Back
Poster Session D
Session: (2052–2107) SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
2106: Disparities of African American Mortality Trends in South Carolina Lupus Cohort
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SC
Sean Carter, MD, BS
MUSC
North Charleston, SC, United States
Abstract Poster Presenter(s)
Sean Carter1, Dulaney Wilson1, Samantha Minkin2, David Dillon3, Baxter Murray1 and Jim Oates1, 1Medical University of South Carolina, Charleston, SC, 2Vanderbilt University Medical Center, Nashville, TN, 3Rheumatology Associates of South Florida, Delray Beach, FL
Background/Purpose: SLE is a chronic autoimmune disorder associated with increased mortality compared to the general population; treatment for SLE has improved and survival rates have substantially improved from initial 3-year mortality rates of 40% in 19531, however, there is still a 3-fold increased risk of death2 with early causes of death from SLE activity, steroid use, and infections, while later deaths are related to cardiovascular disease. This study is an observation of mortality trends in a southern SLE cohort that is predominantly female and Black patients which hopes to further describe characteristics associated with increased mortality in SLE patients.
Methods: Data were gathered from patients enrolled in the medical center's lupus registry. Included patients were those who met 1997 ACR SLE criteria and the Systemic Lupus International Collaborating Clinic Damage Index was calculated. From among deceased patients, death certificates were obtained from the state Department of Health with which cause of death was determined by ICD-10 code. Standardized mortality ratio (SMR) was calculated using expected mortality rates from the CDC WONDER database and characteristics between deceased and living patients were compared.
Results: A total of 712 subjects were included in the final analysis. Of these subjects, 102 died during the research period. Total SMR adjusted for age, race, and gender was 12.29 (95% CI 9.97-14.61). SLE was the primary cause of death, followed by infection, atherosclerosis and malignancy. The average age of the decedents was 42. Of the deceased, there was a statistically significant increased mortality association in Black patients, SLICC damage score of 1 or more, older age at study baseline, and shorter disease duration. There was a trend toward increased mortality in male patients, but this did not reach statistical significance.
Conclusion: The SMR in this cohort was higher than the previously defined meta-SMR2. SLE and infection were the two most listed primary causes of mortality for all subjects regardless of disease duration and there was not a difference between causes of death in first 5 years of disease versus greater than 5 years disease duration and lupus nephritis did not have a statistical impact on mortality which differs from previous reports. There was an increased mortality rate in Black patients so Mann-Whitney U test was performed which revealed that Black patients had a statistically significant higher SLICC damage score compared to white patients. This study highlights the importance of investigating the role of racial disparities in SLE patients to help determine whether there might be underlying factors such as environmental, genetic causes, or other social determinants of health.
.jpg) Cohort Demographics comparing total, deceased, and living SLE patients
Cohort Demographics comparing total, deceased, and living SLE patients
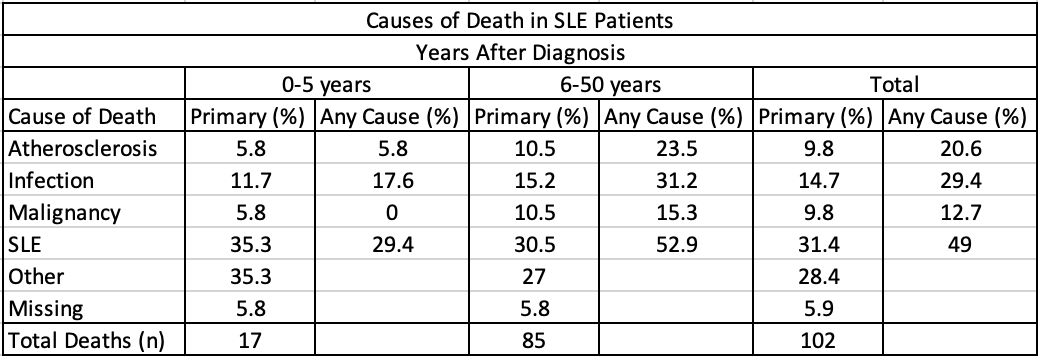 Listed cause of death on death certificate by disease duration
Listed cause of death on death certificate by disease duration
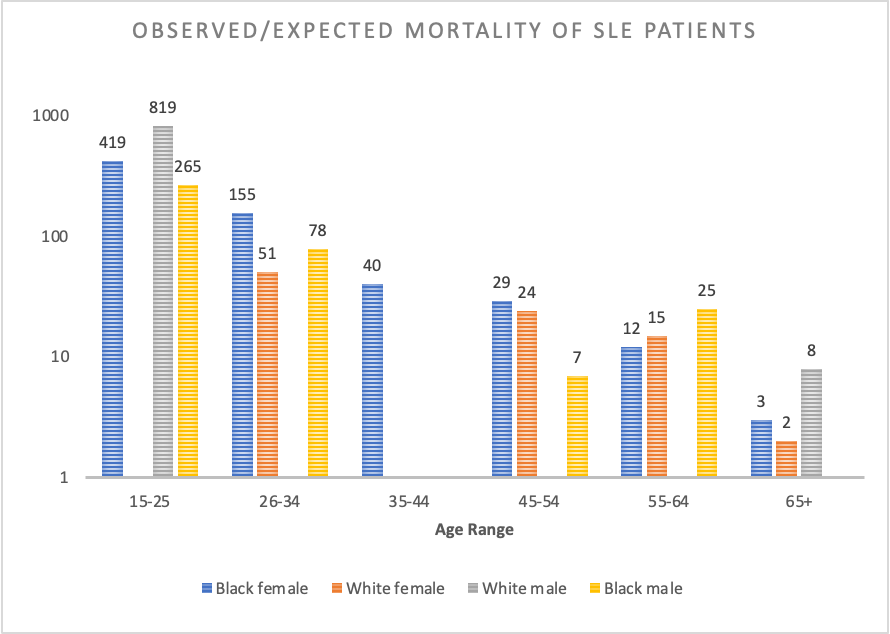 Observed:Expected Mortality Ratio of the cohort by age range
Observed:Expected Mortality Ratio of the cohort by age range
Disclosures: S. Carter, None; D. Wilson, None; S. Minkin, None; D. Dillon, None; B. Murray, None; J. Oates, None.
Background/Purpose: SLE is a chronic autoimmune disorder associated with increased mortality compared to the general population; treatment for SLE has improved and survival rates have substantially improved from initial 3-year mortality rates of 40% in 19531, however, there is still a 3-fold increased risk of death2 with early causes of death from SLE activity, steroid use, and infections, while later deaths are related to cardiovascular disease. This study is an observation of mortality trends in a southern SLE cohort that is predominantly female and Black patients which hopes to further describe characteristics associated with increased mortality in SLE patients.
Methods: Data were gathered from patients enrolled in the medical center's lupus registry. Included patients were those who met 1997 ACR SLE criteria and the Systemic Lupus International Collaborating Clinic Damage Index was calculated. From among deceased patients, death certificates were obtained from the state Department of Health with which cause of death was determined by ICD-10 code. Standardized mortality ratio (SMR) was calculated using expected mortality rates from the CDC WONDER database and characteristics between deceased and living patients were compared.
Results: A total of 712 subjects were included in the final analysis. Of these subjects, 102 died during the research period. Total SMR adjusted for age, race, and gender was 12.29 (95% CI 9.97-14.61). SLE was the primary cause of death, followed by infection, atherosclerosis and malignancy. The average age of the decedents was 42. Of the deceased, there was a statistically significant increased mortality association in Black patients, SLICC damage score of 1 or more, older age at study baseline, and shorter disease duration. There was a trend toward increased mortality in male patients, but this did not reach statistical significance.
Conclusion: The SMR in this cohort was higher than the previously defined meta-SMR2. SLE and infection were the two most listed primary causes of mortality for all subjects regardless of disease duration and there was not a difference between causes of death in first 5 years of disease versus greater than 5 years disease duration and lupus nephritis did not have a statistical impact on mortality which differs from previous reports. There was an increased mortality rate in Black patients so Mann-Whitney U test was performed which revealed that Black patients had a statistically significant higher SLICC damage score compared to white patients. This study highlights the importance of investigating the role of racial disparities in SLE patients to help determine whether there might be underlying factors such as environmental, genetic causes, or other social determinants of health.
- Jessar, R. A., Lamont-Havers, R. W., & Ragan, C. (1953). Natural history of lupus erythematosus disseminatus. Ann Intern Med, 38(4), 717-731. https://doi.org/10.7326/0003-4819-38-4-717
- Yurkovich, M., Vostretsova, K., Chen, W., & Aviña-Zubieta, J. A. (2014). Overall and cause-specific mortality in patients with SLE: a meta-analysis of observational studies. Arthritis Care Res (Hoboken), 66(4), 608-616. https://doi.org/10.1002/acr.22173
.jpg) Cohort Demographics comparing total, deceased, and living SLE patients
Cohort Demographics comparing total, deceased, and living SLE patients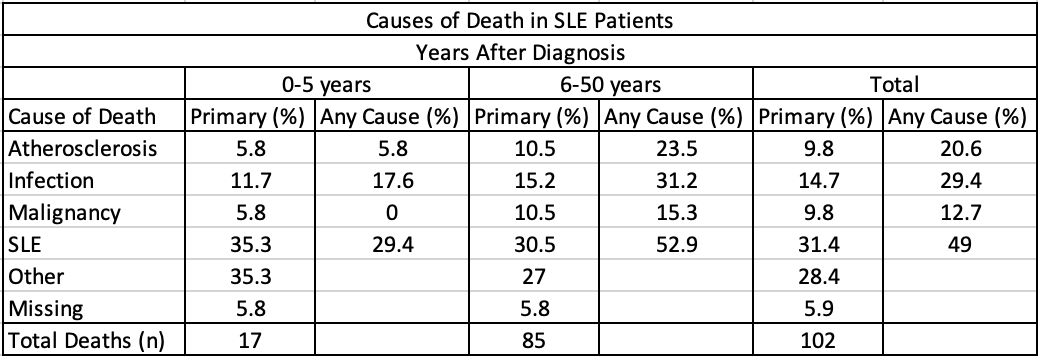 Listed cause of death on death certificate by disease duration
Listed cause of death on death certificate by disease duration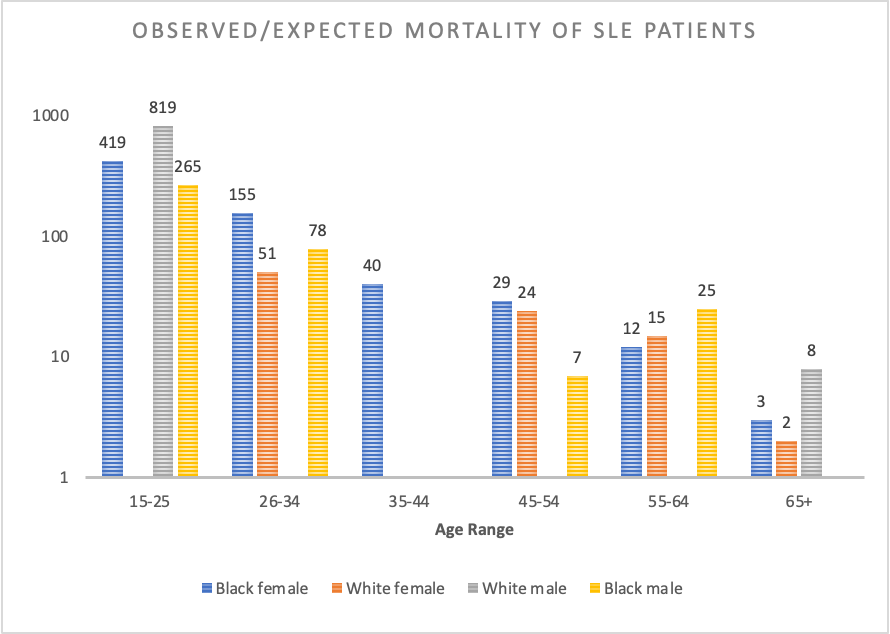 Observed:Expected Mortality Ratio of the cohort by age range
Observed:Expected Mortality Ratio of the cohort by age rangeDisclosures: S. Carter, None; D. Wilson, None; S. Minkin, None; D. Dillon, None; B. Murray, None; J. Oates, None.

