Back
Poster Session D
Session: (1924–1949) Pediatric Rheumatology – Clinical Poster III: Other
1945: Determinants of Patient’s Global Assessment of Disease Severity and Predictors of Disease Course in Juvenile Fibromyalgia
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- BM
Benedetta Mori, -None-
Università degli studi di Genova
San Giuliano Milanese, Milan, Italy
Abstract Poster Presenter(s)
Clara Malattia1, Claudio Lavarello1, Alessandra Alongi2, Benedetta Mori2, Anna Ronchetti3, Lino Nobili4, Lorenzo Chiarella5, Elena Pescio6, Angelo Ravelli7 and Marco Gattorno8, 1Pediatric Clinic and Rheumatology Unit, IRCCS Istituto Giannina Gaslini, Genoa, Italy,Department of Neurosciences, Rehabilitation, Ophthalmology, Genetic and Maternal Infantile Sciences (DINOGMI) University of Genoa, Genova, Italy, 2Department of Pediatric Emergency, ARNAS Civico-Di Cristina-Benfratelli, Palermo, Italy, 3Physical Medicine and Rehabilitation Unit, IRCCS Istituto Giannina Gaslini, Genova, Italy, 4Child Neuropsychiatry Unit, IRCCS Istituto Giannina Gaslini, Genoa, Italy,Department of Neurosciences, Rehabilitation, Ophthalmology, Genetic and Maternal Infantile Sciences (DINOGMI) University of Genoa, Genova, Italy, 5Child Neuropsychiatry Unit, IRCCS Istituto Giannina Gaslini, Genoa, Italy,Department of Neurosciences, Rehabilitation, Ophthalmology, Genetic and Maternal Infantile Sciences (DINOGMI) University of Genoa, Genova, 6Psychology Unit, IRCCS Istituto Giannina Gaslini, Genova, Italy, 7Department of Neurosciences, Rehabilitation, Ophthalmology, Genetic and Maternal Infantile Sciences (DINOGMI) University of Genoa, Italy,Scientific Direction, IRCCS Istituto Giannina Gaslini, Genova, Italy, 8Pediatric Clinic and Rheumatology Unit, IRCCS Istituto Giannina Gaslini, Genoa, Italy
Background/Purpose: Juvenile Fibromyalgia Syndrome (JFS) is a disabling condition characterized by widespread musculoskeletal pain, fatigue and mood disturbances, which impact significantly on patients' quality of life. Very few data on disease course and prognostic factors are currently available due to the lack of longitudinal cohort studies in JFS.We aim to determine the impact of JFS-related symptoms on patient's global assessment of disease severity (PGA) and to identify predictors of disease course.
Methods: We included JFS patients followed at our center between 2018 and 2022. At each follow-up (FU) visit, patients filled a multidimensional questionnaire that evaluates symptoms severity, quality of life and functional ability. Self-report measures (0-10 Visual Analogue Scale) were used to rate the severity of symptoms in the following domains: pain, fatigue, headache, sleep quality, anxyety, depression, cognitive impairement and patient's global assessment of disease severity. Correlation and mediation analyses were performed to explore the relationship between JFS symptoms and PGA. A mixed effects logistic model with random intercepts for subjects was fitted to identify predictors of physician-assessed improvement among demographic features and JFS symptoms at the first visit.
Results: We included 51 patients (44 F; median age at onset 13.7 yrs; median disease duration 1.8 yrs). Median PGA at the inclusion was 7.0 (IQR 5.0, 8.0). Patients were on regular physical activity in 83/194 (43%) FU visits and on medications in 70/194 (36%) FU visits. A strong correlation was found between PGA and pain (r = 0.68, 95%cl 0.59 -0.76), fatigue (r = 0.62, 95%cl 0.52-0.71) and depression (r = 0.60, 95%cl 0.48-0.69). Mediation analysis showed that fatigue and pain are the major determinants of PGA (figure). The impact of fatigue on PGA (total effect β 0.44, 95%cl 0.28-0.56,p< .001) is mediated by sleep quality (β 0.17, 95%cl 0.08-0.31,p< .001) and depression (β 0.14, 95%cl 0.08-0.25,p< .001). Cognitive impairment had an indirect effect on PGA which is mediated by depression (β 0.14, 95%cl 0.08-0.25,p< .001).
Twenty-nine out of 51(56.8%) patients were classified as improved by treating physician in at least one FU visit. The proportion of improved patients was higher among patients on regular physical activity (60%) than in those underdoing medical treatment (2.9%) or combined therapy (50%) (medical and physical therapy) (Pearson´s χ2, p < 0.001). Higher score in the cognitive impairment domain at baseline was associated with lower odds of improvement at FU visits (OR 0.81, 95% CL 0.68-0.97, p = 0.018).
Conclusion: Pain and fatigue are the main determinants of PGA, either directly or due to their influence on sleep and mood disturbances. Elucidation of the impact of disease-related symptoms on PGA might provide insights for the developement of more comprehensive and targeted therapeutic approaches in JFS.
Regular aerobic exercise is associated to a better disease course, while cognitive impairment is a potential predictor of a poor outcome. Interventional studies are needed to determine whether targeting fatigue and cognitive impairment can improve disease severity and outcomes.
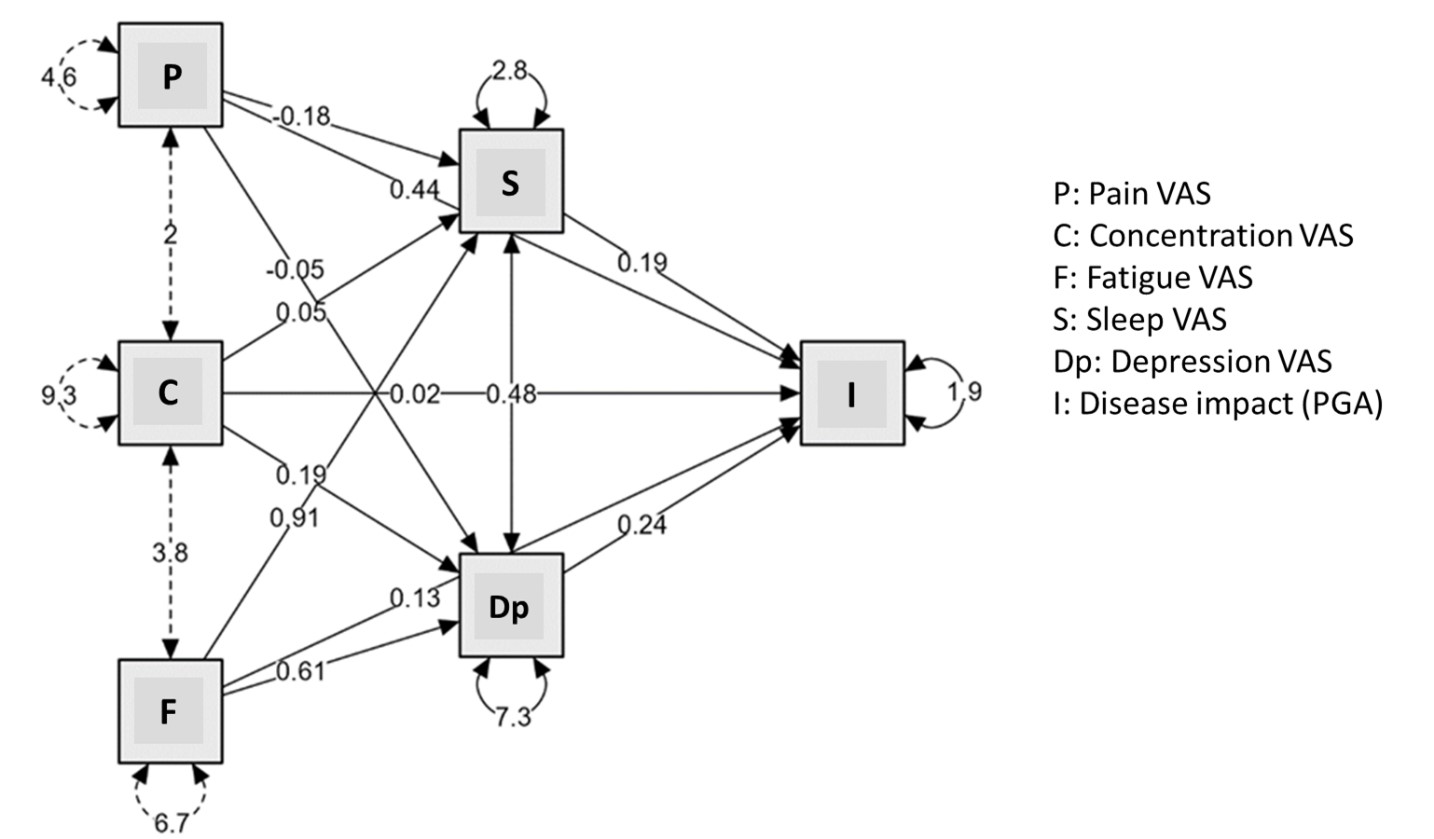 Figure: Path diagram with associated beta coefficients for mediation analysis
Figure: Path diagram with associated beta coefficients for mediation analysis
Disclosures: C. Malattia, None; C. Lavarello, None; A. Alongi, None; B. Mori, None; A. Ronchetti, None; L. Nobili, None; L. Chiarella, None; E. Pescio, None; A. Ravelli, None; M. Gattorno, None.
Background/Purpose: Juvenile Fibromyalgia Syndrome (JFS) is a disabling condition characterized by widespread musculoskeletal pain, fatigue and mood disturbances, which impact significantly on patients' quality of life. Very few data on disease course and prognostic factors are currently available due to the lack of longitudinal cohort studies in JFS.We aim to determine the impact of JFS-related symptoms on patient's global assessment of disease severity (PGA) and to identify predictors of disease course.
Methods: We included JFS patients followed at our center between 2018 and 2022. At each follow-up (FU) visit, patients filled a multidimensional questionnaire that evaluates symptoms severity, quality of life and functional ability. Self-report measures (0-10 Visual Analogue Scale) were used to rate the severity of symptoms in the following domains: pain, fatigue, headache, sleep quality, anxyety, depression, cognitive impairement and patient's global assessment of disease severity. Correlation and mediation analyses were performed to explore the relationship between JFS symptoms and PGA. A mixed effects logistic model with random intercepts for subjects was fitted to identify predictors of physician-assessed improvement among demographic features and JFS symptoms at the first visit.
Results: We included 51 patients (44 F; median age at onset 13.7 yrs; median disease duration 1.8 yrs). Median PGA at the inclusion was 7.0 (IQR 5.0, 8.0). Patients were on regular physical activity in 83/194 (43%) FU visits and on medications in 70/194 (36%) FU visits. A strong correlation was found between PGA and pain (r = 0.68, 95%cl 0.59 -0.76), fatigue (r = 0.62, 95%cl 0.52-0.71) and depression (r = 0.60, 95%cl 0.48-0.69). Mediation analysis showed that fatigue and pain are the major determinants of PGA (figure). The impact of fatigue on PGA (total effect β 0.44, 95%cl 0.28-0.56,p< .001) is mediated by sleep quality (β 0.17, 95%cl 0.08-0.31,p< .001) and depression (β 0.14, 95%cl 0.08-0.25,p< .001). Cognitive impairment had an indirect effect on PGA which is mediated by depression (β 0.14, 95%cl 0.08-0.25,p< .001).
Twenty-nine out of 51(56.8%) patients were classified as improved by treating physician in at least one FU visit. The proportion of improved patients was higher among patients on regular physical activity (60%) than in those underdoing medical treatment (2.9%) or combined therapy (50%) (medical and physical therapy) (Pearson´s χ2, p < 0.001). Higher score in the cognitive impairment domain at baseline was associated with lower odds of improvement at FU visits (OR 0.81, 95% CL 0.68-0.97, p = 0.018).
Conclusion: Pain and fatigue are the main determinants of PGA, either directly or due to their influence on sleep and mood disturbances. Elucidation of the impact of disease-related symptoms on PGA might provide insights for the developement of more comprehensive and targeted therapeutic approaches in JFS.
Regular aerobic exercise is associated to a better disease course, while cognitive impairment is a potential predictor of a poor outcome. Interventional studies are needed to determine whether targeting fatigue and cognitive impairment can improve disease severity and outcomes.
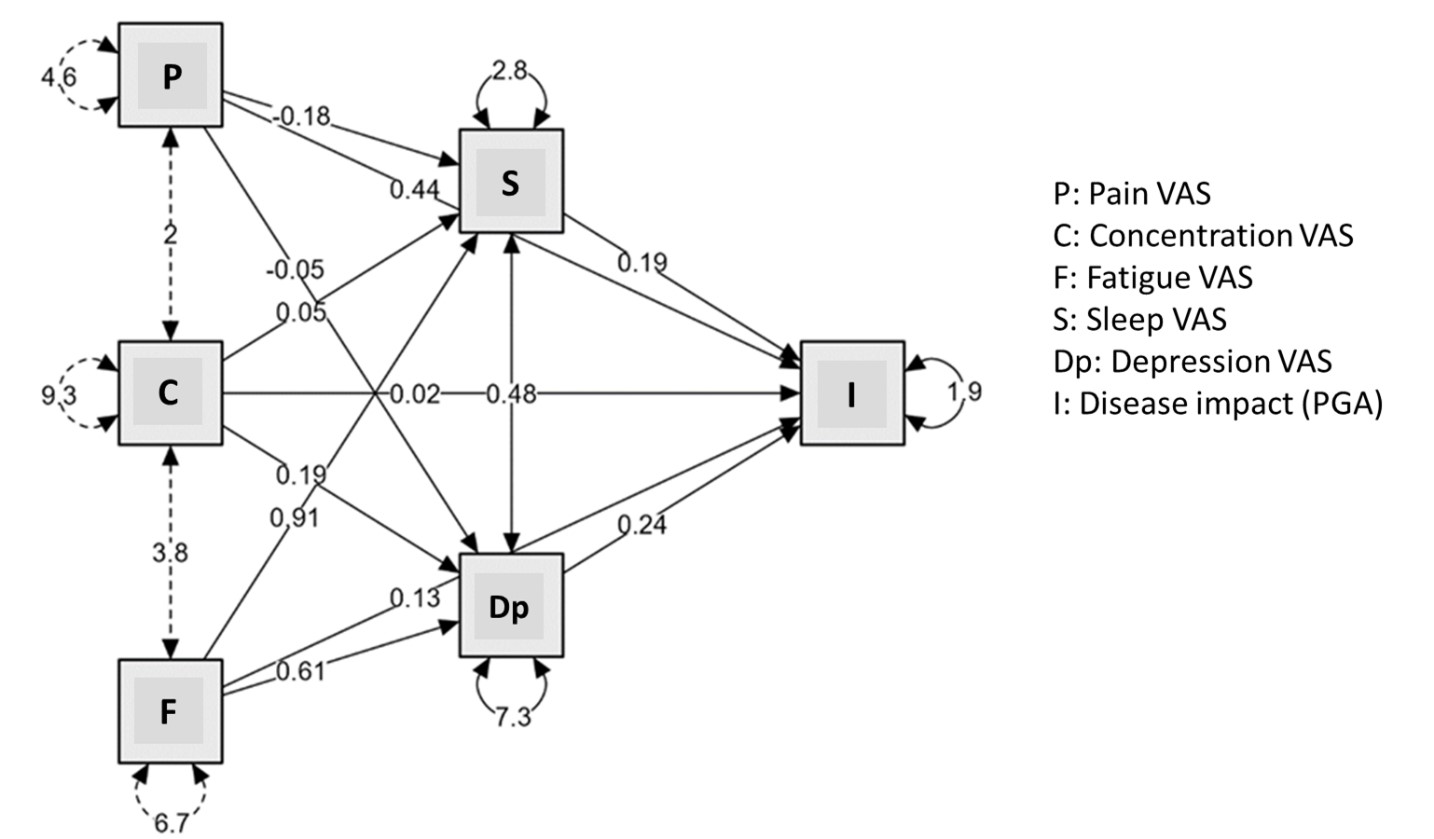 Figure: Path diagram with associated beta coefficients for mediation analysis
Figure: Path diagram with associated beta coefficients for mediation analysisDisclosures: C. Malattia, None; C. Lavarello, None; A. Alongi, None; B. Mori, None; A. Ronchetti, None; L. Nobili, None; L. Chiarella, None; E. Pescio, None; A. Ravelli, None; M. Gattorno, None.

