Back
Poster Session B
Osteoarthritis (OA) and related disorders
Session: (0833–0849) Orthopedics, Low Back Pain, and Rehabilitation Poster
0502: The Effect of Osteoporosis on Developing Vertebral Compression Fracture After Single-level Posterior Lumbar Fusion Surgery: A Large Healthcare Claims Database Study
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- VK
Vartika Kesarwani, MBBS
University of Connecticut
Hartford, CT, United States
Abstract Poster Presenter(s)
Vartika Kesarwani1, Sean Esmende2, Regina Kostyun2, Matthew Solomito2, Heeren Makanji2, John Magaldi2 and Mandeep Kumar2, 1University of Connecticut, Farmington, CT, 2Bone and Joint Institute, Hartford Hospital, Hartford, CT
Background/Purpose: Vertebral compression fracture (VCF) is a significant osteoporosis-related complication (ORC) associated with instrumented spinal fusion. Various studies have assessed the development of VCF in patients undergoing three or greater level spinal fusion. There is a gap in the assessment of VCF following single-level fusion, which may predispose patients to greater stress due to the lack of fixation points. This study aimed to examine the occurrence of VCF among patients with osteoporosis undergoing instrumented single-level posterior lumbar fusion (SLPF) surgery. We hypothesized that surgical patients with osteoporosis would have a greater incidence of compression fractures within the year following surgery than surgical patients without osteoporosis and the year following diagnosis of osteoporosis in the non-surgical group.
Methods: This was a retrospective cohort study using a commercially available medical claims database, PearlDiver. Patient records from 2011 to 2019 were queried and filtered (Figure 1) to identify patients who had an SLPF procedure following a diagnosis of osteoporosis (OP Fusion Group), patients with an SLPF procedure without a preexisting diagnosis of osteoporosis (No OP Fusion Group), and patients with osteoporosis who did not have an SLPF within a year of diagnosis (OP Group). The primary outcomes were the development of a VCF within the year following SLPF for the surgical group or within the year of osteoporosis diagnosis for the control group. Statistical analyses were performed using R software. Differences in the rate of VCF were assessed using chi-square tests. Univariate and multivariate logistic regression analyses were used to understand the association between osteoporosis and SLPF and covariates to VCF.
Results: The query identified 694 patients in the OP Fusion, 25,935 in the No OP Fusion, and 18,455 in the OP Group. Majority were females (OP Fusion = 90%, No OP Fusion = 58.4%, and OP Group = 85%). There were a higher number of patients > 60 years in the OP Fusion and OP Group (78% and 73%) compared to the No OP Fusion Group (53%). A greater number of VCF were diagnosed among patients in the OP Fusion compared to the No OP Fusion Group within the year following SLPF (χ2=10.8 p=0.001) (Table 1). There was no difference in VCF rates between OP Fusion and the OP Group (p=0.218). Univariate logistic analyses identified that female gender, age 70-84 years, Charlson Comorbidity Index (CCI), and osteoporosis pharmacotherapy were associated with developing a VFC after SLPF. After including these variables in the multivariate model, osteoporosis was no longer a risk factor for developing VCF after SLPF (Table 2).
Conclusion: In this large multi-year cohort, the incidence rate of VCF was less than 2%. A pre-operative diagnosis of osteoporosis alone may not be an independent risk factor for developing VCF following SLPF. Other clinical factors such as female gender, 70 years of age or older, higher CCI scores, and osteoporosis treatment should be considered when determining the risk for VCF following surgery.
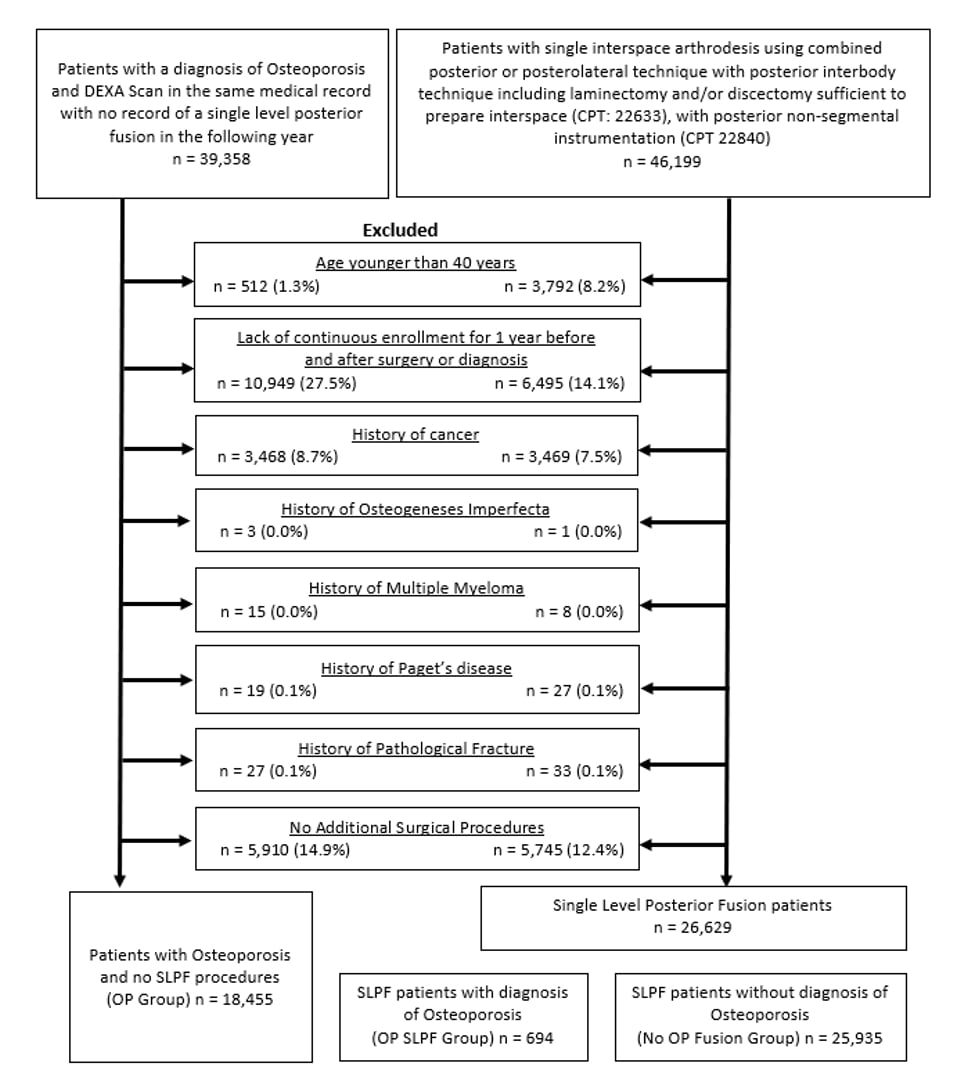 Figure 1: Flow chart for inclusion and exclusion criteria of the patient query.
Figure 1: Flow chart for inclusion and exclusion criteria of the patient query.
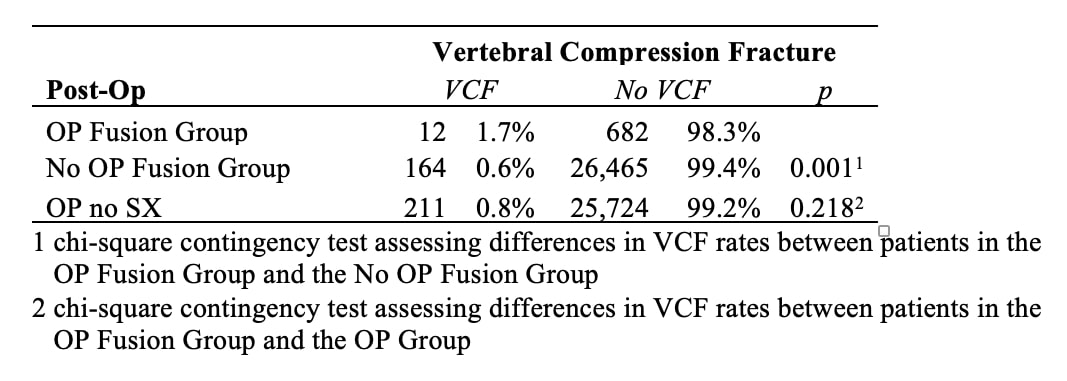 Table 1: Incidence of VCF among patients with osteoporosis underdoing SLPF.
Table 1: Incidence of VCF among patients with osteoporosis underdoing SLPF.
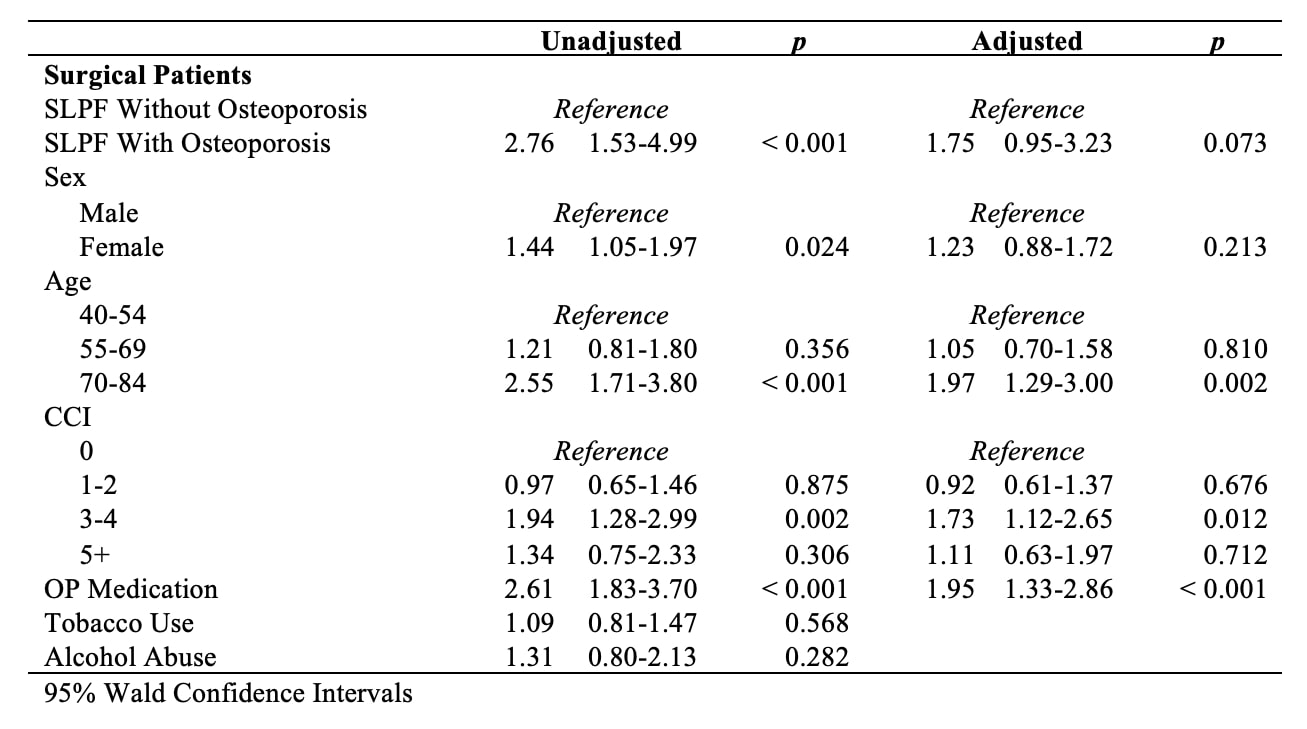 Table 2: Unadjusted and adjusted multivariate analysis for developing a VCF within the year after surgery.
Table 2: Unadjusted and adjusted multivariate analysis for developing a VCF within the year after surgery.
Disclosures: V. Kesarwani, None; S. Esmende, None; R. Kostyun, None; M. Solomito, None; H. Makanji, None; J. Magaldi, None; M. Kumar, None.
Background/Purpose: Vertebral compression fracture (VCF) is a significant osteoporosis-related complication (ORC) associated with instrumented spinal fusion. Various studies have assessed the development of VCF in patients undergoing three or greater level spinal fusion. There is a gap in the assessment of VCF following single-level fusion, which may predispose patients to greater stress due to the lack of fixation points. This study aimed to examine the occurrence of VCF among patients with osteoporosis undergoing instrumented single-level posterior lumbar fusion (SLPF) surgery. We hypothesized that surgical patients with osteoporosis would have a greater incidence of compression fractures within the year following surgery than surgical patients without osteoporosis and the year following diagnosis of osteoporosis in the non-surgical group.
Methods: This was a retrospective cohort study using a commercially available medical claims database, PearlDiver. Patient records from 2011 to 2019 were queried and filtered (Figure 1) to identify patients who had an SLPF procedure following a diagnosis of osteoporosis (OP Fusion Group), patients with an SLPF procedure without a preexisting diagnosis of osteoporosis (No OP Fusion Group), and patients with osteoporosis who did not have an SLPF within a year of diagnosis (OP Group). The primary outcomes were the development of a VCF within the year following SLPF for the surgical group or within the year of osteoporosis diagnosis for the control group. Statistical analyses were performed using R software. Differences in the rate of VCF were assessed using chi-square tests. Univariate and multivariate logistic regression analyses were used to understand the association between osteoporosis and SLPF and covariates to VCF.
Results: The query identified 694 patients in the OP Fusion, 25,935 in the No OP Fusion, and 18,455 in the OP Group. Majority were females (OP Fusion = 90%, No OP Fusion = 58.4%, and OP Group = 85%). There were a higher number of patients > 60 years in the OP Fusion and OP Group (78% and 73%) compared to the No OP Fusion Group (53%). A greater number of VCF were diagnosed among patients in the OP Fusion compared to the No OP Fusion Group within the year following SLPF (χ2=10.8 p=0.001) (Table 1). There was no difference in VCF rates between OP Fusion and the OP Group (p=0.218). Univariate logistic analyses identified that female gender, age 70-84 years, Charlson Comorbidity Index (CCI), and osteoporosis pharmacotherapy were associated with developing a VFC after SLPF. After including these variables in the multivariate model, osteoporosis was no longer a risk factor for developing VCF after SLPF (Table 2).
Conclusion: In this large multi-year cohort, the incidence rate of VCF was less than 2%. A pre-operative diagnosis of osteoporosis alone may not be an independent risk factor for developing VCF following SLPF. Other clinical factors such as female gender, 70 years of age or older, higher CCI scores, and osteoporosis treatment should be considered when determining the risk for VCF following surgery.
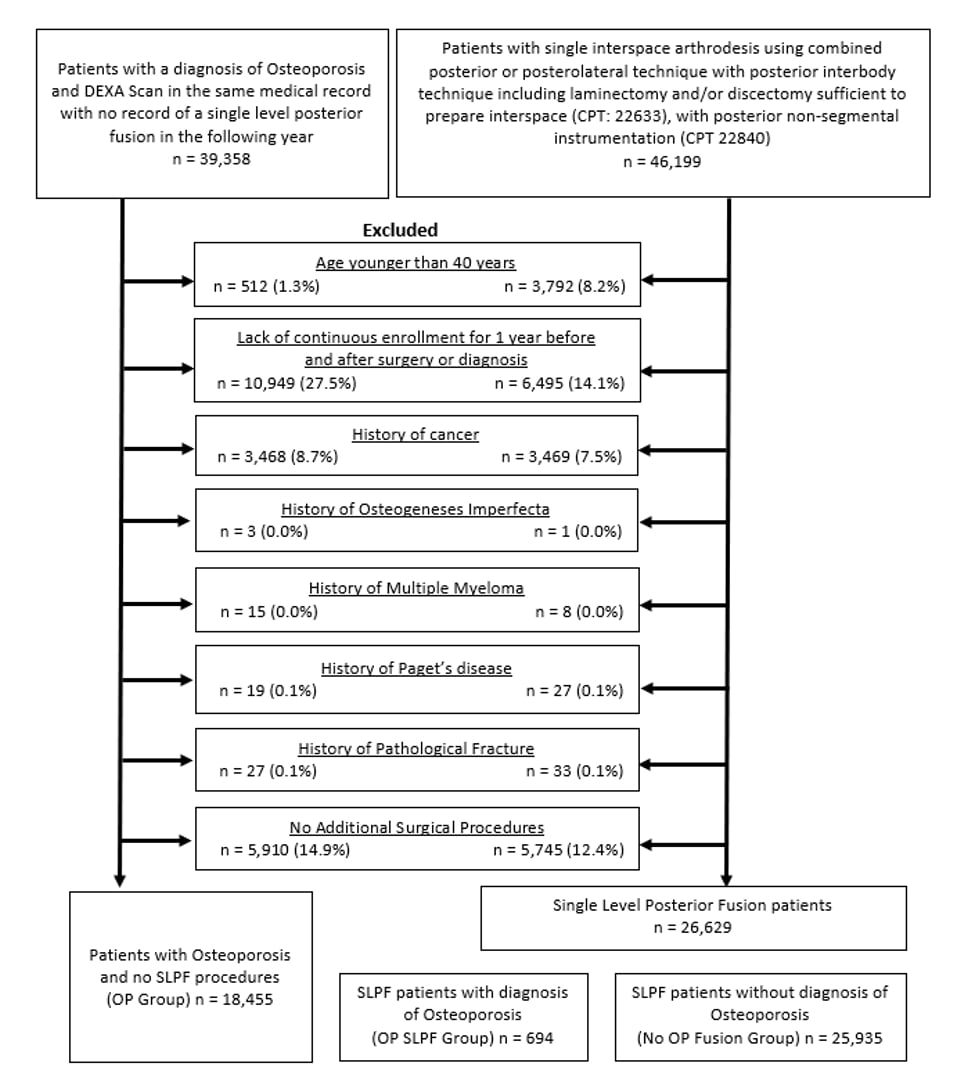 Figure 1: Flow chart for inclusion and exclusion criteria of the patient query.
Figure 1: Flow chart for inclusion and exclusion criteria of the patient query. 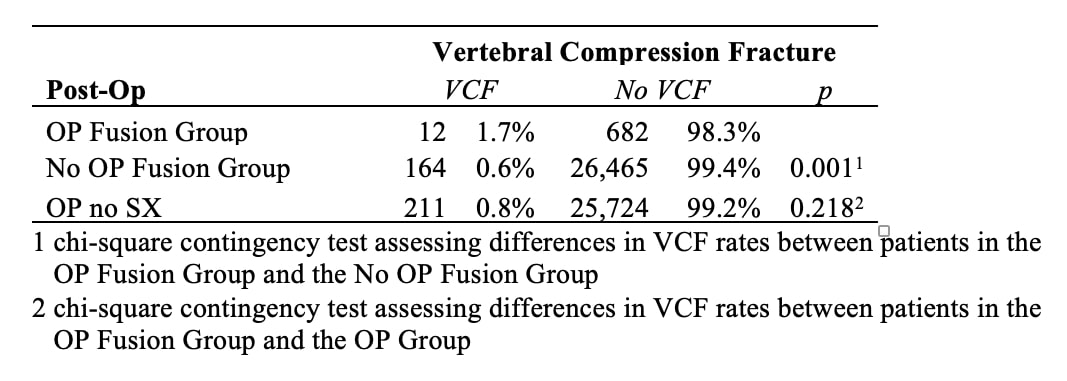 Table 1: Incidence of VCF among patients with osteoporosis underdoing SLPF.
Table 1: Incidence of VCF among patients with osteoporosis underdoing SLPF. 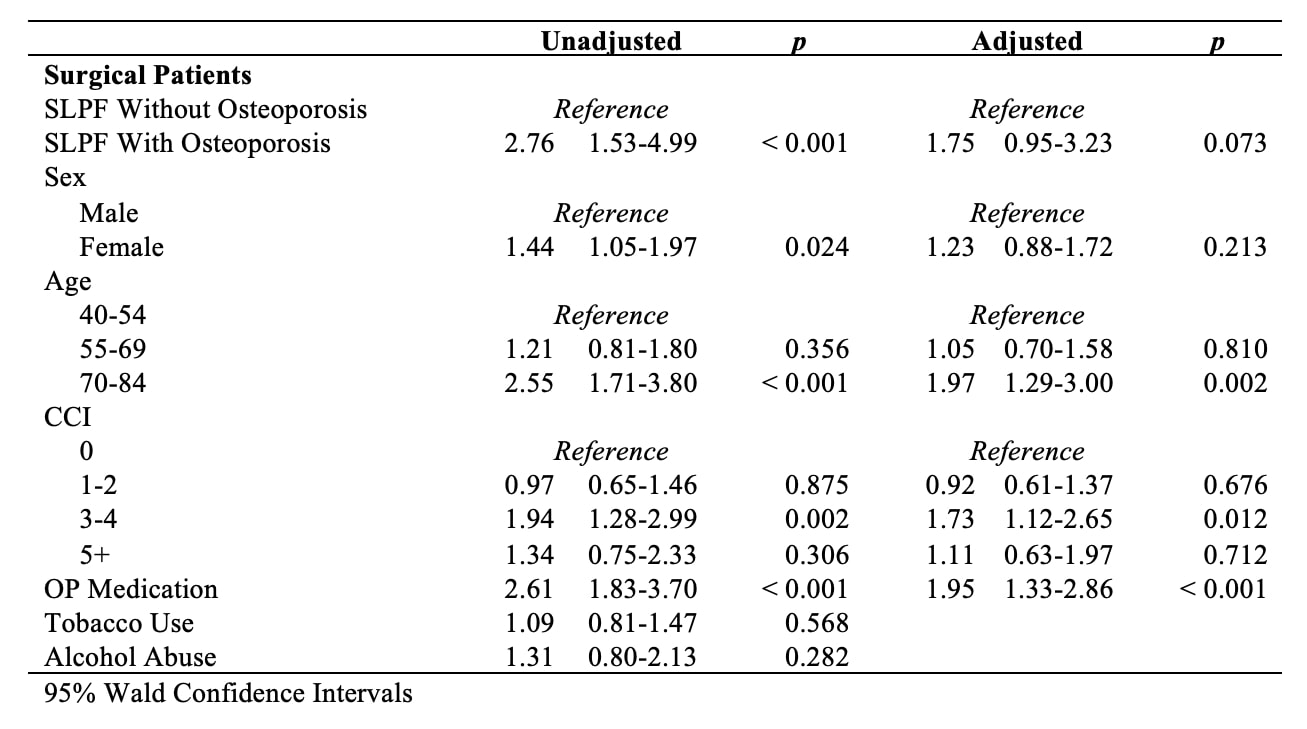 Table 2: Unadjusted and adjusted multivariate analysis for developing a VCF within the year after surgery.
Table 2: Unadjusted and adjusted multivariate analysis for developing a VCF within the year after surgery. Disclosures: V. Kesarwani, None; S. Esmende, None; R. Kostyun, None; M. Solomito, None; H. Makanji, None; J. Magaldi, None; M. Kumar, None.

