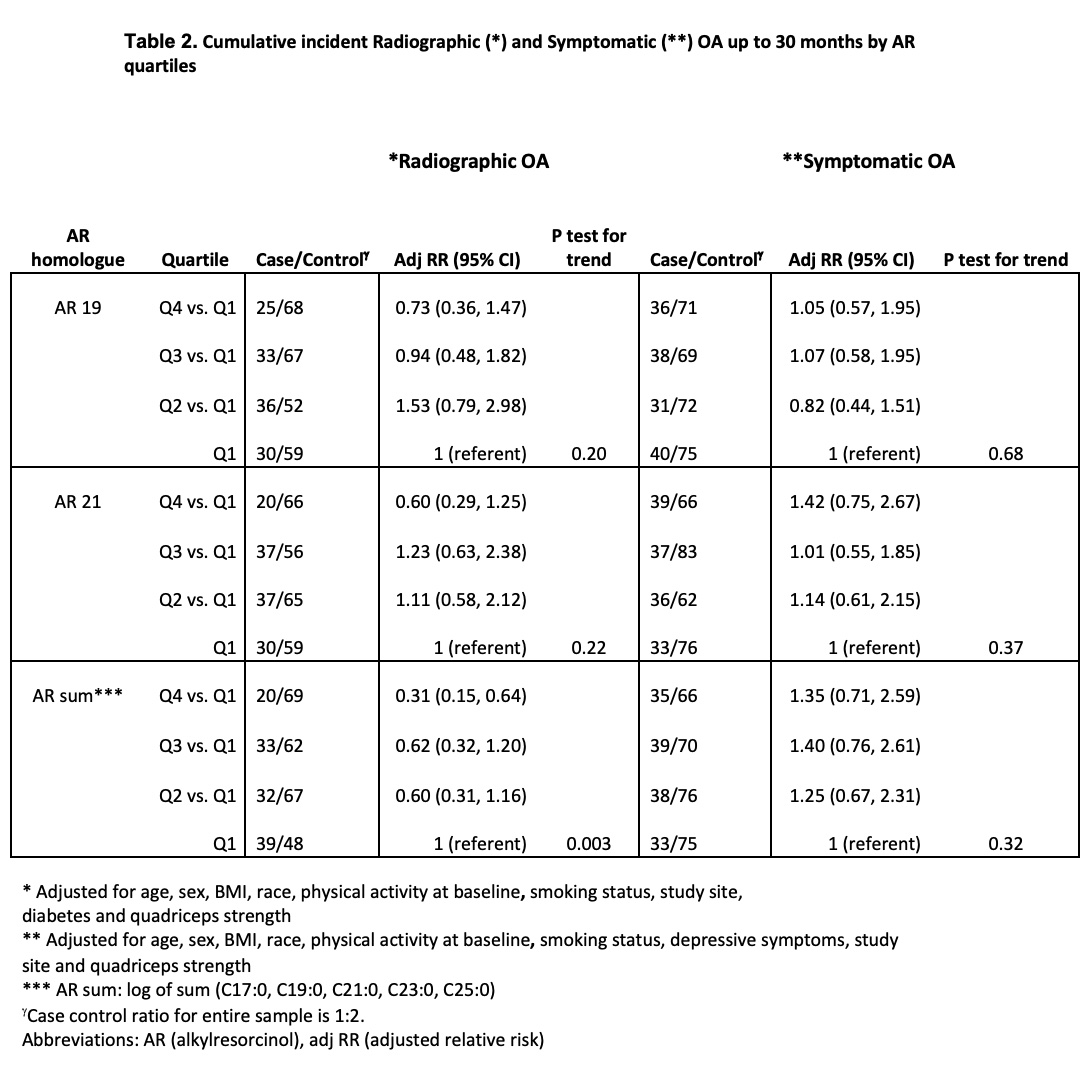
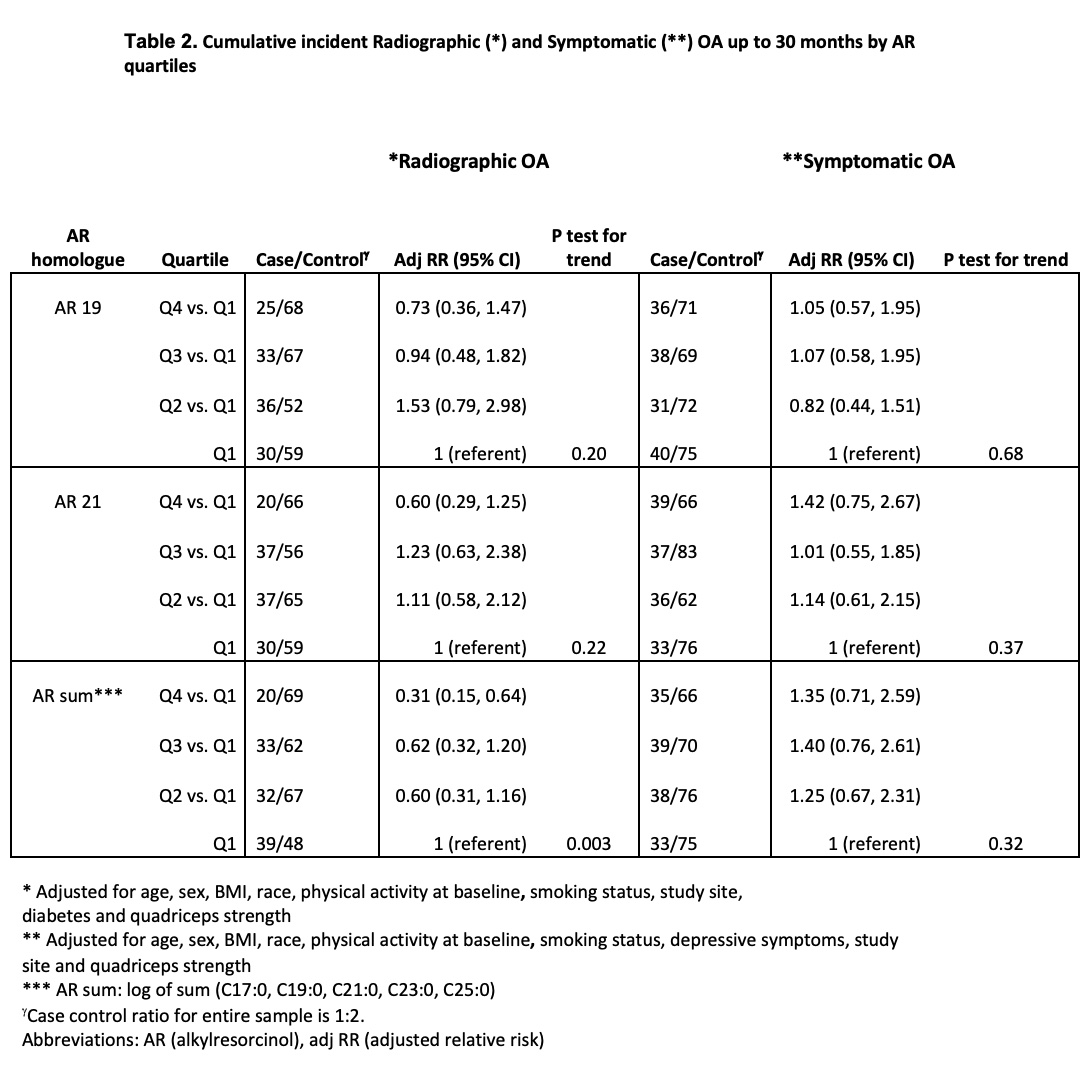
Results: There were similar numbers with incident x-ray OA and incident symptomatic OA (Table 1). No associations of baseline AR levels with 60-month outcomes were noted (figures 1a and 1b). However, we found a significant association between the AR sum (AR C17:0 through AR C25:0) levels and radiographic OA but not symptomatic OA at 30 months (Table 2). For each AR homologue, high levels protected against later radiographic OA (Table 2).
Conclusion: AR levels were not associated with incident OA up to 60 months; however, we found a significant association between AR sum and radiographic knee OA at 30 months. Our data suggests that increased whole grain fiber intake may lower the risk of OA. More evidence is necessary to clarify the association between fiber intake and OA outcomes.
.jpg)
Disclosures: J. Zertuche, None; G. Rabasa, None; A. Lichtenstein, None; N. Matthan, None; M. Nevitt, None; J. Torner, None; C. Lewis, None; D. Misra, None; D. Felson, None.
Background/Purpose: Whole grains, particularly wheat, are an important source of dietary fiber in the US. By providing a fermentable source, whole grains can modify the gut microbiome preventing and improving dysbiosis, and have been reported to protect against chronic disease, including incident symptomatic OA and worsening knee pain.
Alkylresorcinol (AR) (1,3-dihydroxy-5-n-alkylbenzene) is a phenolic lipid with five homologues (C17:0, C19:0, C21:0, C23:0, C25:0) found in high amounts in most whole grains. Plasma AR concentrations remain stable up to 3.9 years, making it a good biomarker of long-term whole grain intake. Biomarkers, as a proxy of dietary intake, can overcome misclassification of dietary exposure base on self-reported dietary intake.
We examined whether fasting AR levels of the predominant AR homologues (C19:0, C21:0), as well as the sum of C17:0 through C25:0, were associated with the development of OA.
Methods: Participants from the Multicenter Osteoarthritis study (MOST) at risk of developing or with knee OA were studied. Knee x-rays and knee symptoms were assessed at baseline and through a 60-month follow-up period. Aliquots of plasma stored at -80°C from the baseline visit were analyzed for AR homologues and total AR using an established (UPLC-QTOF-MS) method.
We carried out two nested case-control studies using risk-set sampling, one for incident radiographic OA (new onset KL >= grade 2) and one for incident symptomatic OA (combination of knee pain on most days + radiographic OA) and examined the relationship between baseline plasma ARs and incident OA at 60 months. Given individual's changing diets, we also tested baseline AR levels with 30-month OA outcomes.
Multivariable conditional logistic regression with covariates including age, sex, BMI, physical activity (using PASE 39), isokinetic quadriceps strength, smoking status, depressive symptoms (using CES-D scale), self-reported race, clinic site, diabetes and knee injury history was performed to examine the association of baseline AR levels with incident OA outcomes up to 60 months. Sensitivity analysis limiting incidence to 30-month follow-up was also performed.
Results: There were similar numbers with incident x-ray OA and incident symptomatic OA (Table 1). No associations of baseline AR levels with 60-month outcomes were noted (figures 1a and 1b). However, we found a significant association between the AR sum (AR C17:0 through AR C25:0) levels and radiographic OA but not symptomatic OA at 30 months (Table 2). For each AR homologue, high levels protected against later radiographic OA (Table 2).
Conclusion: AR levels were not associated with incident OA up to 60 months; however, we found a significant association between AR sum and radiographic knee OA at 30 months. Our data suggests that increased whole grain fiber intake may lower the risk of OA. More evidence is necessary to clarify the association between fiber intake and OA outcomes.
.jpg)
Disclosures: J. Zertuche, None; G. Rabasa, None; A. Lichtenstein, None; N. Matthan, None; M. Nevitt, None; J. Torner, None; C. Lewis, None; D. Misra, None; D. Felson, None.

