Back
Poster Session D
Myopathic rheumatic diseases (polymyositis, dermatomyositis, inclusion body myositis)
Session: (1856–1887) Muscle Biology, Myositis and Myopathies Poster II
1874: Autoantibodies Are Common in Patients with Idiopathic Interstitial Lung Disease Suggesting a High Prevalence of Undiagnosed Autoimmune Connective Tissue Disease
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- ST
Sarah Tansley, PhD, BSc, MBChB
University of Bath
Bath, United Kingdom
Abstract Poster Presenter(s)
Sarah Tansley1, Caroline Cotton2, Fionnuala McMorrow1, Hui Lu1, Aravinthan Loganathan1, Zoe Betteridge1, Robert New3, Lisa Spencer4, Neil McHugh1 and Robert Cooper4, 1University of Bath, Bath, United Kingdom, 2Liverpool University Hospital, Liverpool, United Kingdom, 3NCA, Manchester, 4University of Liverpool, Liverpool
Background/Purpose: In some patients, interstitial lung disease (ILD) may be the dominant or even sole overt manifestation of an otherwise unrecognised autoimmune connective tissue disease (CTD). Accurate diagnosis can be challenging given considerable overlap of the clinical, radiological and histological disease features. Distinguishing CTD related ILD from idiopathic ILD, enables appropriate immunosuppressive treatment, informs prognosis and facilitates monitoring for other CTD associated complications. Occasionally a lung biopsy may be necessary to ensure accurate diagnosis. Autoantibodies are a hallmark feature of CTD, are highly disease specific and their presence is strongly suggestive of covert CTD-ILD in selected populations. We investigated patients labelled as idiopathic ILD for the presence of autoantibodies that may suggest misdiagnosis.
Methods: The serum from three patient subgroups recruited to UK Biomarkers of Interstitial Lung Disease were analysed: 251 with idiopathic Pulmonary Fibrosis (IPF), 206 with idiopathic ILD and non-specific interstitial pneumonia on imaging (iNSIP) and 41 with idiopathic ILD and organising pneumonia on imaging, the later is also known as cryptogenic organising pneumonia (COP). ILD subtype was determined at a local level based on standard clinical assessments.
Autoantibody status was determined by K562 cell radio-immunoprecipitation.
Patient samples with an autoantibody detected by immunoprecipitation were also analysed by a relevant line immunoassay (Euroimmun Myositis research profile, ANA profile 5 or Nucleolar profile). Assays were performed according to manufacturers' instructions.
Results: CTD-autoantibodies were identified in 6% of patients overall but this varied significantly between ILD subgroups. Autoantibodies were rare in patients diagnosed with IPF but were a common finding in those with iNSIP and COP, see table. Autoantibodies identified included those readily detectable by routine testing in hospital laboratories e.g. anti-Jo1, in addition to rarer antibodies not included in most standard assays e.g. anti-Zo. Nearly half of all autoantibodies detected were anti-synthetase autoantibodies. The most common autoantibody identified was anti-PL12 which accounted for one third of all autoantibodies identified.
All autoantibodies identified by immunoprecipitation were detectable by commercial line immunoassay except for anti-KS and anti-OJ.
Conclusion: Covert-CTD is likely to be common amongst patients diagnosed with idiopathic ILD. More specific guidance on autoantibody testing and interpretation could improve autoantibody detection, facilitate accurate diagnosis, and ensure patients receive appropriate immunosuppressive treatment. Joint clinics between rheumatologists and ILD physicians may facilitate this.
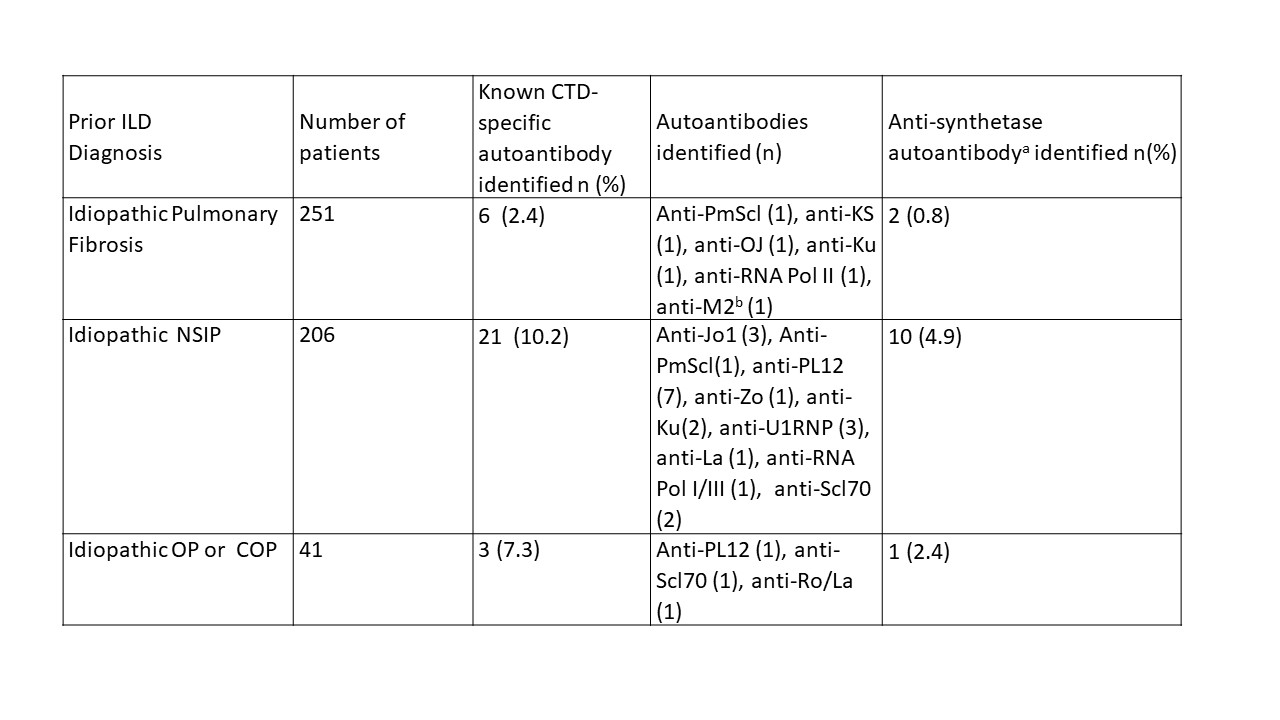 Table: The prevalence of CTD-specific autoantibodies in patients with a diagnosis of idiopathic interstitial lung disease
Table: The prevalence of CTD-specific autoantibodies in patients with a diagnosis of idiopathic interstitial lung disease
a. Anti-Jo 1, anti-PL7, anti-PL12, anti-OJ, anti-KS, anti-EJ, anti-Zo & anti-Ha
b. This patient has a known additional diagnosis of primary biliary cirrhosis
Disclosures: S. Tansley, None; C. Cotton, None; F. McMorrow, None; H. Lu, None; A. Loganathan, None; Z. Betteridge, Accord Healthcare; R. New, None; L. Spencer, None; N. McHugh, None; R. Cooper, None.
Background/Purpose: In some patients, interstitial lung disease (ILD) may be the dominant or even sole overt manifestation of an otherwise unrecognised autoimmune connective tissue disease (CTD). Accurate diagnosis can be challenging given considerable overlap of the clinical, radiological and histological disease features. Distinguishing CTD related ILD from idiopathic ILD, enables appropriate immunosuppressive treatment, informs prognosis and facilitates monitoring for other CTD associated complications. Occasionally a lung biopsy may be necessary to ensure accurate diagnosis. Autoantibodies are a hallmark feature of CTD, are highly disease specific and their presence is strongly suggestive of covert CTD-ILD in selected populations. We investigated patients labelled as idiopathic ILD for the presence of autoantibodies that may suggest misdiagnosis.
Methods: The serum from three patient subgroups recruited to UK Biomarkers of Interstitial Lung Disease were analysed: 251 with idiopathic Pulmonary Fibrosis (IPF), 206 with idiopathic ILD and non-specific interstitial pneumonia on imaging (iNSIP) and 41 with idiopathic ILD and organising pneumonia on imaging, the later is also known as cryptogenic organising pneumonia (COP). ILD subtype was determined at a local level based on standard clinical assessments.
Autoantibody status was determined by K562 cell radio-immunoprecipitation.
Patient samples with an autoantibody detected by immunoprecipitation were also analysed by a relevant line immunoassay (Euroimmun Myositis research profile, ANA profile 5 or Nucleolar profile). Assays were performed according to manufacturers' instructions.
Results: CTD-autoantibodies were identified in 6% of patients overall but this varied significantly between ILD subgroups. Autoantibodies were rare in patients diagnosed with IPF but were a common finding in those with iNSIP and COP, see table. Autoantibodies identified included those readily detectable by routine testing in hospital laboratories e.g. anti-Jo1, in addition to rarer antibodies not included in most standard assays e.g. anti-Zo. Nearly half of all autoantibodies detected were anti-synthetase autoantibodies. The most common autoantibody identified was anti-PL12 which accounted for one third of all autoantibodies identified.
All autoantibodies identified by immunoprecipitation were detectable by commercial line immunoassay except for anti-KS and anti-OJ.
Conclusion: Covert-CTD is likely to be common amongst patients diagnosed with idiopathic ILD. More specific guidance on autoantibody testing and interpretation could improve autoantibody detection, facilitate accurate diagnosis, and ensure patients receive appropriate immunosuppressive treatment. Joint clinics between rheumatologists and ILD physicians may facilitate this.
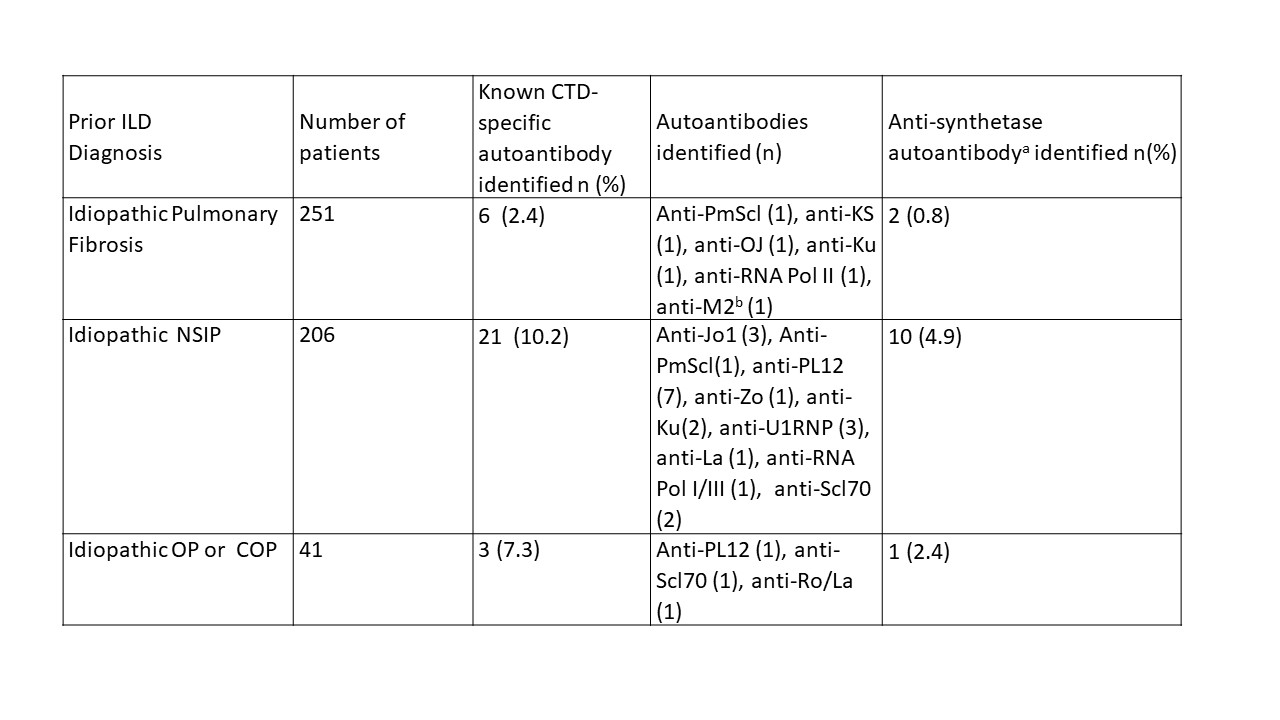 Table: The prevalence of CTD-specific autoantibodies in patients with a diagnosis of idiopathic interstitial lung disease
Table: The prevalence of CTD-specific autoantibodies in patients with a diagnosis of idiopathic interstitial lung diseasea. Anti-Jo 1, anti-PL7, anti-PL12, anti-OJ, anti-KS, anti-EJ, anti-Zo & anti-Ha
b. This patient has a known additional diagnosis of primary biliary cirrhosis
Disclosures: S. Tansley, None; C. Cotton, None; F. McMorrow, None; H. Lu, None; A. Loganathan, None; Z. Betteridge, Accord Healthcare; R. New, None; L. Spencer, None; N. McHugh, None; R. Cooper, None.

