Back
Ignite Talk
Session: Ignite Session 1A
0889: Serum Adipokines Predict Incident Osteoporotic Fracture in Patients with Rheumatoid Arthritis
Saturday, November 12, 2022
1:15 PM – 1:20 PM Eastern Time
Location: Northern Liberties Stage
Joshua Baker, MD, MS
University of Pennsylvania
Philadelphia, PA, United StatesDisclosure: Disclosure(s): No financial relationships with ineligible companies to disclose
Ignite Speaker(s)
Joshua Baker1, Katherine Wysham2, Bryant England3, Punyasha Roul4, Aleksander Lenert5, Grant Cannon6, Brian Sauer7, Geoffrey Thiele3 and Ted Mikuls8, 1University of Pennsylvania, Philadelphia, PA, 2VA Puget Sound/University of Washington, Seattle, WA, 3University of Nebraska Medical Center, Omaha, NE, 4UNMC, Omaha, NE, 5University of Iowa, Iowa City, IA, 6Retired, Salt Lake City, UT, 7Salt Lake City VA/University of Utah, Salt Lake City, UT, 8Division of Rheumatology, University of Nebraska Medical Center, Omaha, NE
Background/Purpose: Adipokines are fat and muscle-secreted protein hormones that regulate metabolism. Adiponectin has been associated with fracture in the general population while the role of leptin is less clear. Fibroblast Growth Factor (FGF)-21 is an indicator of metabolic stress has been associated adverse bone morphology and strength in other settings. We assessed whether adipokines are associated with a history of osteoporosis and fracture at time of enrollment in the Veteran’s Affairs Rheumatoid Arthritis (VARA) registry and whether they independently predict future incident fractures.
Methods: Participants were adults with physician-confirmed RA. Adipokines were measured on the MesoScale Discovery platform using banked serum from enrollment. Values were log-adjusted, standardized (per SD), and dichotomized above/below the median value. A history of osteoporosis and fracture were defined based on the presence of any relevant HCUP-CCS codes within the 12 months before enrollment. Incident osteoporotic fracture was defined based on validated algorithms using diagnostic and procedure codes and confirmed by chart review. Linear regression was used to evaluate differences in adipokines among those with a history of osteoporosis or fracture at enrollment. Multivariable Cox proportional hazard models evaluated associations between adipokines and incident fracture adjusting for demographics, smoking, BMI, prednisone use, comorbidity score, disease activity, and any history of osteoporosis and fracture prior to enrollment.
Results: A total of 2512 participants were included (mean (SD) age 71 (10) years; 87% male). At enrollment, 648 patients had a history of any prior fracture and 452 had a history of osteoporosis. Over 16,573 person-years of follow-up, there were 86 incident fractures at a rate of 0.52 per 100 person-years. After adjustment, those with a history of fracture at enrollment had higher adiponectin, leptin, and FGF-21 levels (Figure 1). In addition, those with a history of osteoporosis (with or without prior fracture) had higher levels of adiponectin and leptin. After adjustment, there was a higher risk of incident fracture among patients with adiponectin [HR: 1.43 (1.07, 1.90) p=0.01] and leptin [HR: 1.49 (1.11, 1.98) p=0.006] levels above the median. Patients with elevated levels of both adiponectin and leptin experienced a much higher risk of fracture compared to those in whom neither was elevated [HR: 2.14 (1.38, 3.33) p=0.001] (Figure 2).
Conclusion: Elevations in adipokines are independently associated with a greater prevalence of osteoporosis and fracture at enrollment and predict incident osteoporotic fractures in patients with RA. perhaps by identifying patients who have altered body composition or disrupted metabolic pathways. Further study is needed to determine how alterations in adipokines over time could be leveraged as part of a precision medicine approach with the goal of preventing fracture.
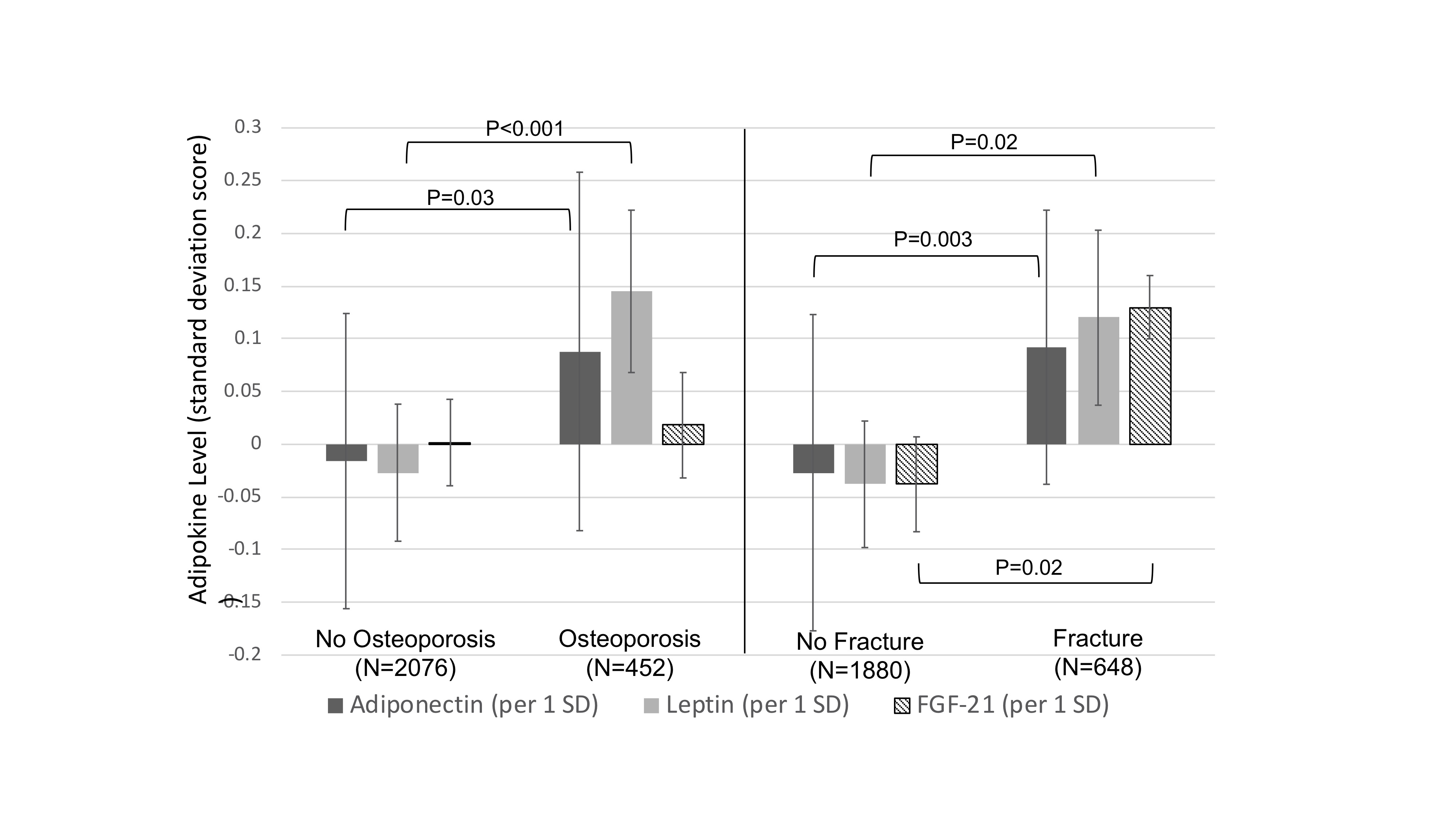 Figure 1: Adipokine levels by prevalent osteoporosis or history of fracture, at VARA enrollment adjusted for age, sex, race, BMI, DAS28, smoking, and prednisone use. Linear regression, adjusted for age, sex, race, BMI, smoking, prednisone use, DAS28, prednisone use, and comorbidity score (RDCI). Note: The RDCI was adjusted down 1 point for those with prevalent fracture. Abbreviations: SD=standard deviation
Figure 1: Adipokine levels by prevalent osteoporosis or history of fracture, at VARA enrollment adjusted for age, sex, race, BMI, DAS28, smoking, and prednisone use. Linear regression, adjusted for age, sex, race, BMI, smoking, prednisone use, DAS28, prednisone use, and comorbidity score (RDCI). Note: The RDCI was adjusted down 1 point for those with prevalent fracture. Abbreviations: SD=standard deviation
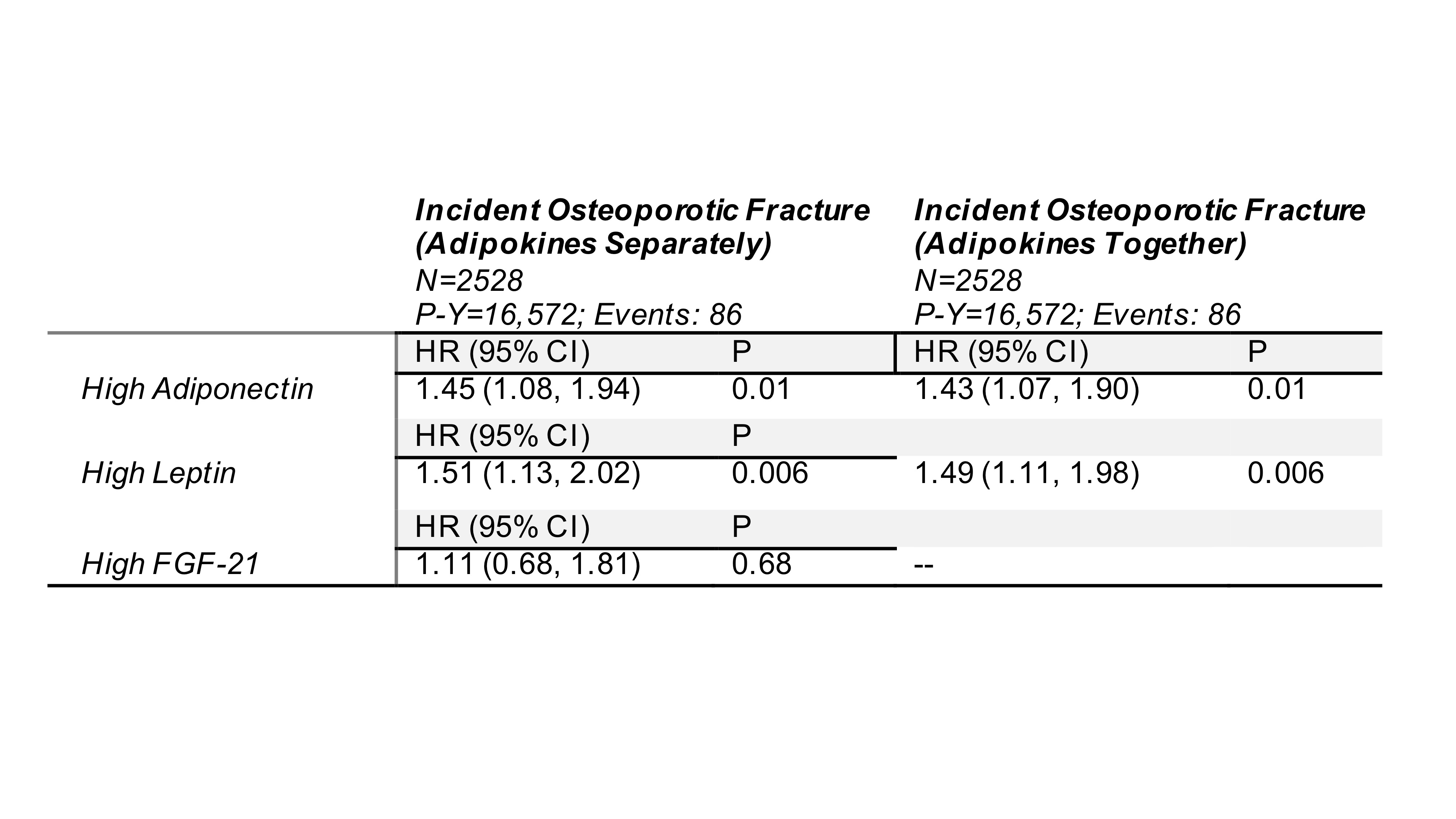 Table: Association between adipokines and incident fracture. In the left column, the result represents the effect for the exposure in three separate models. In the right column, adipokines were tested in the same model (if p < 0.1 when tested alone).
Table: Association between adipokines and incident fracture. In the left column, the result represents the effect for the exposure in three separate models. In the right column, adipokines were tested in the same model (if p < 0.1 when tested alone).
All models adjusted for age, age2, sex, race, BMI, smoking, history of osteoporosis, history of fracture, prior use of bisphosphonates, DAS28, prednisone use, comorbidity score (RDCI), and date of enrollment (and squared term). Note: The RDCI was adjusted down 1 point for those with prevalent fracture.
Abbreviations: P-Y= Person-years; HR= Hazard Ratio; CI= Confidence Interval; BMI= Body Mass Index; TNFi= Tumor Necrosis Factor Inhibitor
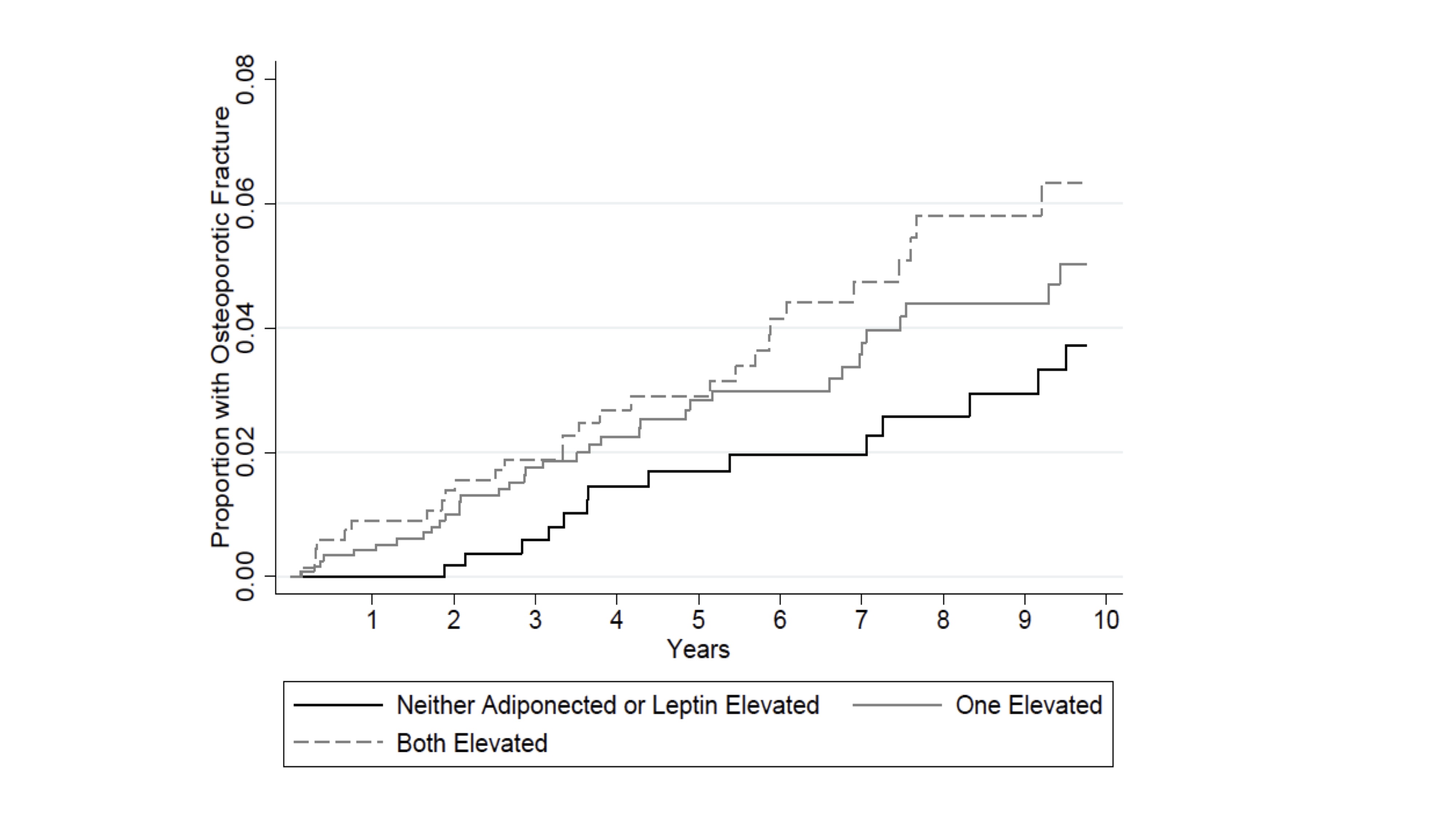 Figure 2: Cumulative probability of incident osteoporotic fracture by number of elevated adipokines (adiponectin/leptin) adjusted for age, sex, race, date enrolled, BMI, RDCI, smoking history, prednisone use, prior fracture, osteoporosis, prior bisphosphonate use, and baseline DAS28. Note: The RDCI was adjusted down 1 point for those with prevalent fracture.
Figure 2: Cumulative probability of incident osteoporotic fracture by number of elevated adipokines (adiponectin/leptin) adjusted for age, sex, race, date enrolled, BMI, RDCI, smoking history, prednisone use, prior fracture, osteoporosis, prior bisphosphonate use, and baseline DAS28. Note: The RDCI was adjusted down 1 point for those with prevalent fracture.
Disclosures: J. Baker, Bristol-Myers Squibb(BMS), RediTrex, Pfizer; K. Wysham, None; B. England, Boehringer-Ingelheim; P. Roul, None; A. Lenert, None; G. Cannon, None; B. Sauer, None; G. Thiele, None; T. Mikuls, Gilead Sciences, Bristol-Myers Squibb, Horizon, Sanofi, Pfizer Inc.
Background/Purpose: Adipokines are fat and muscle-secreted protein hormones that regulate metabolism. Adiponectin has been associated with fracture in the general population while the role of leptin is less clear. Fibroblast Growth Factor (FGF)-21 is an indicator of metabolic stress has been associated adverse bone morphology and strength in other settings. We assessed whether adipokines are associated with a history of osteoporosis and fracture at time of enrollment in the Veteran’s Affairs Rheumatoid Arthritis (VARA) registry and whether they independently predict future incident fractures.
Methods: Participants were adults with physician-confirmed RA. Adipokines were measured on the MesoScale Discovery platform using banked serum from enrollment. Values were log-adjusted, standardized (per SD), and dichotomized above/below the median value. A history of osteoporosis and fracture were defined based on the presence of any relevant HCUP-CCS codes within the 12 months before enrollment. Incident osteoporotic fracture was defined based on validated algorithms using diagnostic and procedure codes and confirmed by chart review. Linear regression was used to evaluate differences in adipokines among those with a history of osteoporosis or fracture at enrollment. Multivariable Cox proportional hazard models evaluated associations between adipokines and incident fracture adjusting for demographics, smoking, BMI, prednisone use, comorbidity score, disease activity, and any history of osteoporosis and fracture prior to enrollment.
Results: A total of 2512 participants were included (mean (SD) age 71 (10) years; 87% male). At enrollment, 648 patients had a history of any prior fracture and 452 had a history of osteoporosis. Over 16,573 person-years of follow-up, there were 86 incident fractures at a rate of 0.52 per 100 person-years. After adjustment, those with a history of fracture at enrollment had higher adiponectin, leptin, and FGF-21 levels (Figure 1). In addition, those with a history of osteoporosis (with or without prior fracture) had higher levels of adiponectin and leptin. After adjustment, there was a higher risk of incident fracture among patients with adiponectin [HR: 1.43 (1.07, 1.90) p=0.01] and leptin [HR: 1.49 (1.11, 1.98) p=0.006] levels above the median. Patients with elevated levels of both adiponectin and leptin experienced a much higher risk of fracture compared to those in whom neither was elevated [HR: 2.14 (1.38, 3.33) p=0.001] (Figure 2).
Conclusion: Elevations in adipokines are independently associated with a greater prevalence of osteoporosis and fracture at enrollment and predict incident osteoporotic fractures in patients with RA. perhaps by identifying patients who have altered body composition or disrupted metabolic pathways. Further study is needed to determine how alterations in adipokines over time could be leveraged as part of a precision medicine approach with the goal of preventing fracture.
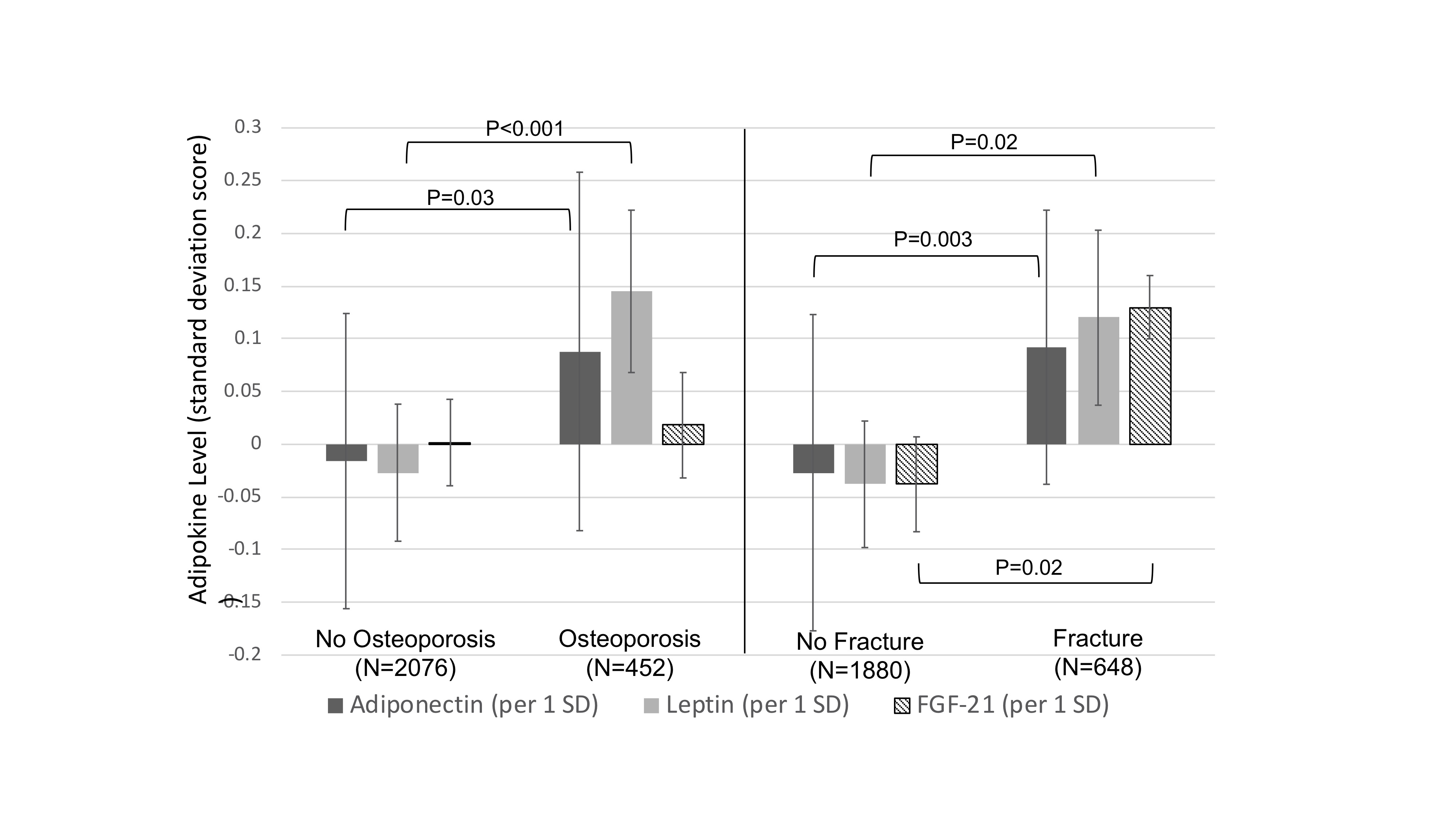 Figure 1: Adipokine levels by prevalent osteoporosis or history of fracture, at VARA enrollment adjusted for age, sex, race, BMI, DAS28, smoking, and prednisone use. Linear regression, adjusted for age, sex, race, BMI, smoking, prednisone use, DAS28, prednisone use, and comorbidity score (RDCI). Note: The RDCI was adjusted down 1 point for those with prevalent fracture. Abbreviations: SD=standard deviation
Figure 1: Adipokine levels by prevalent osteoporosis or history of fracture, at VARA enrollment adjusted for age, sex, race, BMI, DAS28, smoking, and prednisone use. Linear regression, adjusted for age, sex, race, BMI, smoking, prednisone use, DAS28, prednisone use, and comorbidity score (RDCI). Note: The RDCI was adjusted down 1 point for those with prevalent fracture. Abbreviations: SD=standard deviation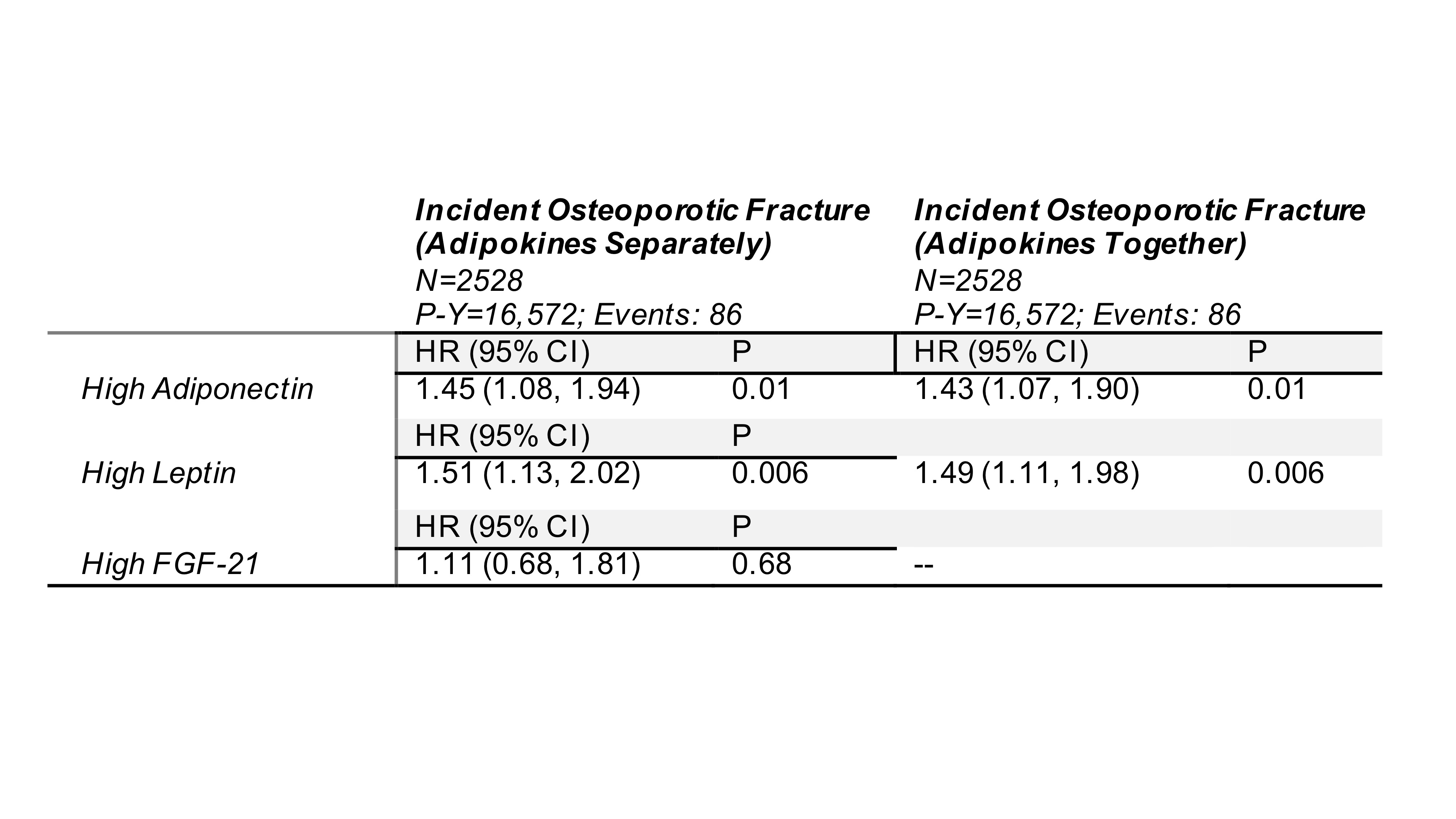 Table: Association between adipokines and incident fracture. In the left column, the result represents the effect for the exposure in three separate models. In the right column, adipokines were tested in the same model (if p < 0.1 when tested alone).
Table: Association between adipokines and incident fracture. In the left column, the result represents the effect for the exposure in three separate models. In the right column, adipokines were tested in the same model (if p < 0.1 when tested alone). All models adjusted for age, age2, sex, race, BMI, smoking, history of osteoporosis, history of fracture, prior use of bisphosphonates, DAS28, prednisone use, comorbidity score (RDCI), and date of enrollment (and squared term). Note: The RDCI was adjusted down 1 point for those with prevalent fracture.
Abbreviations: P-Y= Person-years; HR= Hazard Ratio; CI= Confidence Interval; BMI= Body Mass Index; TNFi= Tumor Necrosis Factor Inhibitor
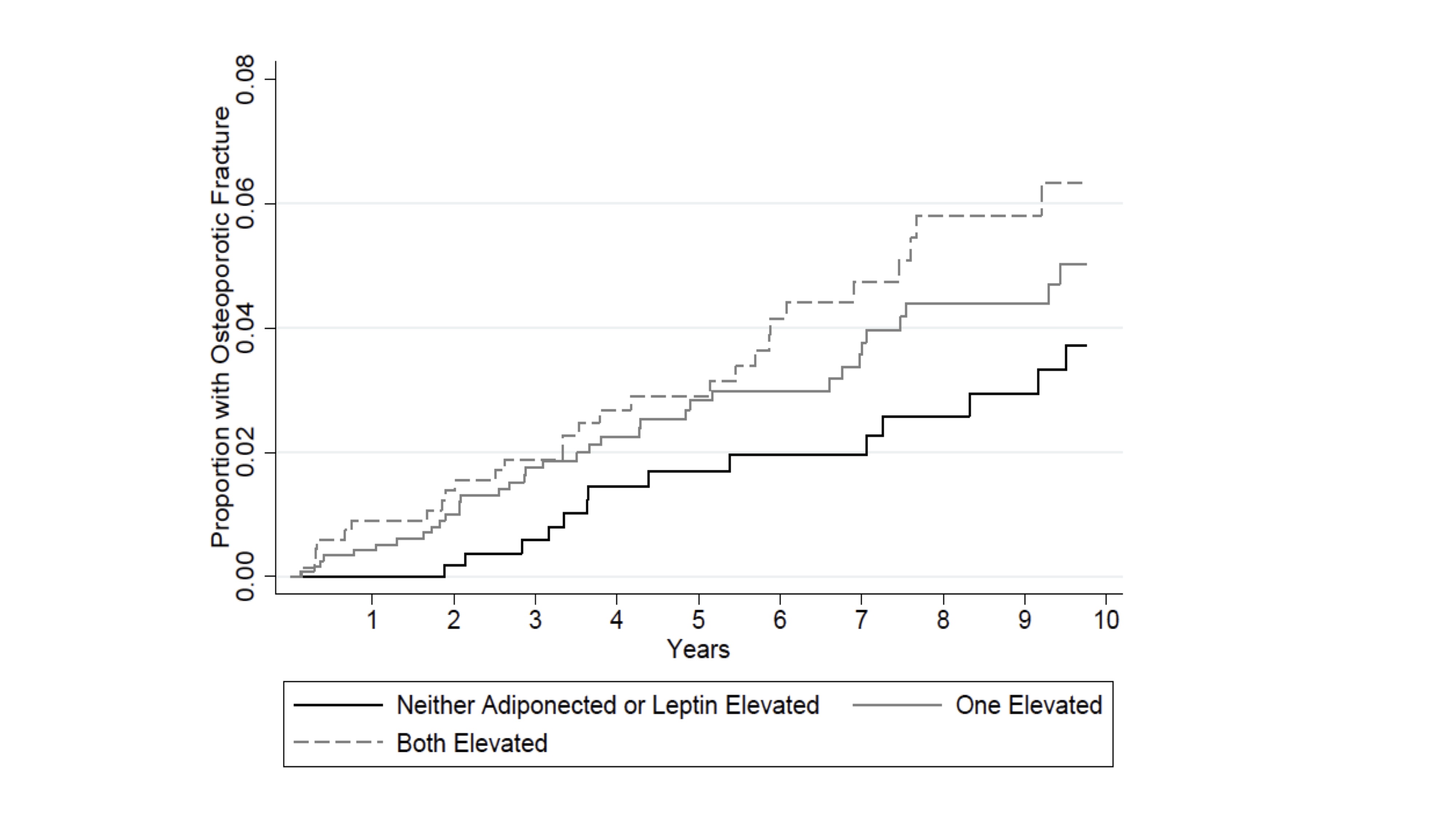 Figure 2: Cumulative probability of incident osteoporotic fracture by number of elevated adipokines (adiponectin/leptin) adjusted for age, sex, race, date enrolled, BMI, RDCI, smoking history, prednisone use, prior fracture, osteoporosis, prior bisphosphonate use, and baseline DAS28. Note: The RDCI was adjusted down 1 point for those with prevalent fracture.
Figure 2: Cumulative probability of incident osteoporotic fracture by number of elevated adipokines (adiponectin/leptin) adjusted for age, sex, race, date enrolled, BMI, RDCI, smoking history, prednisone use, prior fracture, osteoporosis, prior bisphosphonate use, and baseline DAS28. Note: The RDCI was adjusted down 1 point for those with prevalent fracture.Disclosures: J. Baker, Bristol-Myers Squibb(BMS), RediTrex, Pfizer; K. Wysham, None; B. England, Boehringer-Ingelheim; P. Roul, None; A. Lenert, None; G. Cannon, None; B. Sauer, None; G. Thiele, None; T. Mikuls, Gilead Sciences, Bristol-Myers Squibb, Horizon, Sanofi, Pfizer Inc.

