Back
Poster Session D
Session: (2052–2107) SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
2058: Evidence on the Construct Validity of the Perceived Deficits Questionnaire Among Adult Patients with Systemic Lupus Erythematosus
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall

Stefan Perera, MD, MSc
University of Toronto
Toronto, ON, Canada
Abstract Poster Presenter(s)
Stefan Perera1, Jiandong Su2, Kathleen Bingham3, Mahta Kakvan1, Maria Carmela Tartaglia4, Leslet Ruttan5, Joan Wither1, May Choi6, Simone Appenzeller7, Dorcas Beaton8, Dennisse Bonilla2, Patricia Katz9, Robin Green5, Michelle Barraclough10 and Zahi Touma2, 1Schroeder Arthritis Institute, Krembil Research Institute, University Health Network, University of Toronto, Toronto, ON, Canada, 2Schroeder Arthritis Institute, Krembil Research Institute, University Health Network and University of Toronto, Toronto, ON, Canada, 3Centre for Mental Health, University Health Network; Department of Psychiatry, University of Toronto, Toronto, ON, Canada, 4University of Toronto Krembil Neurosciences Centre, Toronto, ON, Canada, 5University Health Network-Toronto Rehabilitation Institute, Toronto, ON, Canada, 6Brigham and Women's Hospital | University of Calgary, Calgary, AB, Canada, 7Unicamp, Campinas, São Paulo, Brazil, 8Institute for Work & Health, Toronto, ON, Canada, 9UCSF, San Rafael, CA, 10Schroeder Arthritis Institute, Krembil Research Institute, University Health Network, Centre for Epidemiology Versus Arthritis, Division of Musculoskeletal and Dermatological Sciences, School of Biological Sciences, Faculty of Biology, Medicine and Health, The University of Manchester, NIHR Manchester Biomedical Research Centre, Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, Toronto, ON, Canada
Background/Purpose: Cognitive impairment (CI) is prevalent in SLE and negatively impacts social and occupational engagement. There is a need for a patient-reported outcome measure (PROM) of CI in SLE. The Perceived Deficits Questionnaire (PDQ) was created to assess perceived CI in multiple sclerosis. We assessed the concurrent construct validity of the PDQ as a PROM of CI among adult patients with SLE compared to: 1) an objective cognitive measure (ACR Neuropsychological Battery, ACR-NB) and 2) a subjective cognitive measure (Patient Reported Outcomes Measurement Information System (PROMIS) Computerized Adaptive Test (CAT) Cognitive Abilities and Concerns Scales).
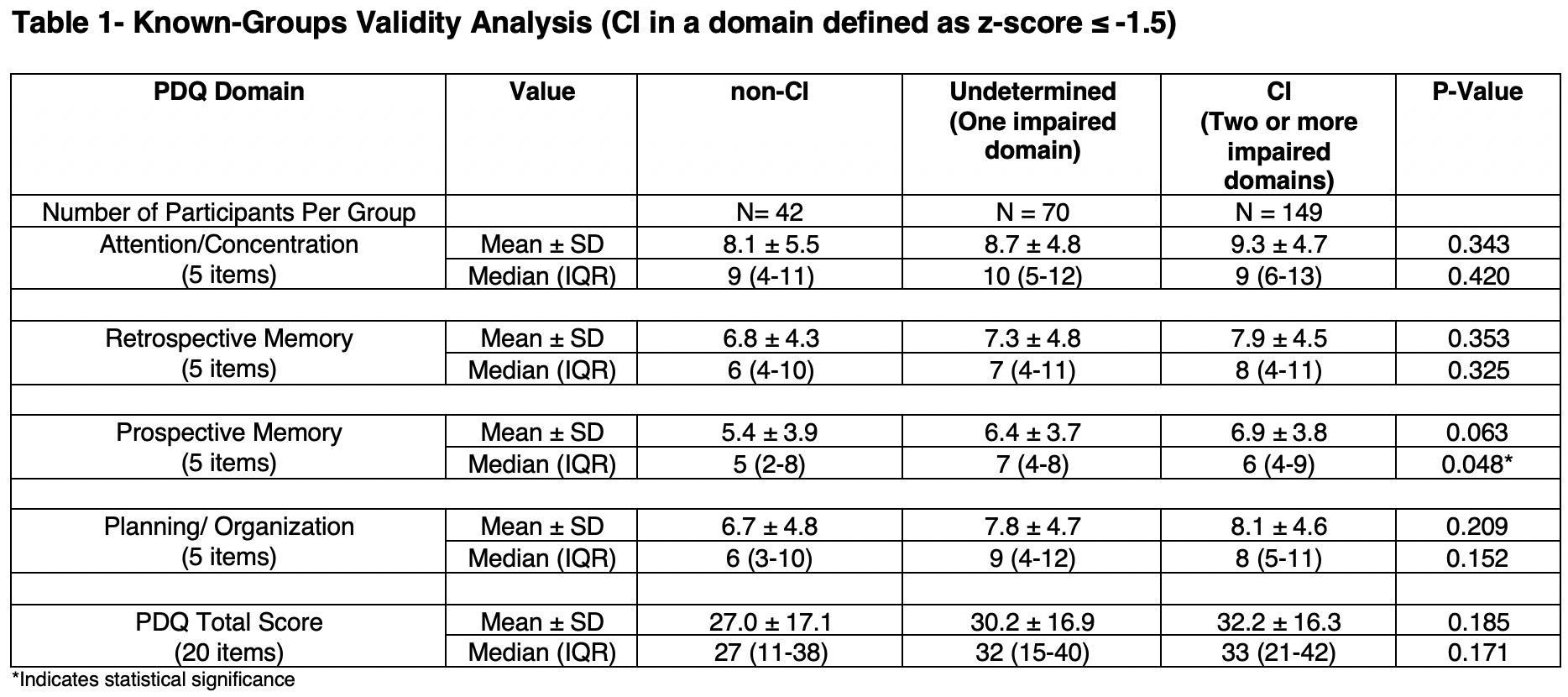
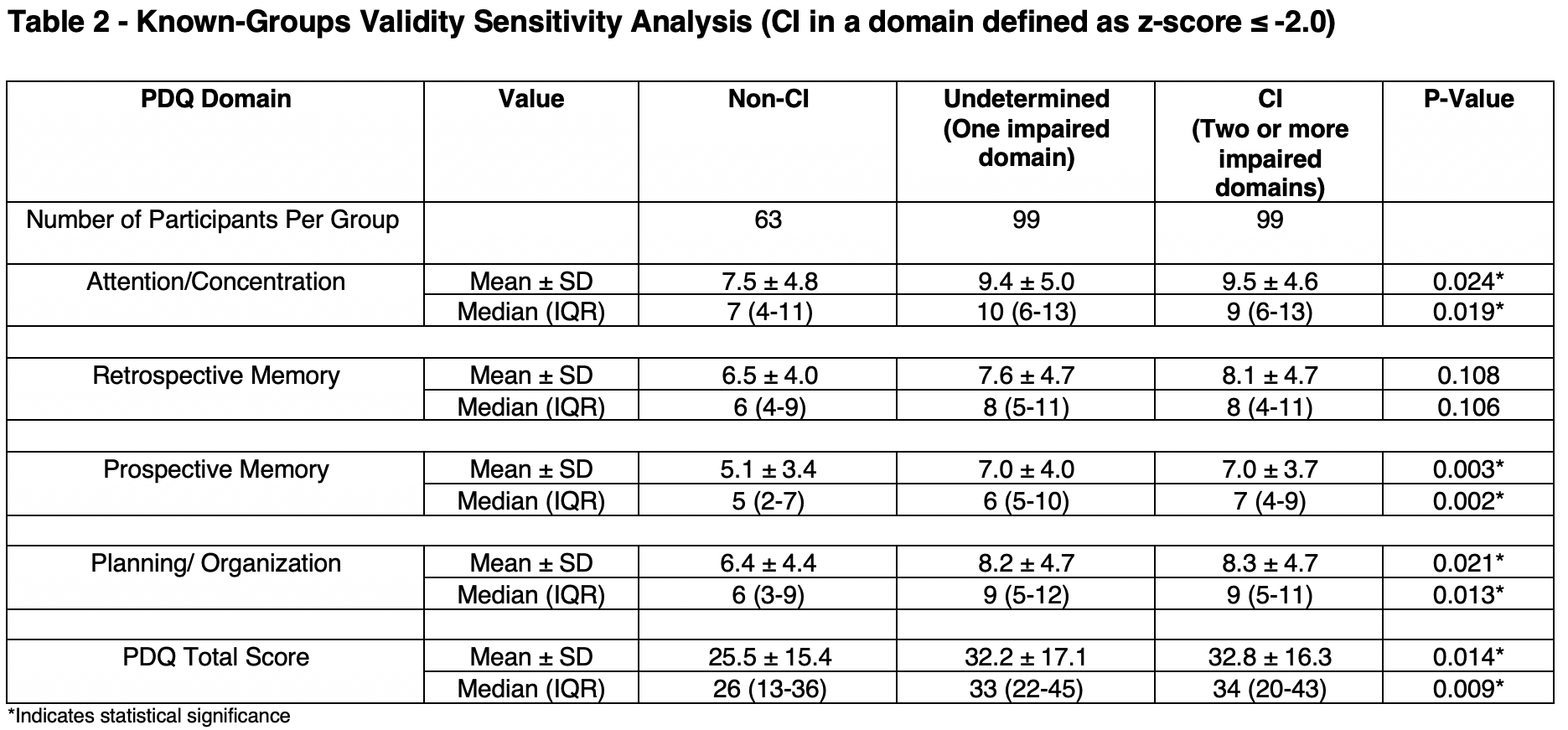
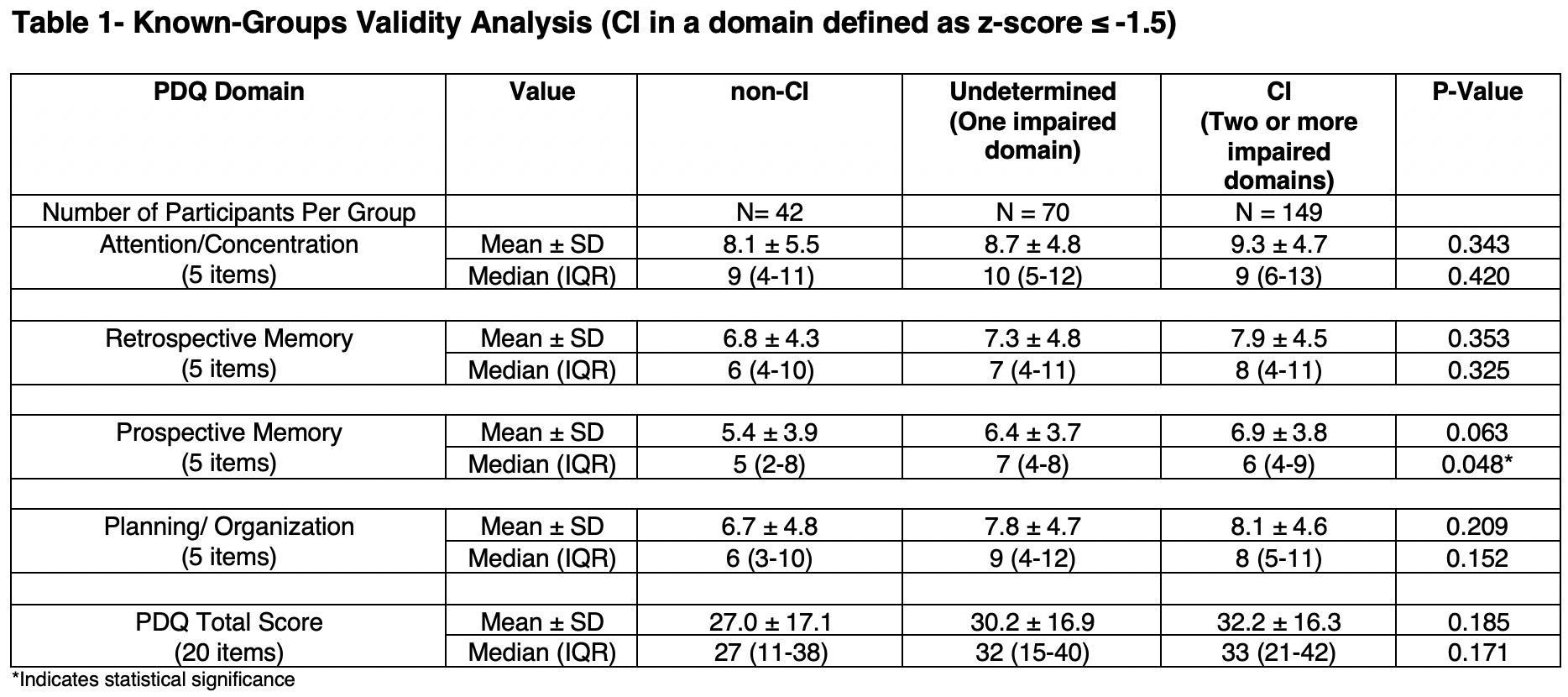
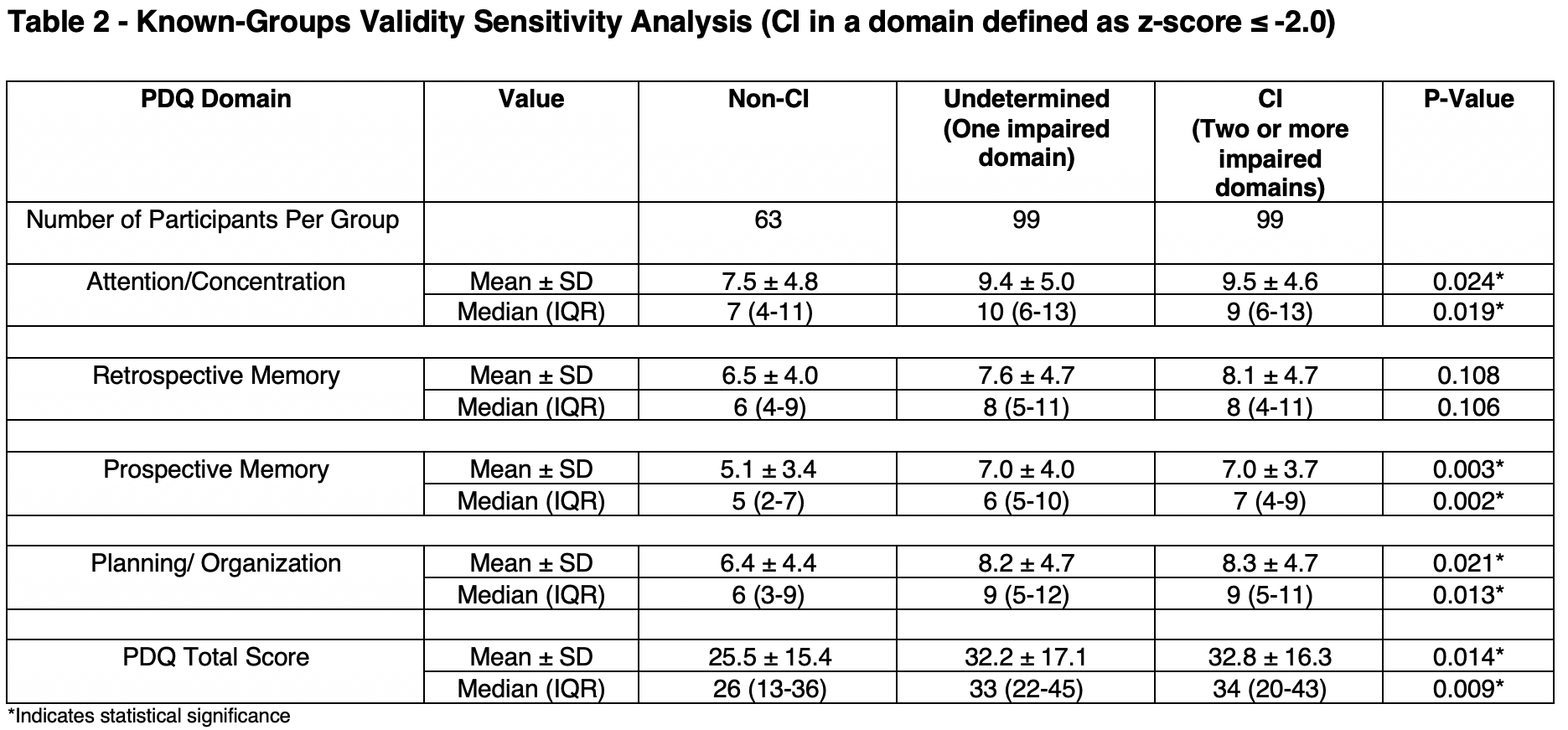
Methods: Participants included 261 English-speaking adults ≥ 18 years of age with SLE recruited from a single centre. All participants completed the PDQ which includes 4 subscale scores (attention/concentration, retrospective memory, prospective memory, planning/organization) and the ACR-NB. Known-Groups validity was assessed by dividing participants into 3 groups (non-CI, Undetermined, and CI) based on the ACR-NB and assessing whether the PDQ subscale scores differed significantly between groups in the expected direction. Groups were defined as follows: 1) non-CI (z-score of > -1.5 in all ACR-NB domains); 2) Undetermined, (z-score ≤ -1.5 in one ACR-NB domain); 3) CI, (z-score ≤ -1.5 in ≥ 2 ACR-NB domains). In the sensitivity analysis CI was defined as a z-score ≤ -2.0 in ≥ 2 ACR-NB domains. We hypothesized that the PDQ would be significantly different between the three CI groups (non-CI, undetermined and CI). ANOVA and Kruskal-Wallis analyses were performed. As a secondary analysis, 157 participants completed the PROMIS CAT Cognitive scales as a PROM comparator to the PDQ. The concurrent construct validity of PDQ compared to PROMIS CAT cognitive measures was assessed. We hypothesized that the PDQ would demonstrate strong correlation with each of the PROMIS cognitive measures, given that both are subjective measures. Spearman correlations between the PDQ total and subscale scores and the PROMIS CAT Cognitive scores were computed.
Results: The PDQ did not differ between the 3 groups when a z-score ≤ -1.5 was used (Table 1). While the mean and median PDQ scores were higher (reflecting worse perceived CI) in patients with objective CI compared to the other two groups, this did not reach statistical significance except for the median PDQ subscale of prospective memory. In the sensitivity analysis (Table 2), the mean and median PDQ scores were higher in patients with objective CI and reached statistical significance in total and all subscales except for the retrospective memory subscale. Secondary analyses demonstrated strong correlations between the PDQ total and subscale scores and the PROMIS CAT Cognitive scores (Table 3).
Conclusion: The results of this study provide evidence on the construct validity of the PDQ for the assessment of CI in adults patients with SLE. PDQ total and subscales scores were worse in patients with objective CI (ACR-NB), but only when using the more severe definition of CI. In addition, PDQ total and subscales scores were moderately-strongly associated with another subjective measure of CI, PROMIS CAT Cognitive measures.

Disclosures: S. Perera, None; J. Su, None; K. Bingham, None; M. Kakvan, None; M. Tartaglia, None; L. Ruttan, None; J. Wither, AstraZeneca, Pfizer; M. Choi, AstraZeneca, MitogenDx, mallinckrodt, Janssen, AbbVie/Abbott, Alimentiv, Amgen, AVIR Pharma Inc, BioJAMP, Bristol-Myers Squibb(BMS), Celltrion, Ferring, Fresenius Kabi, McKesson, Mylan, Takeda, Pendopharm, Pfizer, Roche; S. Appenzeller, None; D. Beaton, None; D. Bonilla, None; P. Katz, None; R. Green, None; M. Barraclough, None; Z. Touma, None.
Background/Purpose: Cognitive impairment (CI) is prevalent in SLE and negatively impacts social and occupational engagement. There is a need for a patient-reported outcome measure (PROM) of CI in SLE. The Perceived Deficits Questionnaire (PDQ) was created to assess perceived CI in multiple sclerosis. We assessed the concurrent construct validity of the PDQ as a PROM of CI among adult patients with SLE compared to: 1) an objective cognitive measure (ACR Neuropsychological Battery, ACR-NB) and 2) a subjective cognitive measure (Patient Reported Outcomes Measurement Information System (PROMIS) Computerized Adaptive Test (CAT) Cognitive Abilities and Concerns Scales).
Methods: Participants included 261 English-speaking adults ≥ 18 years of age with SLE recruited from a single centre. All participants completed the PDQ which includes 4 subscale scores (attention/concentration, retrospective memory, prospective memory, planning/organization) and the ACR-NB. Known-Groups validity was assessed by dividing participants into 3 groups (non-CI, Undetermined, and CI) based on the ACR-NB and assessing whether the PDQ subscale scores differed significantly between groups in the expected direction. Groups were defined as follows: 1) non-CI (z-score of > -1.5 in all ACR-NB domains); 2) Undetermined, (z-score ≤ -1.5 in one ACR-NB domain); 3) CI, (z-score ≤ -1.5 in ≥ 2 ACR-NB domains). In the sensitivity analysis CI was defined as a z-score ≤ -2.0 in ≥ 2 ACR-NB domains. We hypothesized that the PDQ would be significantly different between the three CI groups (non-CI, undetermined and CI). ANOVA and Kruskal-Wallis analyses were performed. As a secondary analysis, 157 participants completed the PROMIS CAT Cognitive scales as a PROM comparator to the PDQ. The concurrent construct validity of PDQ compared to PROMIS CAT cognitive measures was assessed. We hypothesized that the PDQ would demonstrate strong correlation with each of the PROMIS cognitive measures, given that both are subjective measures. Spearman correlations between the PDQ total and subscale scores and the PROMIS CAT Cognitive scores were computed.
Results: The PDQ did not differ between the 3 groups when a z-score ≤ -1.5 was used (Table 1). While the mean and median PDQ scores were higher (reflecting worse perceived CI) in patients with objective CI compared to the other two groups, this did not reach statistical significance except for the median PDQ subscale of prospective memory. In the sensitivity analysis (Table 2), the mean and median PDQ scores were higher in patients with objective CI and reached statistical significance in total and all subscales except for the retrospective memory subscale. Secondary analyses demonstrated strong correlations between the PDQ total and subscale scores and the PROMIS CAT Cognitive scores (Table 3).
Conclusion: The results of this study provide evidence on the construct validity of the PDQ for the assessment of CI in adults patients with SLE. PDQ total and subscales scores were worse in patients with objective CI (ACR-NB), but only when using the more severe definition of CI. In addition, PDQ total and subscales scores were moderately-strongly associated with another subjective measure of CI, PROMIS CAT Cognitive measures.

Disclosures: S. Perera, None; J. Su, None; K. Bingham, None; M. Kakvan, None; M. Tartaglia, None; L. Ruttan, None; J. Wither, AstraZeneca, Pfizer; M. Choi, AstraZeneca, MitogenDx, mallinckrodt, Janssen, AbbVie/Abbott, Alimentiv, Amgen, AVIR Pharma Inc, BioJAMP, Bristol-Myers Squibb(BMS), Celltrion, Ferring, Fresenius Kabi, McKesson, Mylan, Takeda, Pendopharm, Pfizer, Roche; S. Appenzeller, None; D. Beaton, None; D. Bonilla, None; P. Katz, None; R. Green, None; M. Barraclough, None; Z. Touma, None.

