Back
Poster Session D
Session: (2052–2107) SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
2083: A Network Meta-analysis on 532 SLE Patients: Low Complement Levels in the First Trimester Predict Disease Flare in Pregnancy
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SS
Savino Sciascia, MD
University of Turin
Torino, Turin, Italy
Abstract Poster Presenter(s)
Massimo Radin1, Irene Cecchi2, Francesca Crisafulli3, Evandro Mendes Klumb4, Guilherme Ramires De Jesús4, Miguel Ángel Saavedra5, Geraldine Vanessa Reyes-Navarro6, Luca iaccarino7, Maddalena Larosa7, Gabriella Moroni8, Francesco Tamborini9, dario Roccatello1, Laura Andreoli3, Cecilia Beatrice Chighizola10 and Savino Sciascia2, 1University of Turin, Turin, Italy, 2University of Turin, Torino, Italy, 3University of Brescia, Brescia, Italy, 4Instituto Fernandes Figueira, Rio De Janeiro, Brazil, 5Hospital de Especialidades Dr. Antonio Fraga Mouret, Ciudad de México, Mexico, 6Benemérita Universidad Autónoma de Puebla, Puebla, Mexico, 7University of Padova, Padova, Italy, 8Humanitas University, Rozzano, Italy, 9Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Milano, Italy, 10University of Milan, Milano, Italy
Background/Purpose: The complement system is a key-player in the pathogenesis of systemic lupus erythematosus (SLE); decrease in C3 and C4 levels correlates with disease activity and precedes clinically evident flare. Since synthesis of complement proteins increase during gestational course, it is debated whether complement levels exert a prognostic role in pregnant women with SLE.
We performed a network meta-analysis to assess the prognostic role of complement in pregnant SLE women, to evaluate the possible role of complement fluctuations during pregnancies.
Methods: Data from available prospective studies (Jan 2002-Dec 2020) investigating pregnancies in at least 50 SLE patients, excluding miscarriages before 12 weeks, werepooled together. After a systematic literature search, corresponding authors of 19 retrieved studies meetinginclusion criteria were invited to contribute with additional data, including complement C3 and C4 levels [6 months before pregnancy, at conception, 1st trimester (T1), 2nd trimester (T2), 3rd trimester (T3) and 3 months after delivery].
Results: A total of 532 SLE women from four eligible studies were included in the analysis [1-4]. Lupus Nephritis (LN) was diagnosed in 237 patients (44.5%) and Antiphospholipid Syndrome in 68 (12.8%). A total of 170 patients (32%) experienced a flare during pregnancy, defined as need of new Immunosuppressants or increase of prednisone > 9 mg/day.
Patients with LN had significantly lower mean levels of complement (C3 at conception; C3 at T1; C3 after 3 months of delivery; C4 at all timepoints except for C4 at T3). SLE patients who experienced flares during pregnancy had significantly lower mean levels of complement (all timepoints for both C3 and C4). Table 1 shows the mean C3 and C4 levels in different timepoints according to diagnosis and flare during pregnancy. Pregnancies with flare had a higher rate of maternal of fetal complications (60% vs.50.3%;p=0.03). The lowest levels of complement were observed in patients with a concomitant diagnosis of LN and presence of flare, particularly during theT1 (Figure 1). Nevertheless, both in LN and flare groups the lowest levels of C3 and C4 were documented at T1.
Conclusion: In this prospective large cohort of SLE patients low C3/C4 levels, particularly in T1, were associated with a higher frequency of flare. Lowering levels of complement, especially in T1, even within normal range might alert the treating clinicians in predicting disease course and consequently avoid flares, especially in LN.
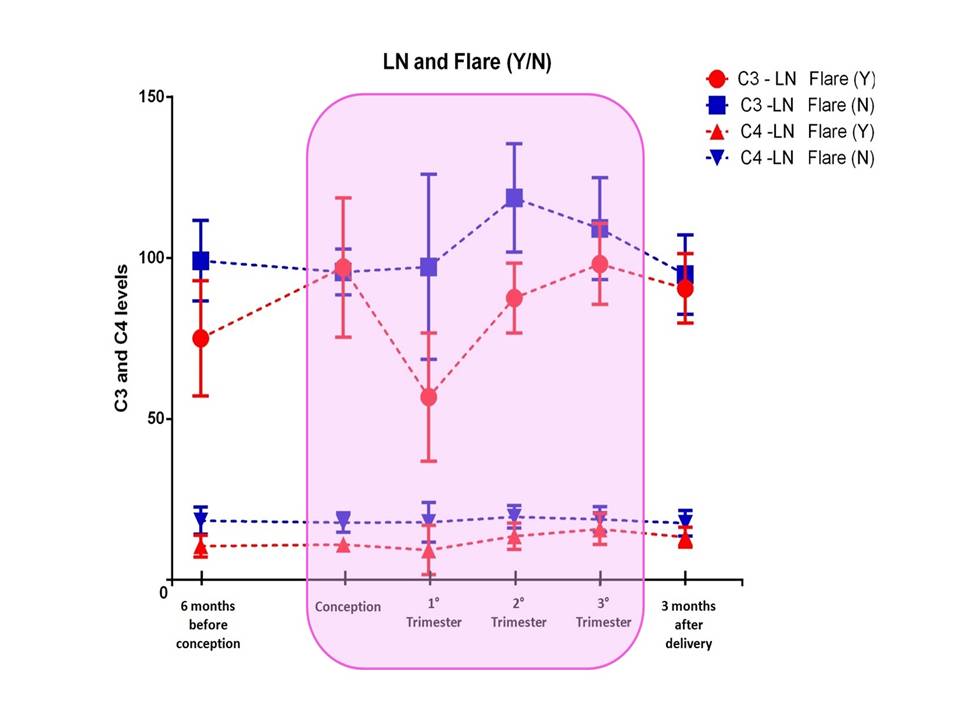 Figure 1. Complement Levels during time in patients with Lupus Nephritis and presence, or absence, of flare during pregnancy.
Figure 1. Complement Levels during time in patients with Lupus Nephritis and presence, or absence, of flare during pregnancy.
Disclosures: M. Radin, None; I. Cecchi, None; F. Crisafulli, None; E. Klumb, None; G. De Jesús, None; M. Saavedra, None; G. Reyes-Navarro, None; L. iaccarino, None; M. Larosa, None; G. Moroni, None; F. Tamborini, None; d. Roccatello, None; L. Andreoli, None; C. Chighizola, None; S. Sciascia, None.
Background/Purpose: The complement system is a key-player in the pathogenesis of systemic lupus erythematosus (SLE); decrease in C3 and C4 levels correlates with disease activity and precedes clinically evident flare. Since synthesis of complement proteins increase during gestational course, it is debated whether complement levels exert a prognostic role in pregnant women with SLE.
We performed a network meta-analysis to assess the prognostic role of complement in pregnant SLE women, to evaluate the possible role of complement fluctuations during pregnancies.
Methods: Data from available prospective studies (Jan 2002-Dec 2020) investigating pregnancies in at least 50 SLE patients, excluding miscarriages before 12 weeks, werepooled together. After a systematic literature search, corresponding authors of 19 retrieved studies meetinginclusion criteria were invited to contribute with additional data, including complement C3 and C4 levels [6 months before pregnancy, at conception, 1st trimester (T1), 2nd trimester (T2), 3rd trimester (T3) and 3 months after delivery].
Results: A total of 532 SLE women from four eligible studies were included in the analysis [1-4]. Lupus Nephritis (LN) was diagnosed in 237 patients (44.5%) and Antiphospholipid Syndrome in 68 (12.8%). A total of 170 patients (32%) experienced a flare during pregnancy, defined as need of new Immunosuppressants or increase of prednisone > 9 mg/day.
Patients with LN had significantly lower mean levels of complement (C3 at conception; C3 at T1; C3 after 3 months of delivery; C4 at all timepoints except for C4 at T3). SLE patients who experienced flares during pregnancy had significantly lower mean levels of complement (all timepoints for both C3 and C4). Table 1 shows the mean C3 and C4 levels in different timepoints according to diagnosis and flare during pregnancy. Pregnancies with flare had a higher rate of maternal of fetal complications (60% vs.50.3%;p=0.03). The lowest levels of complement were observed in patients with a concomitant diagnosis of LN and presence of flare, particularly during theT1 (Figure 1). Nevertheless, both in LN and flare groups the lowest levels of C3 and C4 were documented at T1.
Conclusion: In this prospective large cohort of SLE patients low C3/C4 levels, particularly in T1, were associated with a higher frequency of flare. Lowering levels of complement, especially in T1, even within normal range might alert the treating clinicians in predicting disease course and consequently avoid flares, especially in LN.
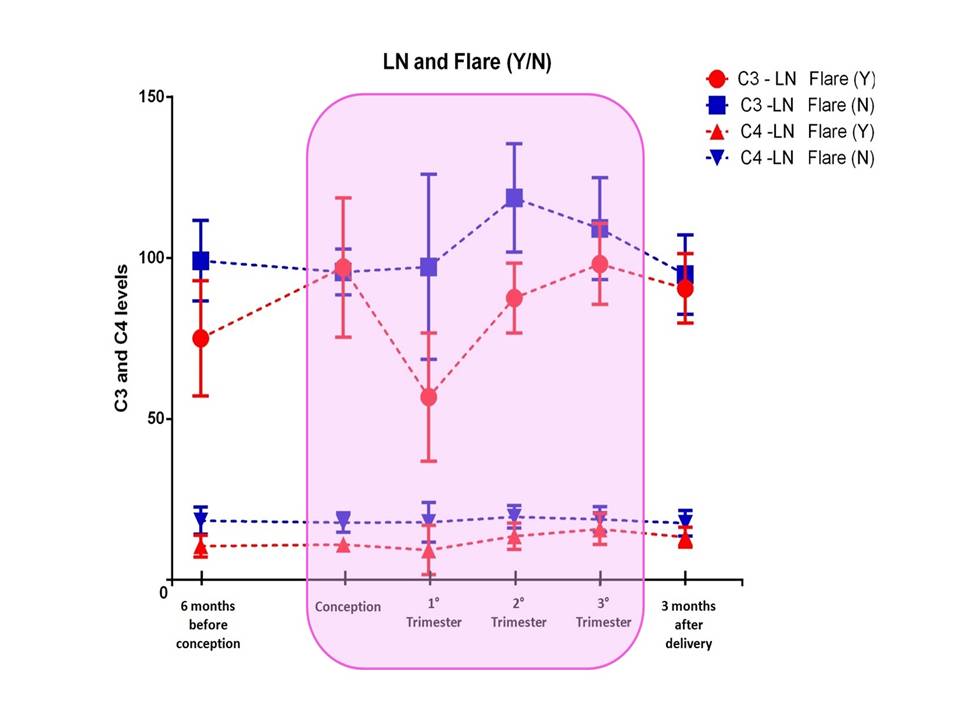 Figure 1. Complement Levels during time in patients with Lupus Nephritis and presence, or absence, of flare during pregnancy.
Figure 1. Complement Levels during time in patients with Lupus Nephritis and presence, or absence, of flare during pregnancy. Disclosures: M. Radin, None; I. Cecchi, None; F. Crisafulli, None; E. Klumb, None; G. De Jesús, None; M. Saavedra, None; G. Reyes-Navarro, None; L. iaccarino, None; M. Larosa, None; G. Moroni, None; F. Tamborini, None; d. Roccatello, None; L. Andreoli, None; C. Chighizola, None; S. Sciascia, None.

