Back
Poster Session D
Session: (1924–1949) Pediatric Rheumatology – Clinical Poster III: Other
1925: Characterizing Phenotypic Changes by SARS-CoV-2 Variant in Multisystem Inflammatory Syndrome in Children (MIS-C): A Single Institution Case Series
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- EL
Emma Leisinger, BS
University of Iowa
Iowa City, IA, United States
Abstract Poster Presenter(s)
Sandy D. Hong1 and Emma Leisinger2, 1University of Iowa Stead Family Children's Hospital, Iowa City, IA, 2University of Iowa, Iowa City, IA
Background/Purpose: Multisystem inflammatory syndrome in children (MIS-C) is a severe hyper-inflammatory condition associated with a recent SARS-CoV-2 infection. Case reports began in April of 2020 from Italy and the United Kingdom documenting cases of children with shock-like illness and features of Kawasaki Disease (KD). Epidemiologic data demonstrates a latent rise and peak of MIS-C cases approximately 2-4 weeks after peak population infection. This study evaluated the phenotypic presentations of children diagnosed with MIS-C compared with the dominant SARS-CoV-2 variant type in the population throughout the course of the pandemic.
Methods: A retrospective chart reviews was performed on patients treated for MIS-C at the University of Iowa Stead Family Children's Hospital (UISFCH) from April 2020 to April 2022. Phenotyping was based on main clinical features at presentation. All patients met CDC guidelines for MIS-C. Variant category was determined by State of Iowa Department of Public Health data outlining the dominant variant by in state testing. The original strain indicates the time for which variant testing was not available at the state level. (See figure 1) Patient classification based on presenting features fell within 5 phenotypes; those with gastrointestinal involvement either fit criteria for mixed-abdominal or shock phenotypes, and those with dermatological features were characterized as KD-like or mixed-rash phenotypes. Patients with respiratory features were categorized as respiratory phenotype. (See Figure 2)
Results: Seventy children with median age of 8 (interquartile range (IQR) 0.58-19) years met the criteria for MIS-C. 28 patients (40%) were characterized as shock phenotype, 20 patients (29%) KD-like, 15 patients (21%) mixed abdominal, 6 patients (9%) mixed rash, and 1 patient (1%) respiratory. The phenotypic breakdown per SARS-CoV-2 variant showed that during the delta variant patients with gastrointestinal involvement with and without shock were the dominant phenotype at 70% (17/22) with 75% (13/17) of those being patients having shock. A Fisher's Exact Test comparing the gastrointestinal versus dermatologic phenotypes by variant yielded a p-value of 0.229.
Conclusion: Patients diagnosed with MIS-C during the time frame of the original, and alpha strain presented with similar amounts of gastrointestinal and dermatologic features, but as new variants emerged, it was evident that the phenotype proportions shifted. During the delta strain the majority of patients presented with gastrointestinal involvement and shock. We demonstrate the rise of MIS-C after population peaks in the original and delta strain, and a distinctive lack of cases following the surge of the omicron strain. The lack of a peak may be due to omicron causing less immune activation, previous infection in our pediatric population, and the effect of vaccination.
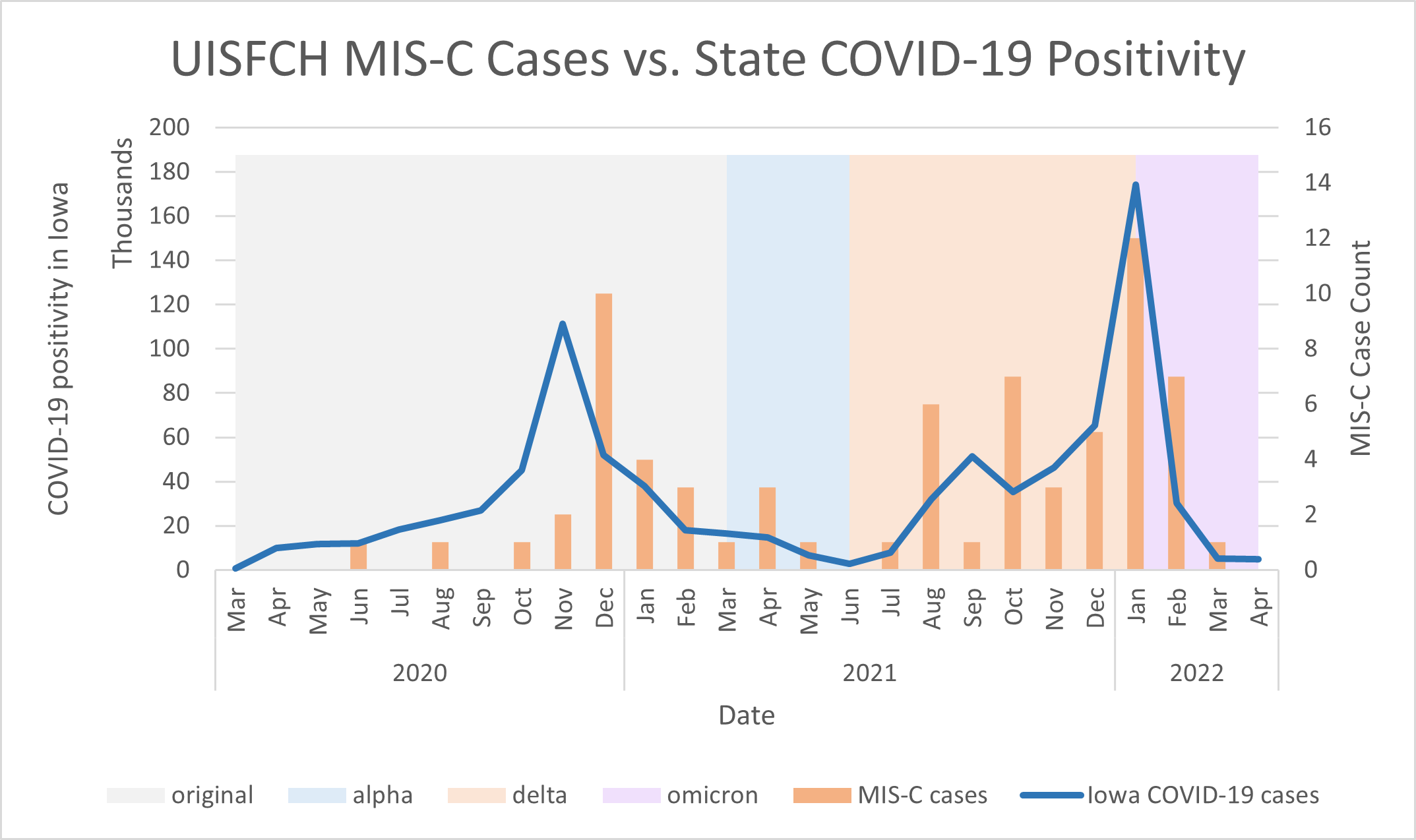 Figure 1: MIS-C case count per month was compared with positive tests (in thousands) over the course of the pandemic. Background coloring indicates the dominant SARS-CoV-2 variant in the state of Iowa. Original variant (grey) outlines the time in which state testing for variant type was not readily available.
Figure 1: MIS-C case count per month was compared with positive tests (in thousands) over the course of the pandemic. Background coloring indicates the dominant SARS-CoV-2 variant in the state of Iowa. Original variant (grey) outlines the time in which state testing for variant type was not readily available.
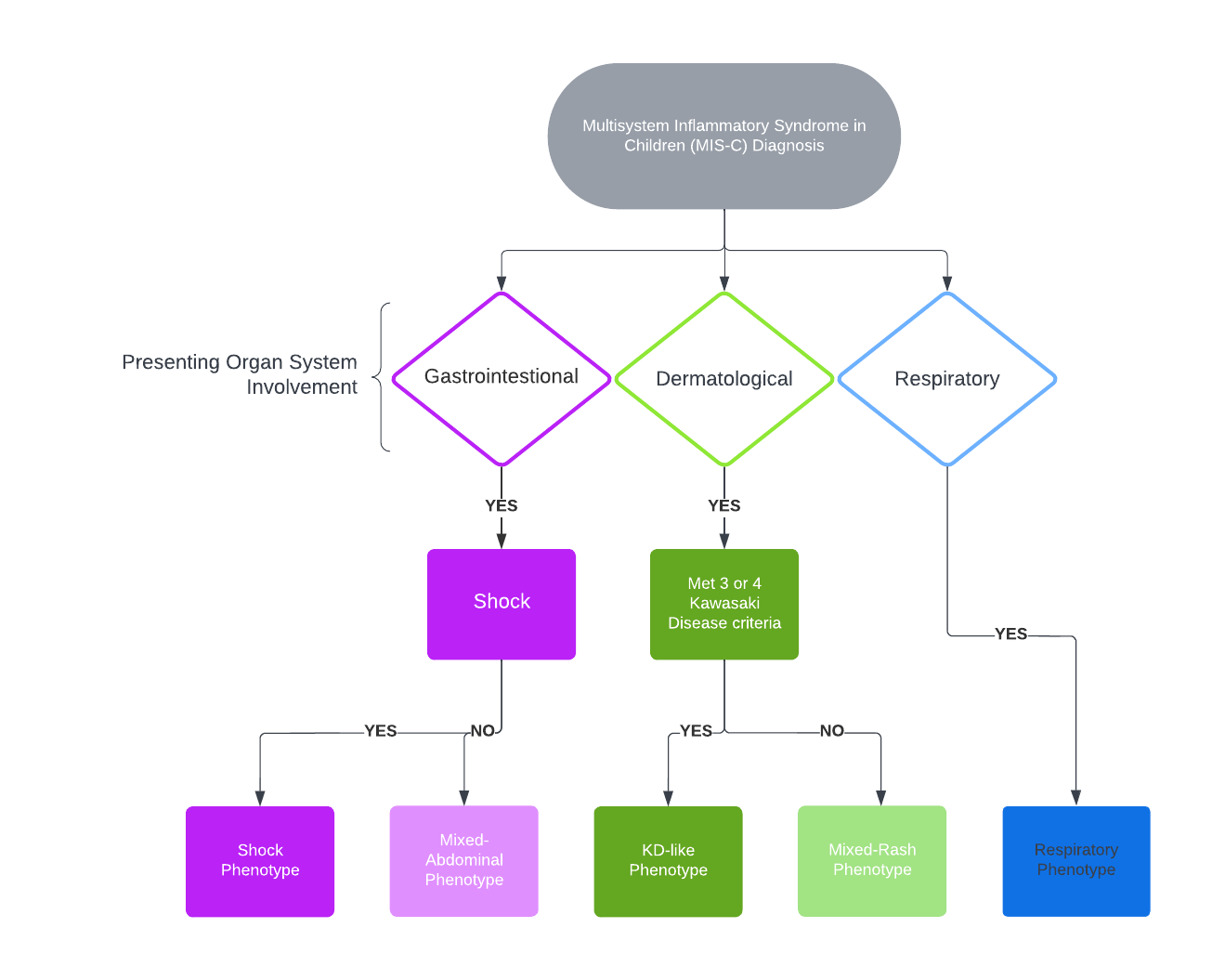 Figure 2: Flow diagram outlining classification of phenotype based on presenting organ system involvement. All patients met MIS-C criteria. Gastrointestinal involvement included abdominal pain, nausea, vomiting, and diarrhea. Dermatologic involvement included conjunctivitis muco-cutaneous changes, periorbital edema, erythema of hands and feet and morbilliform rashes. KD criteria was based on the AHA KD 2017 Guidelines.
Figure 2: Flow diagram outlining classification of phenotype based on presenting organ system involvement. All patients met MIS-C criteria. Gastrointestinal involvement included abdominal pain, nausea, vomiting, and diarrhea. Dermatologic involvement included conjunctivitis muco-cutaneous changes, periorbital edema, erythema of hands and feet and morbilliform rashes. KD criteria was based on the AHA KD 2017 Guidelines.
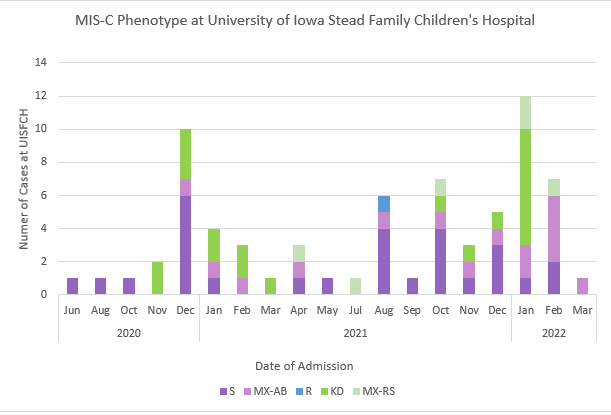 Figure 3: Cases of MIS-C admitted at UISFCH over the course of the pandemic displayed in admissions per month. Patients were categorically colored based on phenotype. Purple coloring indicates gastrointestinal involvement; patients with shock in dark purple and mixed-abdominal (no shock) in light purple. Green coloring indicated dermatologic features with those meeting criteria for KD or incomplete KD in dark green and those not meeting criteria but having prominent rash categorized as mixed rash in light green. Blue coloring indicated the respiratory phenotype.
Figure 3: Cases of MIS-C admitted at UISFCH over the course of the pandemic displayed in admissions per month. Patients were categorically colored based on phenotype. Purple coloring indicates gastrointestinal involvement; patients with shock in dark purple and mixed-abdominal (no shock) in light purple. Green coloring indicated dermatologic features with those meeting criteria for KD or incomplete KD in dark green and those not meeting criteria but having prominent rash categorized as mixed rash in light green. Blue coloring indicated the respiratory phenotype.
Disclosures: S. Hong, None; E. Leisinger, None.
Background/Purpose: Multisystem inflammatory syndrome in children (MIS-C) is a severe hyper-inflammatory condition associated with a recent SARS-CoV-2 infection. Case reports began in April of 2020 from Italy and the United Kingdom documenting cases of children with shock-like illness and features of Kawasaki Disease (KD). Epidemiologic data demonstrates a latent rise and peak of MIS-C cases approximately 2-4 weeks after peak population infection. This study evaluated the phenotypic presentations of children diagnosed with MIS-C compared with the dominant SARS-CoV-2 variant type in the population throughout the course of the pandemic.
Methods: A retrospective chart reviews was performed on patients treated for MIS-C at the University of Iowa Stead Family Children's Hospital (UISFCH) from April 2020 to April 2022. Phenotyping was based on main clinical features at presentation. All patients met CDC guidelines for MIS-C. Variant category was determined by State of Iowa Department of Public Health data outlining the dominant variant by in state testing. The original strain indicates the time for which variant testing was not available at the state level. (See figure 1) Patient classification based on presenting features fell within 5 phenotypes; those with gastrointestinal involvement either fit criteria for mixed-abdominal or shock phenotypes, and those with dermatological features were characterized as KD-like or mixed-rash phenotypes. Patients with respiratory features were categorized as respiratory phenotype. (See Figure 2)
Results: Seventy children with median age of 8 (interquartile range (IQR) 0.58-19) years met the criteria for MIS-C. 28 patients (40%) were characterized as shock phenotype, 20 patients (29%) KD-like, 15 patients (21%) mixed abdominal, 6 patients (9%) mixed rash, and 1 patient (1%) respiratory. The phenotypic breakdown per SARS-CoV-2 variant showed that during the delta variant patients with gastrointestinal involvement with and without shock were the dominant phenotype at 70% (17/22) with 75% (13/17) of those being patients having shock. A Fisher's Exact Test comparing the gastrointestinal versus dermatologic phenotypes by variant yielded a p-value of 0.229.
Conclusion: Patients diagnosed with MIS-C during the time frame of the original, and alpha strain presented with similar amounts of gastrointestinal and dermatologic features, but as new variants emerged, it was evident that the phenotype proportions shifted. During the delta strain the majority of patients presented with gastrointestinal involvement and shock. We demonstrate the rise of MIS-C after population peaks in the original and delta strain, and a distinctive lack of cases following the surge of the omicron strain. The lack of a peak may be due to omicron causing less immune activation, previous infection in our pediatric population, and the effect of vaccination.
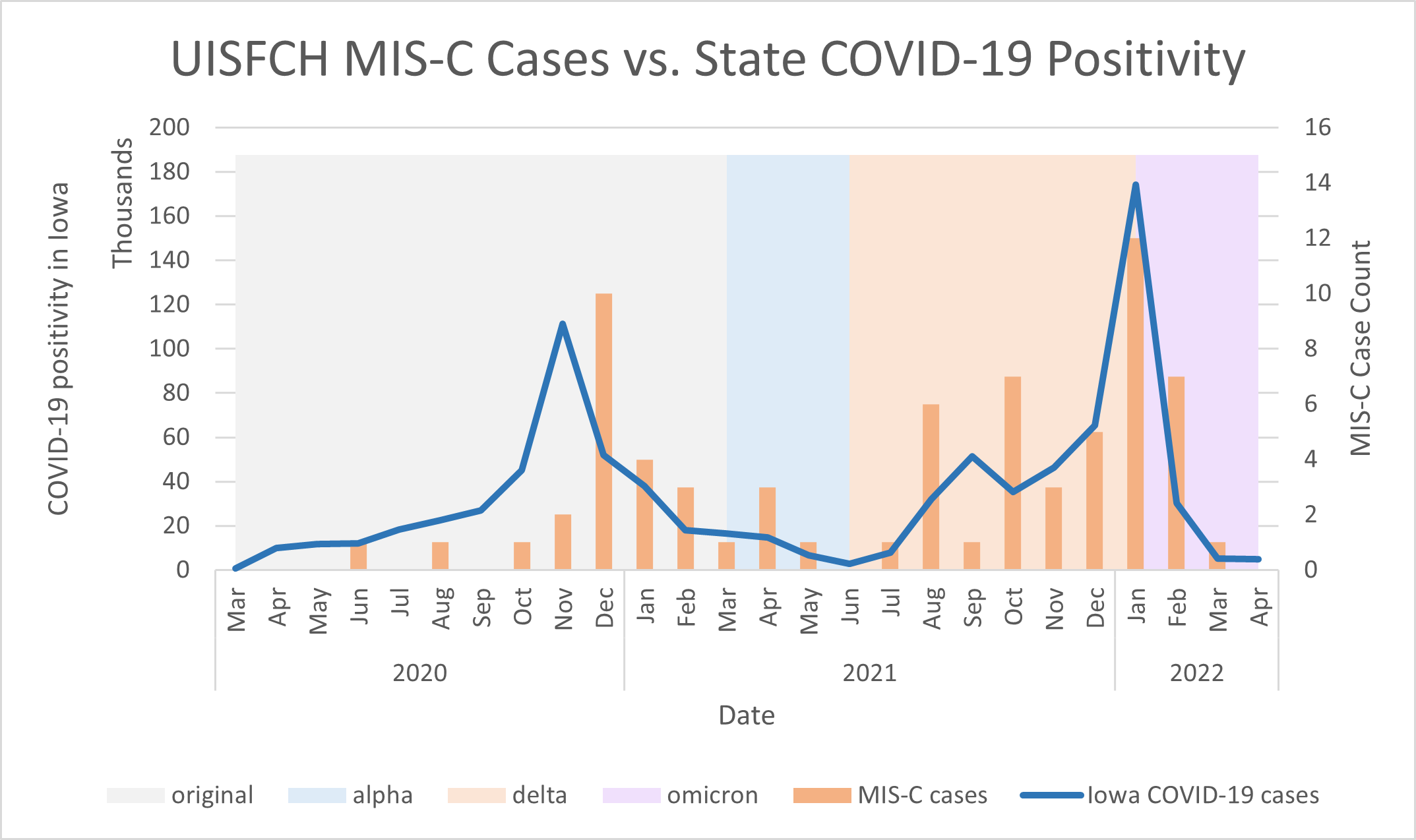 Figure 1: MIS-C case count per month was compared with positive tests (in thousands) over the course of the pandemic. Background coloring indicates the dominant SARS-CoV-2 variant in the state of Iowa. Original variant (grey) outlines the time in which state testing for variant type was not readily available.
Figure 1: MIS-C case count per month was compared with positive tests (in thousands) over the course of the pandemic. Background coloring indicates the dominant SARS-CoV-2 variant in the state of Iowa. Original variant (grey) outlines the time in which state testing for variant type was not readily available. 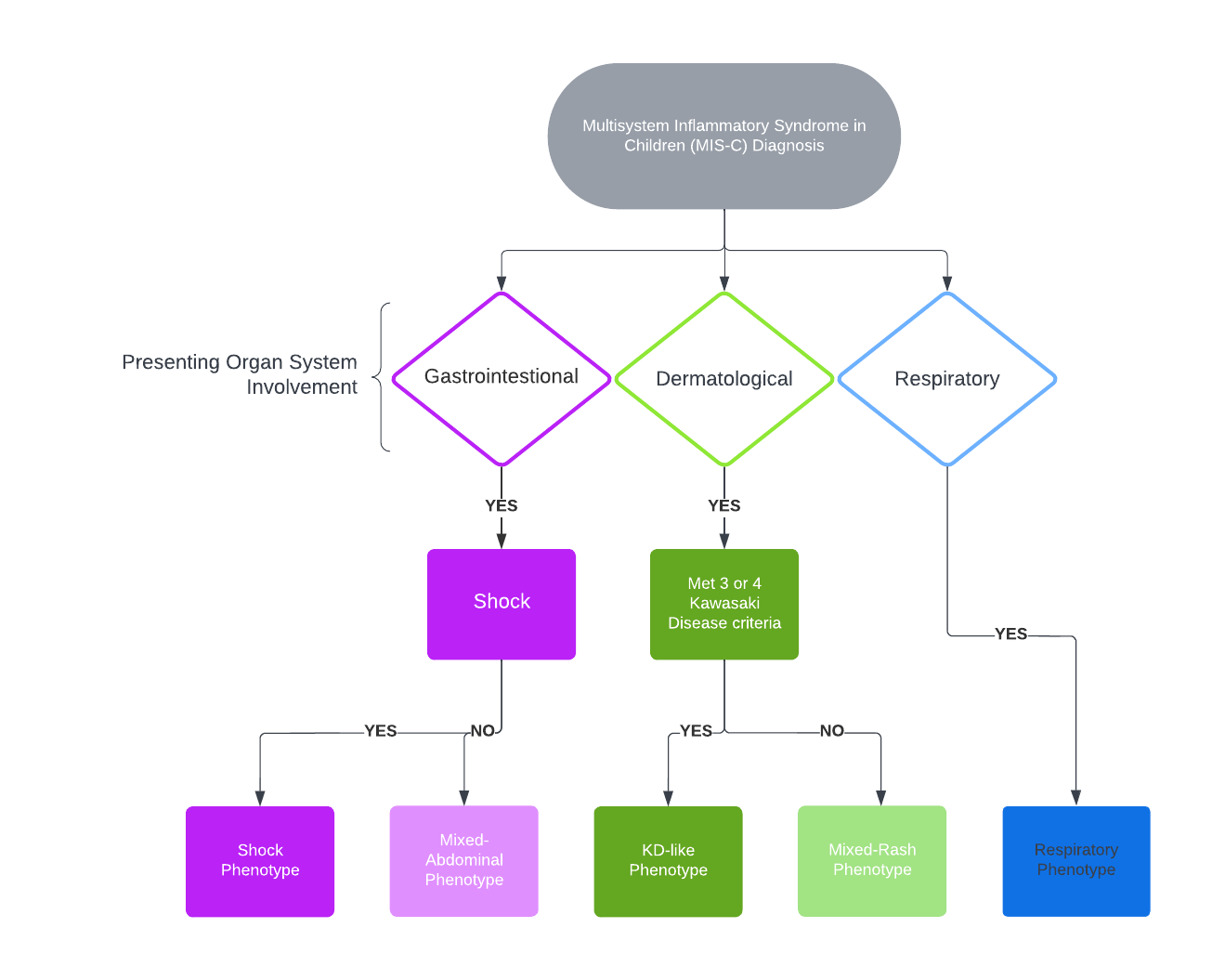 Figure 2: Flow diagram outlining classification of phenotype based on presenting organ system involvement. All patients met MIS-C criteria. Gastrointestinal involvement included abdominal pain, nausea, vomiting, and diarrhea. Dermatologic involvement included conjunctivitis muco-cutaneous changes, periorbital edema, erythema of hands and feet and morbilliform rashes. KD criteria was based on the AHA KD 2017 Guidelines.
Figure 2: Flow diagram outlining classification of phenotype based on presenting organ system involvement. All patients met MIS-C criteria. Gastrointestinal involvement included abdominal pain, nausea, vomiting, and diarrhea. Dermatologic involvement included conjunctivitis muco-cutaneous changes, periorbital edema, erythema of hands and feet and morbilliform rashes. KD criteria was based on the AHA KD 2017 Guidelines.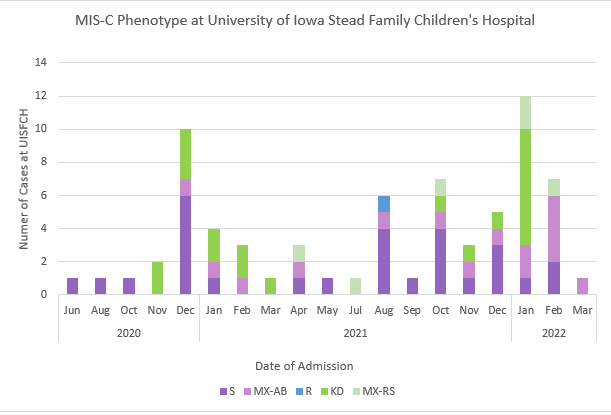 Figure 3: Cases of MIS-C admitted at UISFCH over the course of the pandemic displayed in admissions per month. Patients were categorically colored based on phenotype. Purple coloring indicates gastrointestinal involvement; patients with shock in dark purple and mixed-abdominal (no shock) in light purple. Green coloring indicated dermatologic features with those meeting criteria for KD or incomplete KD in dark green and those not meeting criteria but having prominent rash categorized as mixed rash in light green. Blue coloring indicated the respiratory phenotype.
Figure 3: Cases of MIS-C admitted at UISFCH over the course of the pandemic displayed in admissions per month. Patients were categorically colored based on phenotype. Purple coloring indicates gastrointestinal involvement; patients with shock in dark purple and mixed-abdominal (no shock) in light purple. Green coloring indicated dermatologic features with those meeting criteria for KD or incomplete KD in dark green and those not meeting criteria but having prominent rash categorized as mixed rash in light green. Blue coloring indicated the respiratory phenotype. Disclosures: S. Hong, None; E. Leisinger, None.

