Back
Poster Session D
Session: (2052–2107) SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
2091: Burden and Incidence of Multimorbidity in Systemic Lupus Erythematosus in a Community Population-Based Cohort: The Lupus Midwest Network
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- GF
Gabriel Figueroa-Parra, MD
Mayo Clinic
Rochester, MN, United States
Abstract Poster Presenter(s)
Gabriel Figueroa Parra1, Jose Meade Aguilar1, Cynthia Crowson2, Cassondra Hulshizer1, Tina Gunderson1, Alanna Chamberlain1 and Ali Duarte-Garcia1, 1Mayo Clinic, Rochester, MN, 2Mayo Clinic, Eyota, MN
Background/Purpose: As the life expectancy of patients with systemic lupus erythematosus (SLE) improves, comorbidities have become more critical. Multimorbidity (MM2+) is defined as the coexistence of two or more chronic diseases. There is limited knowledge about the prevalence of MM2+ at SLE diagnosis and its development after SLE onset. We aimed to assess the prevalence (burden) of MM2+ at SLE classification and its incidence after SLE onset in a community population-based cohort of SLE patients compared to matched controls.
Methods: Incident SLE patients meeting the 2019 EULAR/ACR classification criteria in a population-based cohort, matched 1:1 on sex, age, and county of residence to non-SLE comparators from the same underlying population, were included. We assembled 57 chronic condition categories based upon previously described 44 categories (England, BR. ARD 2020). The 13 additional categories were added based on the SLICC/ACR damage index (SDI) or were otherwise considered relevant to SLE. MM2+ was defined as the presence of two or more chronic conditions categories. Five or more chronic conditions (MM5+) was used as a secondary definition. Comorbidities were assessed using ICD codes within a two-year lookback period to determine the burden at SLE classification. Two or more codes at least 30 days apart were required to count a comorbidity.
The categories were stratified as "SLE-related" if they were included in the SDI; the rest were classified as "non-SLE-related." Logistic regression models were used to estimate the odds ratio (OR) at baseline. Aalen-Johansen methods were used to estimate the cumulative incidence of MM2+ and MM5+ among patients with SLE and comparators. Cox proportional hazards models adjusted for age, sex, and calendar year of incidence were used to estimate the probability of developing MM2+ and MM5+ in both groups. OR p-values were false discovery rate (FDR)-adjusted.
Results: We included 268 patients with SLE and 264 comparators. The median age was 47 years; 80% and 81% were female and 80% and 89% were non-Hispanic White, respectively.
At SLE classification, 56.3% of the patients with SLE already had MM2+ compared to 37.9% of non-SLE comparators (OR 2.34, 95% CI 1.62, 3.40). The burden of MM2+ given by non-SLE-related conditions was higher (47.8% in patients with SLE and 32.6% in comparators) than the burden given by SLE-related conditions (17.2% and 6.8%, respectively). Results were similar using the MM5+ definition. (Table 1)
After SLE classification, the risk of developing MM2+ was 2.5-fold higher among patients with SLE than comparators (hazard ratio (HR) 2.46, 95% CI 1.84, 3.29); the risk given by SLE-related conditions was substantially higher (HR 3.08, 95% CI 2.29, 4.15) than the risk given by non-SLE-related conditions (HR 1.93, 95% CI, 1.47, 2.53). Results were similar using the MM5+ definition (Figure 1).
Conclusion: Patients with SLE have a higher burden of multimorbidity even before SLE classification, driven predominantly by non-SLE-associated comorbidities. SLE-specific comorbidities drive the elevated risk of multimorbidity after SLE classification, but chronic conditions not traditionally associated with SLE are also elevated.
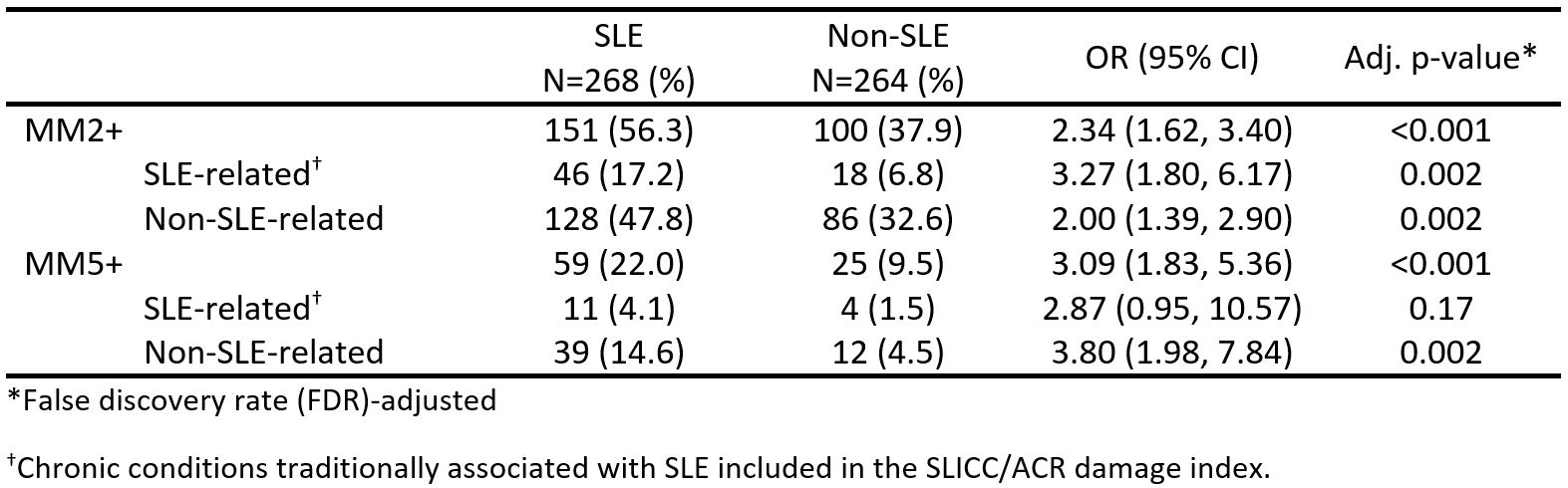 Table 1. Burden of multimorbidity (MM2+) and substantial multimorbidity (MM5+) among patients with systemic lupus erythematosus (SLE) and matched comparators at SLE classification. OR = odds ratio
Table 1. Burden of multimorbidity (MM2+) and substantial multimorbidity (MM5+) among patients with systemic lupus erythematosus (SLE) and matched comparators at SLE classification. OR = odds ratio
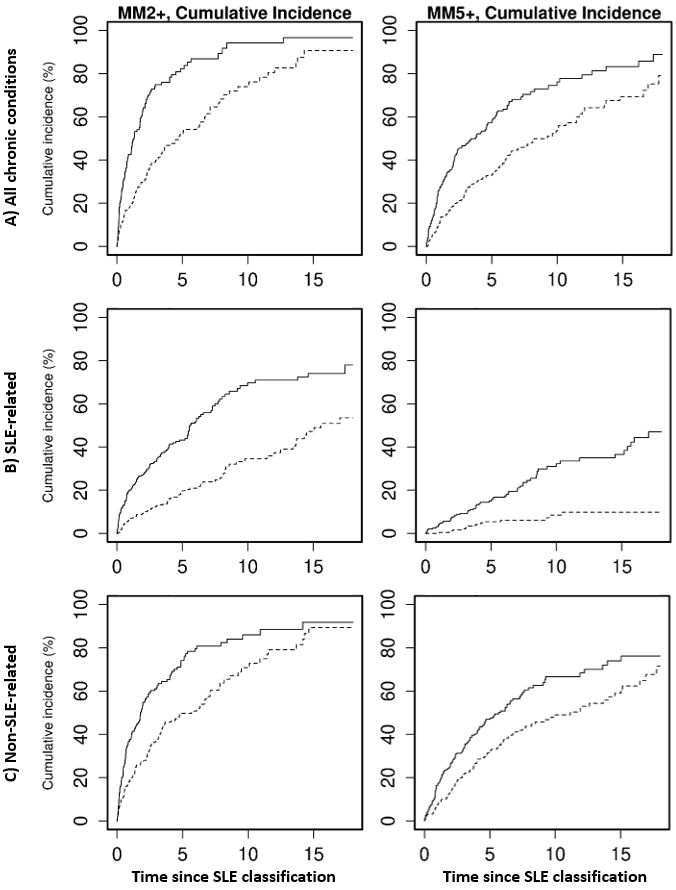 Figure 1. A) Cumulative incidence of multimorbidity (MM2+) and substantial multimorbidity (MM5+) among patients with systemic lupus erythematosus (SLE; solid line) after diagnosis and matched comparators (dashed line). B) MM2+ and MM5+ given by chronic conditions related to SLE and C) by conditions not traditionally related to SLE. Cox models adjusted for age, sex, and calendar year.
Figure 1. A) Cumulative incidence of multimorbidity (MM2+) and substantial multimorbidity (MM5+) among patients with systemic lupus erythematosus (SLE; solid line) after diagnosis and matched comparators (dashed line). B) MM2+ and MM5+ given by chronic conditions related to SLE and C) by conditions not traditionally related to SLE. Cox models adjusted for age, sex, and calendar year.
Disclosures: G. Figueroa Parra, None; J. Meade Aguilar, None; C. Crowson, None; C. Hulshizer, None; T. Gunderson, None; A. Chamberlain, None; A. Duarte-Garcia, None.
Background/Purpose: As the life expectancy of patients with systemic lupus erythematosus (SLE) improves, comorbidities have become more critical. Multimorbidity (MM2+) is defined as the coexistence of two or more chronic diseases. There is limited knowledge about the prevalence of MM2+ at SLE diagnosis and its development after SLE onset. We aimed to assess the prevalence (burden) of MM2+ at SLE classification and its incidence after SLE onset in a community population-based cohort of SLE patients compared to matched controls.
Methods: Incident SLE patients meeting the 2019 EULAR/ACR classification criteria in a population-based cohort, matched 1:1 on sex, age, and county of residence to non-SLE comparators from the same underlying population, were included. We assembled 57 chronic condition categories based upon previously described 44 categories (England, BR. ARD 2020). The 13 additional categories were added based on the SLICC/ACR damage index (SDI) or were otherwise considered relevant to SLE. MM2+ was defined as the presence of two or more chronic conditions categories. Five or more chronic conditions (MM5+) was used as a secondary definition. Comorbidities were assessed using ICD codes within a two-year lookback period to determine the burden at SLE classification. Two or more codes at least 30 days apart were required to count a comorbidity.
The categories were stratified as "SLE-related" if they were included in the SDI; the rest were classified as "non-SLE-related." Logistic regression models were used to estimate the odds ratio (OR) at baseline. Aalen-Johansen methods were used to estimate the cumulative incidence of MM2+ and MM5+ among patients with SLE and comparators. Cox proportional hazards models adjusted for age, sex, and calendar year of incidence were used to estimate the probability of developing MM2+ and MM5+ in both groups. OR p-values were false discovery rate (FDR)-adjusted.
Results: We included 268 patients with SLE and 264 comparators. The median age was 47 years; 80% and 81% were female and 80% and 89% were non-Hispanic White, respectively.
At SLE classification, 56.3% of the patients with SLE already had MM2+ compared to 37.9% of non-SLE comparators (OR 2.34, 95% CI 1.62, 3.40). The burden of MM2+ given by non-SLE-related conditions was higher (47.8% in patients with SLE and 32.6% in comparators) than the burden given by SLE-related conditions (17.2% and 6.8%, respectively). Results were similar using the MM5+ definition. (Table 1)
After SLE classification, the risk of developing MM2+ was 2.5-fold higher among patients with SLE than comparators (hazard ratio (HR) 2.46, 95% CI 1.84, 3.29); the risk given by SLE-related conditions was substantially higher (HR 3.08, 95% CI 2.29, 4.15) than the risk given by non-SLE-related conditions (HR 1.93, 95% CI, 1.47, 2.53). Results were similar using the MM5+ definition (Figure 1).
Conclusion: Patients with SLE have a higher burden of multimorbidity even before SLE classification, driven predominantly by non-SLE-associated comorbidities. SLE-specific comorbidities drive the elevated risk of multimorbidity after SLE classification, but chronic conditions not traditionally associated with SLE are also elevated.
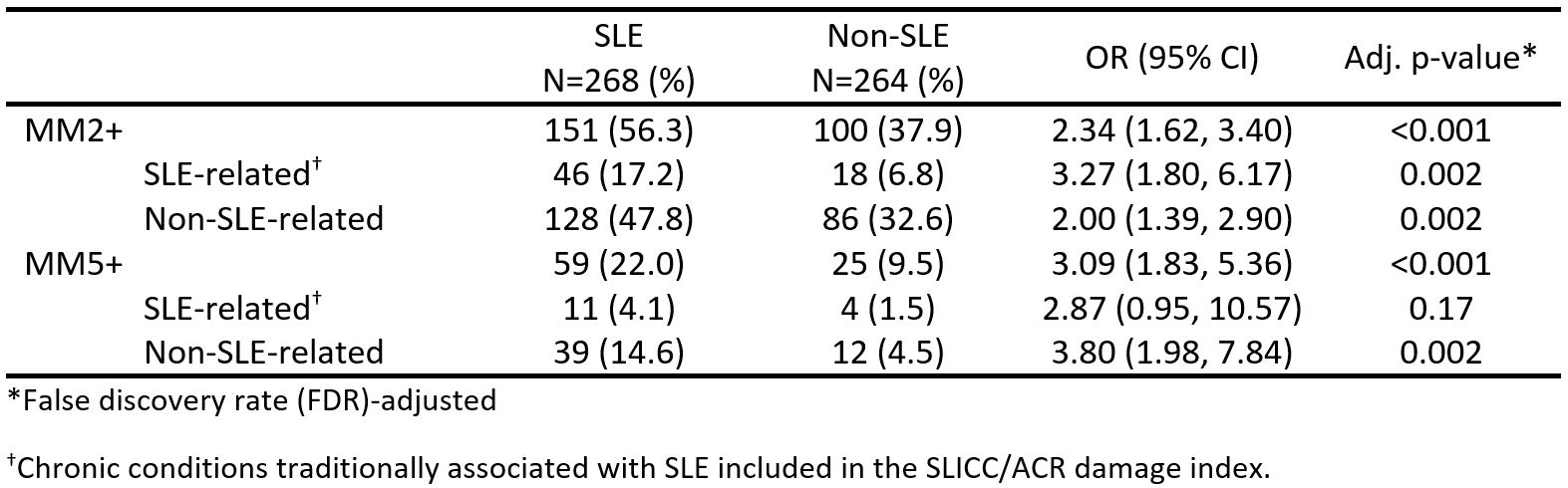 Table 1. Burden of multimorbidity (MM2+) and substantial multimorbidity (MM5+) among patients with systemic lupus erythematosus (SLE) and matched comparators at SLE classification. OR = odds ratio
Table 1. Burden of multimorbidity (MM2+) and substantial multimorbidity (MM5+) among patients with systemic lupus erythematosus (SLE) and matched comparators at SLE classification. OR = odds ratio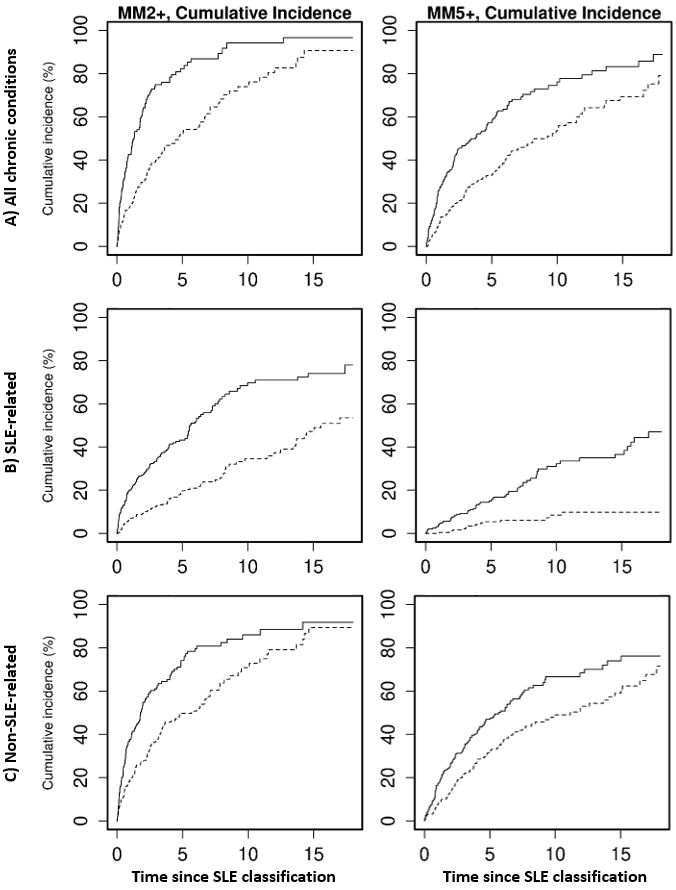 Figure 1. A) Cumulative incidence of multimorbidity (MM2+) and substantial multimorbidity (MM5+) among patients with systemic lupus erythematosus (SLE; solid line) after diagnosis and matched comparators (dashed line). B) MM2+ and MM5+ given by chronic conditions related to SLE and C) by conditions not traditionally related to SLE. Cox models adjusted for age, sex, and calendar year.
Figure 1. A) Cumulative incidence of multimorbidity (MM2+) and substantial multimorbidity (MM5+) among patients with systemic lupus erythematosus (SLE; solid line) after diagnosis and matched comparators (dashed line). B) MM2+ and MM5+ given by chronic conditions related to SLE and C) by conditions not traditionally related to SLE. Cox models adjusted for age, sex, and calendar year.Disclosures: G. Figueroa Parra, None; J. Meade Aguilar, None; C. Crowson, None; C. Hulshizer, None; T. Gunderson, None; A. Chamberlain, None; A. Duarte-Garcia, None.

