Back
Ignite Talk
Session: Ignite Session 2A
0071: Workforce Changes and Characteristics of Adult Rheumatologists in a United States Medicare Claims Analysis
Saturday, November 12, 2022
2:40 PM – 2:45 PM Eastern Time
Location: Northern Liberties Stage
- MM
Melissa Mannion, MD
University of Alabama at Birmingham
Birmingham, AL, United StatesDisclosure: Disclosure information not submitted.
Ignite Speaker(s)
Melissa Mannion1, Fenglong Xie1, John FitzGerald2, Amy Mudano3, Zihan Wan1 and Jeffrey Curtis4, 1University of Alabama at Birmingham, Birmingham, AL, 2University of California Los Angeles, Los Angeles, CA, 3Illumination Health, Hoover, AL, 4University of Alabama at Birmingham, Hoover, AL
Background/Purpose: Prior studies have projected inadequate growth in the rheumatology provider workforce to keep up with population demand. The objective of this project was to estimate the current status and evolution over time of the adult rheumatology workforce in the United States using administrative claims data from Medicare.
Methods: Using a 100% sample of Medicare claims from 2000 to 2019 for rheumatologic diseases augmented by multiple external resources, we identified adult rheumatologists by National Provider Identifier (NPI) number and specialty taxonomy codes that billed for ≥10 patients in a calendar year. Providers were classified as entering the workforce if they were not identified in a prior year, and exiting the workforce if they were not identified in the subsequent year. Demographic characteristics of the workforce, U.S. Census definitions for rural or urban practice setting, and practice size (large practice defined as >3 physicians) were descriptively summarized.
Results: There were 5,843 rheumatologists identified in Medicare claims in 2019. The active workforce in 2019 was 51% male, the proportion of female physicians entering (37%) was greater than those exiting (25%) while the opposite was true for male physicians (35% entering, 55% exiting). Most rheumatologists were in non-academic (89%), large practice (74%), and urban (75%) settings. The total active physicians increased from 4304 to 5843 during the study period. There was an increase in entering physicians from 2000 to a peak in 2008 (n=435) followed by a decline since 2013. The number of exiting physicians has been less than the number of entering except for years (2007 and 2019).
Conclusion: The total number of practicing adult rheumatologists increased over time with a drop in physicians entering the workforce in recent years. Ongoing work is evaluating similar changes in advanced practice providers (e.g. nurse practitioners, physician assistants), and the geographic location of rheumatologists' practices. This data can help inform policy, training, and workforce growth initiatives to ensure adequate access to rheumatology providers for patients with rheumatic diseases.
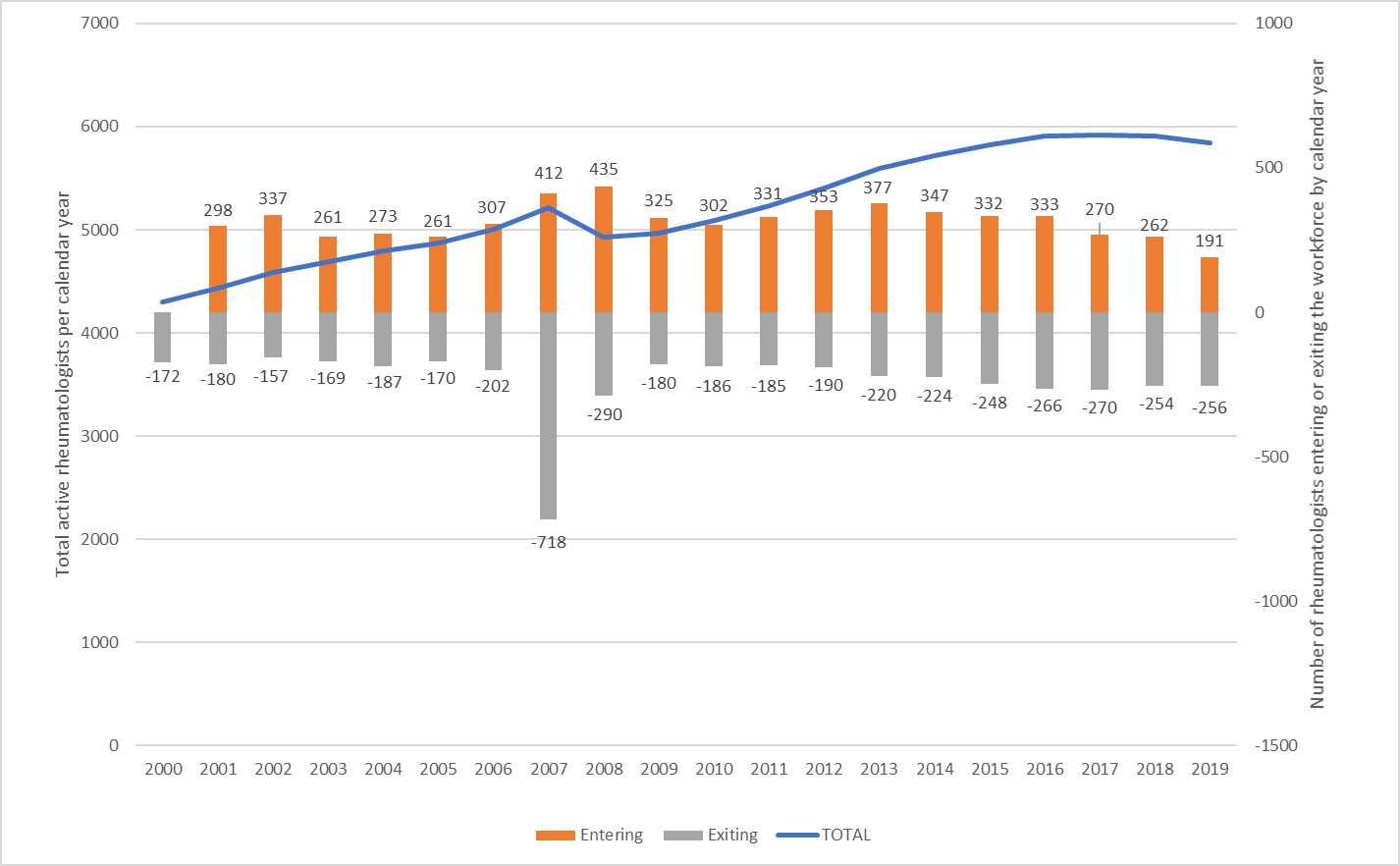 Figure 1: Change in total rheumatologists (line) and rheumatologists entering or exiting (stacked columns) by calendar year in Medicare claims data
Figure 1: Change in total rheumatologists (line) and rheumatologists entering or exiting (stacked columns) by calendar year in Medicare claims data
Disclosures: M. Mannion, None; F. Xie, Bendcare; J. FitzGerald, None; A. Mudano, None; Z. Wan, None; J. Curtis, AbbVie/Abbott, Amgen, ArthritisPower, Aqtual, Bendcare, Bristol-Myers Squibb(BMS), CorEvitas, FASTER, GlaxoSmithKlein(GSK), IlluminationHealth, Janssen, Labcorp, Eli Lilly, Myriad, Novartis, Pfizer, Sanofi, Scipher, Setpoint, UCB, United Rheumatology.
Background/Purpose: Prior studies have projected inadequate growth in the rheumatology provider workforce to keep up with population demand. The objective of this project was to estimate the current status and evolution over time of the adult rheumatology workforce in the United States using administrative claims data from Medicare.
Methods: Using a 100% sample of Medicare claims from 2000 to 2019 for rheumatologic diseases augmented by multiple external resources, we identified adult rheumatologists by National Provider Identifier (NPI) number and specialty taxonomy codes that billed for ≥10 patients in a calendar year. Providers were classified as entering the workforce if they were not identified in a prior year, and exiting the workforce if they were not identified in the subsequent year. Demographic characteristics of the workforce, U.S. Census definitions for rural or urban practice setting, and practice size (large practice defined as >3 physicians) were descriptively summarized.
Results: There were 5,843 rheumatologists identified in Medicare claims in 2019. The active workforce in 2019 was 51% male, the proportion of female physicians entering (37%) was greater than those exiting (25%) while the opposite was true for male physicians (35% entering, 55% exiting). Most rheumatologists were in non-academic (89%), large practice (74%), and urban (75%) settings. The total active physicians increased from 4304 to 5843 during the study period. There was an increase in entering physicians from 2000 to a peak in 2008 (n=435) followed by a decline since 2013. The number of exiting physicians has been less than the number of entering except for years (2007 and 2019).
Conclusion: The total number of practicing adult rheumatologists increased over time with a drop in physicians entering the workforce in recent years. Ongoing work is evaluating similar changes in advanced practice providers (e.g. nurse practitioners, physician assistants), and the geographic location of rheumatologists' practices. This data can help inform policy, training, and workforce growth initiatives to ensure adequate access to rheumatology providers for patients with rheumatic diseases.
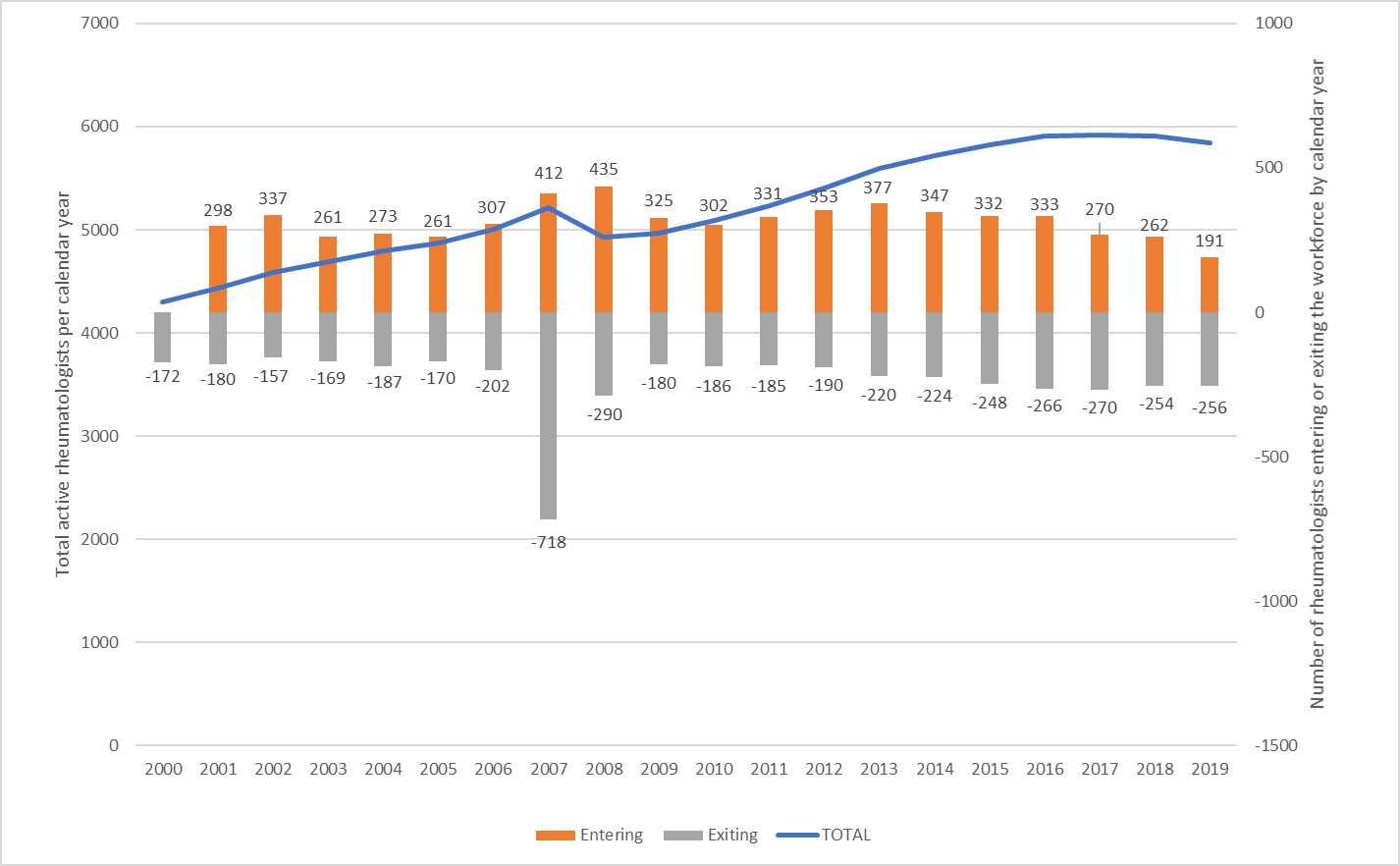 Figure 1: Change in total rheumatologists (line) and rheumatologists entering or exiting (stacked columns) by calendar year in Medicare claims data
Figure 1: Change in total rheumatologists (line) and rheumatologists entering or exiting (stacked columns) by calendar year in Medicare claims dataDisclosures: M. Mannion, None; F. Xie, Bendcare; J. FitzGerald, None; A. Mudano, None; Z. Wan, None; J. Curtis, AbbVie/Abbott, Amgen, ArthritisPower, Aqtual, Bendcare, Bristol-Myers Squibb(BMS), CorEvitas, FASTER, GlaxoSmithKlein(GSK), IlluminationHealth, Janssen, Labcorp, Eli Lilly, Myriad, Novartis, Pfizer, Sanofi, Scipher, Setpoint, UCB, United Rheumatology.

