Back
Poster Session D
Osteoarthritis (OA) and related disorders
Session: (1888–1923) Osteoarthritis – Clinical Poster
1910: Evaluation of Dynamic Effects of Depressive Symptoms on Functional Outcomes in Knee Osteoarthritis
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- RM
Rhea Mehta, BA, MHS
University of Maryland, Baltimore
Baltimore, MD, United States
Abstract Poster Presenter(s)
Rhea Mehta1, Marc Hochberg2, Michelle Shardell1, Alice Ryan1, Yu Dong1, Brock Beamer1, Jason Peer2, Megan Schuler3, Joseph Gallo4, Elizabeth Stuart4 and Alan Rathbun1, 1University of Maryland, School of Medicine, Baltimore, MD, 2University of Maryland School of Medicine, Baltimore, MD, 3Rand Inc., Boston, MA, 4Johns Hopkins Bloomberg School of Public Health, Baltimore, MD
Background/Purpose: Knee OA is a leading cause of functional decline, and psychiatric comorbidity is common, particularly major depression. Depressive symptoms decrease physical activity and exacerbate functional disability, but depression is dynamic, and research has not assessed how these fluctuations affect functional outcomes as knee OA progresses. The study objective was to evaluate how changes in depressive symptoms affect functional outcomes among persons with radiographic knee OA (Figure 1).
Methods: Participants (n=2,212) from the Osteoarthritis Initiative (N=4,796) with radiographic knee OA (Kellgren-Lawrence grade ≥ 2 in one or both knees) and complete baseline data were included in the analytic sample. Depressive symptoms were assessed as a time-varying score using the Center for Epidemiological Studies Depression Scale (CES-D; range 0-60) at baseline and first three annual follow-up visits. Functional outcomes were measured at the first four annual follow-up visits and included gait speed and Physical Activity Scale for the Elderly (PASE). Outcome variables were standardized such that associations could be interpreted as differences in standard deviations per unit CES-D. Time-invariant confounders were measured at study enrollment and included demographic, socioeconomic, and lifestyle factors. Time-varying covariates were measured concurrent to CES-D scores and included BMI, pain, additional treatments, and other knee OA signs and symptoms. The primary method of analysis was marginal structural models that estimated main and time-specific effects of depressive symptoms on functional outcomes.
Results: There were significant main effects (Table 1) of depressive symptoms on both gait speed (β = -0.0045; 95% CI: -0.0080, -0.0011) and PASE (β = -0.0053; 95% CI: -0.0094, -0.0011) that indicated physical performance and physical activity were lower with higher CES-D scores. However, there was variability regarding the effects of depressive symptoms on functional outcomes (Figure 2) as evidenced by exposure-by-time interactions for the first to fourth follow-up interval for gait speed (P = 0.018) and first to second follow-up interval for PASE (P=0.055). The influence of depressive symptoms on gait speed declined over time from the first (β = -0.0079; 95% CI: -0.0125, -0.0032) to fourth (β = -0.0012; 95% CI: -0.0061, 0.0037) follow-up interval. Similarly, the association between depressive symptoms and PASE decreased from the first (β = -0.0086; 95% CI: -0.0141, -0.0030) to second (β = -0.0012; 95% CI: -0.0079, 0.0055) follow-up interval but then exhibited a reversion during the third and fourth follow-up intervals.
Conclusion: These findings imply that the negative effect of depressive symptoms on functional outcomes in knee OA decreases over time as structural and clinical knee OA progresses. Nonetheless, the significant effect of depressive symptoms on functional outcomes, particularly earlier in time, highlights the need for early intervention on comorbid depression in knee OA patients to prevent functional declines and maintain physical performance and activity during aging.
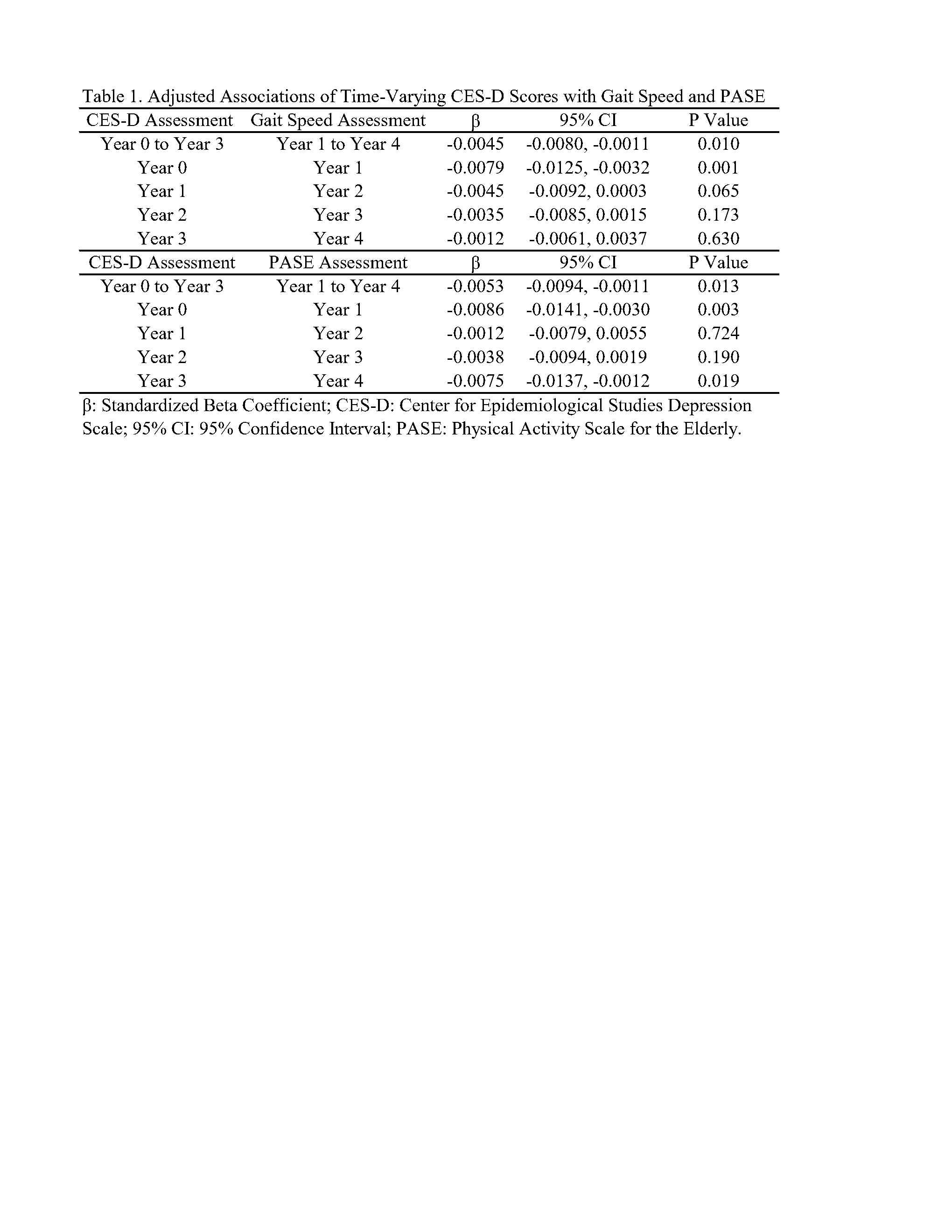
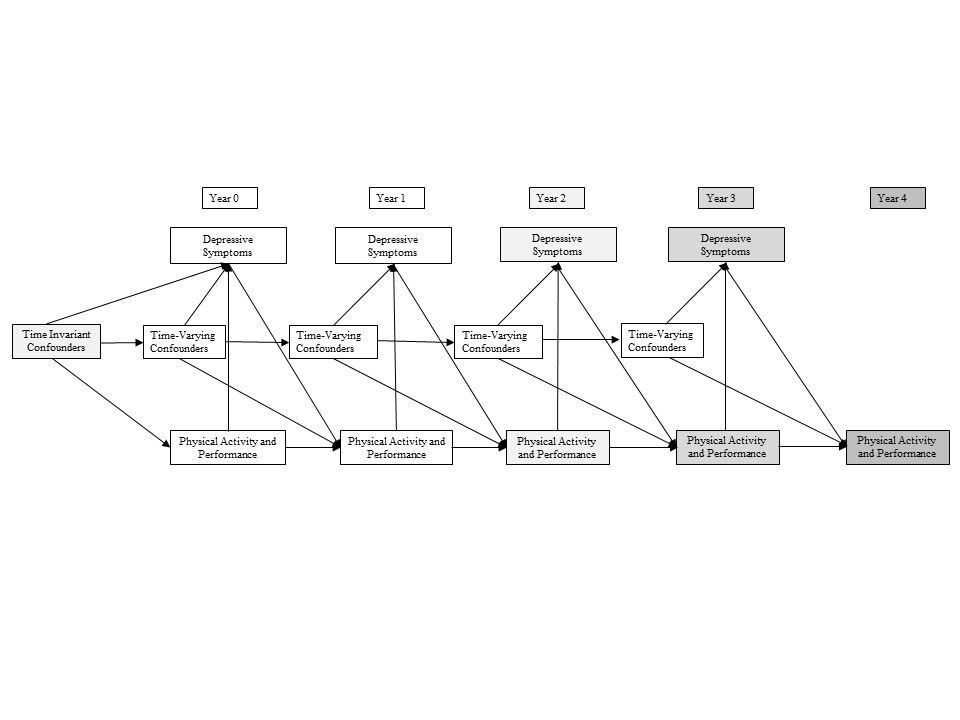 Figure 1. Directed Acyclic Graph Depicting the Epidemiological Study Design and Hypothesized Causal Relationships Between Depressive Symptoms, Functional Outcomes, Time-Invariant and Time-Varying Confounders
Figure 1. Directed Acyclic Graph Depicting the Epidemiological Study Design and Hypothesized Causal Relationships Between Depressive Symptoms, Functional Outcomes, Time-Invariant and Time-Varying Confounders
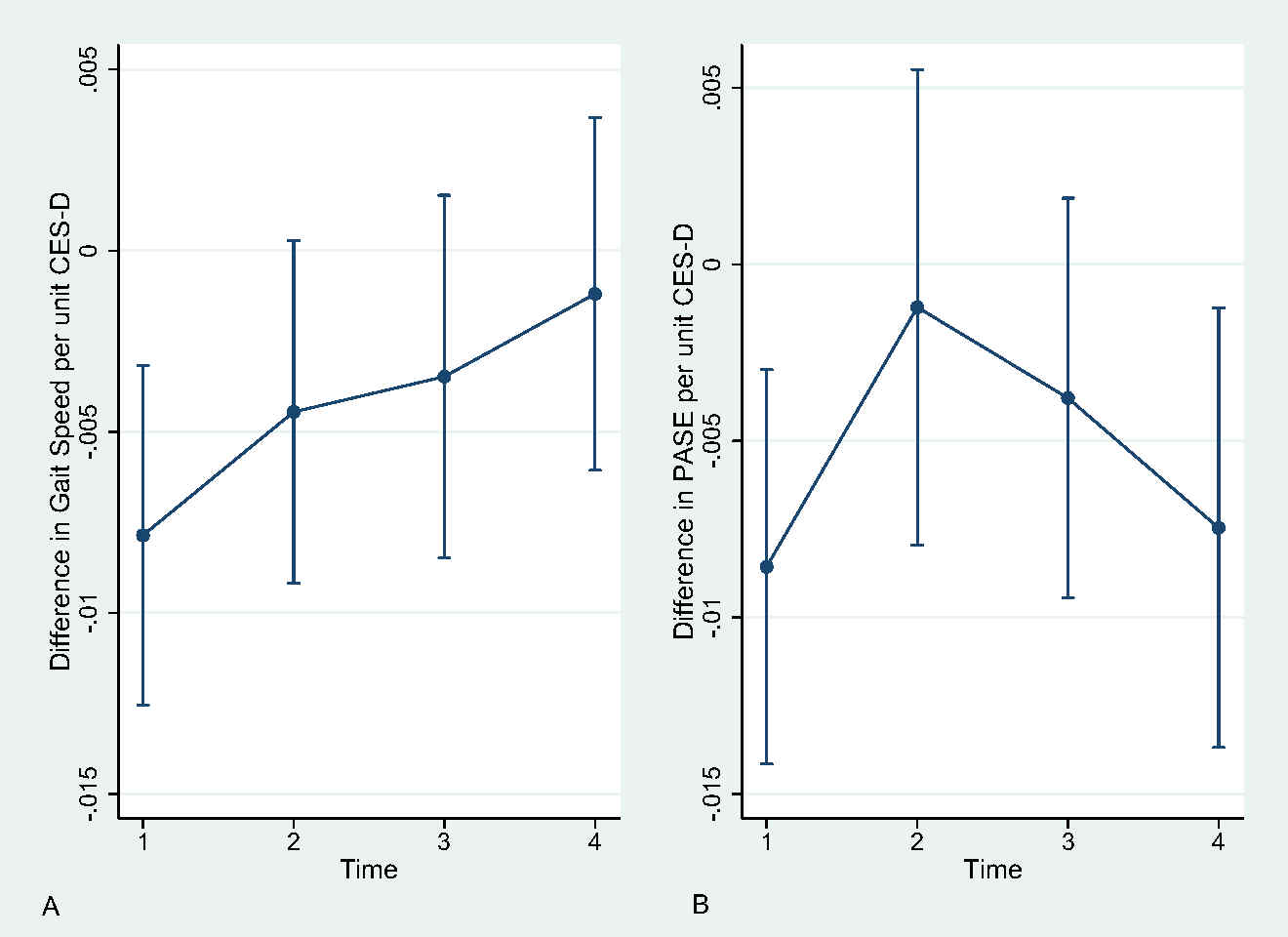 Figure 2. Average Marginal Effects of Time-Varying CES-D Scores on Standardized A) Gait Speed and B) PASE. CESD: Center for Epidemiological Studies Scale; PASE: Physical Activity Scale for the Elderly
Figure 2. Average Marginal Effects of Time-Varying CES-D Scores on Standardized A) Gait Speed and B) PASE. CESD: Center for Epidemiological Studies Scale; PASE: Physical Activity Scale for the Elderly
Disclosures: R. Mehta, None; M. Hochberg, None; M. Shardell, None; A. Ryan, None; Y. Dong, None; B. Beamer, None; J. Peer, None; M. Schuler, None; J. Gallo, None; E. Stuart, None; A. Rathbun, None.
Background/Purpose: Knee OA is a leading cause of functional decline, and psychiatric comorbidity is common, particularly major depression. Depressive symptoms decrease physical activity and exacerbate functional disability, but depression is dynamic, and research has not assessed how these fluctuations affect functional outcomes as knee OA progresses. The study objective was to evaluate how changes in depressive symptoms affect functional outcomes among persons with radiographic knee OA (Figure 1).
Methods: Participants (n=2,212) from the Osteoarthritis Initiative (N=4,796) with radiographic knee OA (Kellgren-Lawrence grade ≥ 2 in one or both knees) and complete baseline data were included in the analytic sample. Depressive symptoms were assessed as a time-varying score using the Center for Epidemiological Studies Depression Scale (CES-D; range 0-60) at baseline and first three annual follow-up visits. Functional outcomes were measured at the first four annual follow-up visits and included gait speed and Physical Activity Scale for the Elderly (PASE). Outcome variables were standardized such that associations could be interpreted as differences in standard deviations per unit CES-D. Time-invariant confounders were measured at study enrollment and included demographic, socioeconomic, and lifestyle factors. Time-varying covariates were measured concurrent to CES-D scores and included BMI, pain, additional treatments, and other knee OA signs and symptoms. The primary method of analysis was marginal structural models that estimated main and time-specific effects of depressive symptoms on functional outcomes.
Results: There were significant main effects (Table 1) of depressive symptoms on both gait speed (β = -0.0045; 95% CI: -0.0080, -0.0011) and PASE (β = -0.0053; 95% CI: -0.0094, -0.0011) that indicated physical performance and physical activity were lower with higher CES-D scores. However, there was variability regarding the effects of depressive symptoms on functional outcomes (Figure 2) as evidenced by exposure-by-time interactions for the first to fourth follow-up interval for gait speed (P = 0.018) and first to second follow-up interval for PASE (P=0.055). The influence of depressive symptoms on gait speed declined over time from the first (β = -0.0079; 95% CI: -0.0125, -0.0032) to fourth (β = -0.0012; 95% CI: -0.0061, 0.0037) follow-up interval. Similarly, the association between depressive symptoms and PASE decreased from the first (β = -0.0086; 95% CI: -0.0141, -0.0030) to second (β = -0.0012; 95% CI: -0.0079, 0.0055) follow-up interval but then exhibited a reversion during the third and fourth follow-up intervals.
Conclusion: These findings imply that the negative effect of depressive symptoms on functional outcomes in knee OA decreases over time as structural and clinical knee OA progresses. Nonetheless, the significant effect of depressive symptoms on functional outcomes, particularly earlier in time, highlights the need for early intervention on comorbid depression in knee OA patients to prevent functional declines and maintain physical performance and activity during aging.
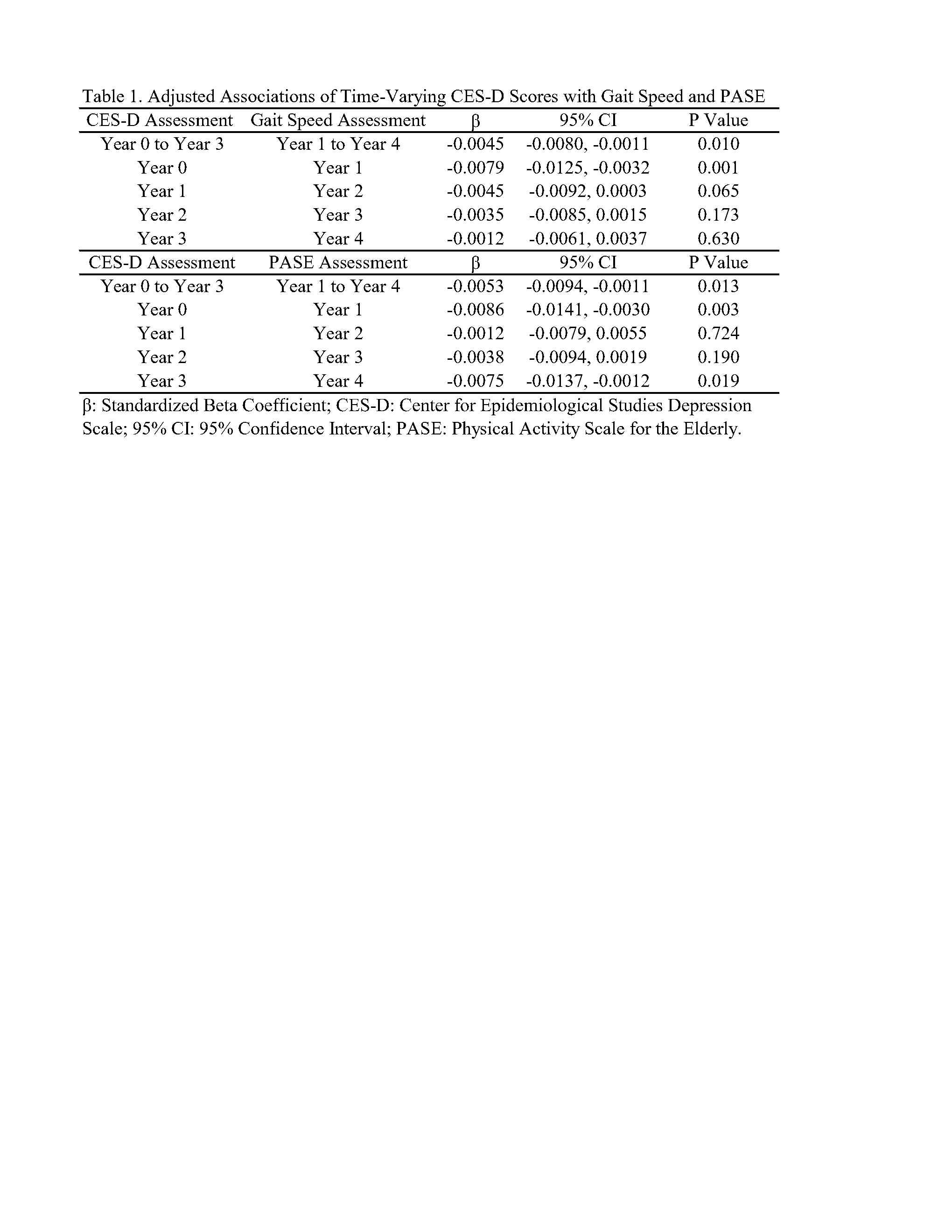
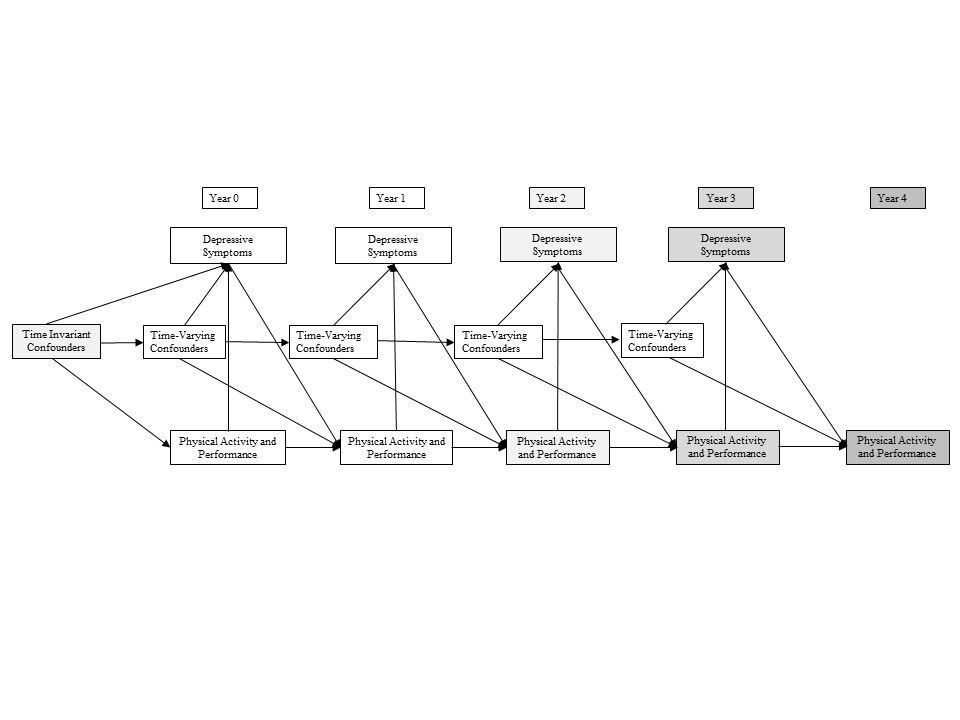 Figure 1. Directed Acyclic Graph Depicting the Epidemiological Study Design and Hypothesized Causal Relationships Between Depressive Symptoms, Functional Outcomes, Time-Invariant and Time-Varying Confounders
Figure 1. Directed Acyclic Graph Depicting the Epidemiological Study Design and Hypothesized Causal Relationships Between Depressive Symptoms, Functional Outcomes, Time-Invariant and Time-Varying Confounders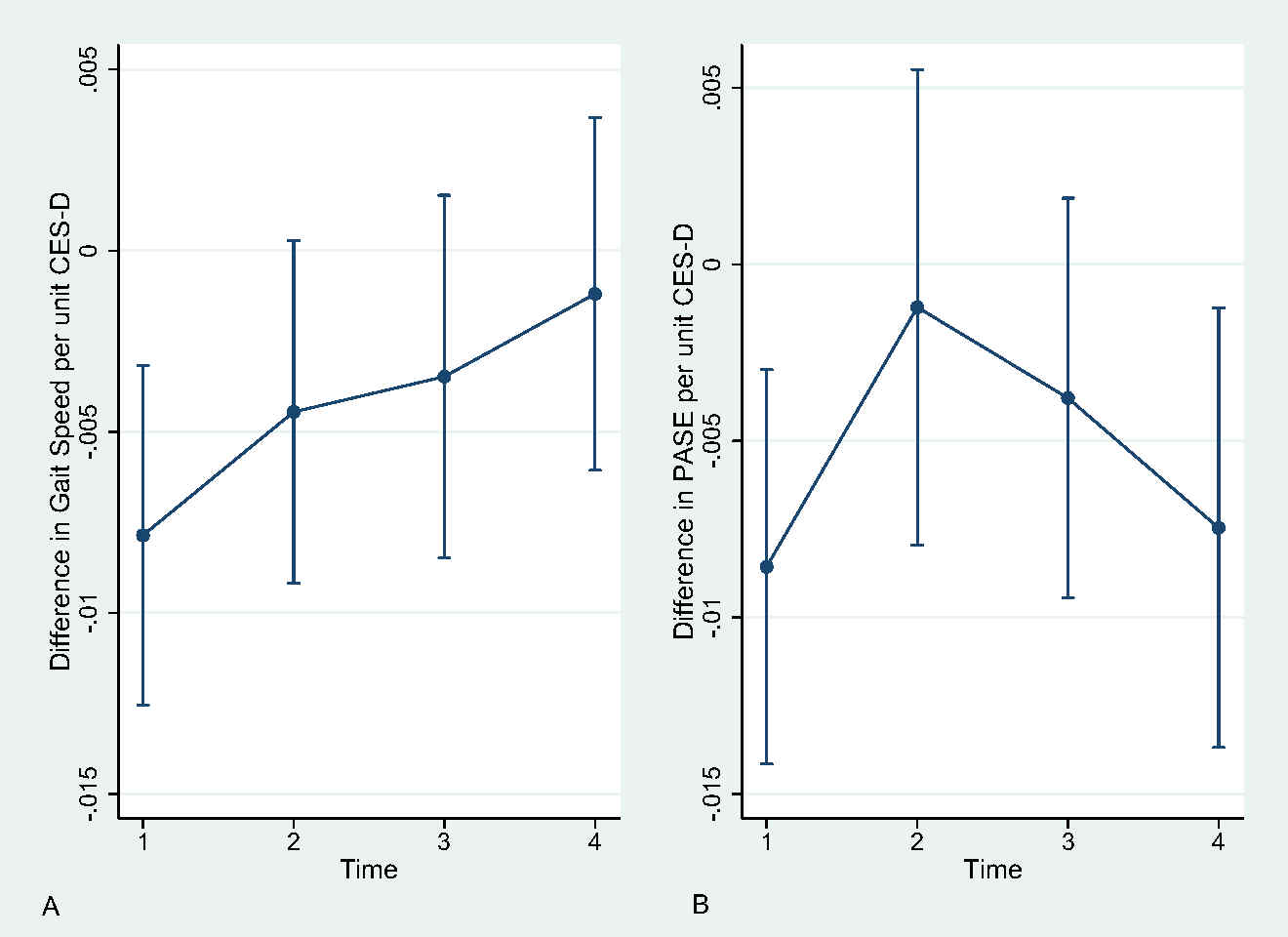 Figure 2. Average Marginal Effects of Time-Varying CES-D Scores on Standardized A) Gait Speed and B) PASE. CESD: Center for Epidemiological Studies Scale; PASE: Physical Activity Scale for the Elderly
Figure 2. Average Marginal Effects of Time-Varying CES-D Scores on Standardized A) Gait Speed and B) PASE. CESD: Center for Epidemiological Studies Scale; PASE: Physical Activity Scale for the ElderlyDisclosures: R. Mehta, None; M. Hochberg, None; M. Shardell, None; A. Ryan, None; Y. Dong, None; B. Beamer, None; J. Peer, None; M. Schuler, None; J. Gallo, None; E. Stuart, None; A. Rathbun, None.

