Back
Poster Session D
Session: (2154–2178) Systemic Sclerosis and Related Disorders – Clinical Poster III
2159: Gastroesophageal Reflux Disease in an Australian Scleroderma Cohort - Associations and Effect of Treatment
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- AQ
Alannah Quinlivan, MBBS
St Vincent's Hospital Melbourne
Highett, Victoria, Australia
Abstract Poster Presenter(s)
Alannah Quinlivan1, Dennis Neuen2, Dylan Hansen3, Wendy Stevens3, Laura Ross4, Nava Ferdowsi3, Susanna Proudman5, Jenny Walker6, Jo Sahhar7, Gene-Siew Ngian8, Diane Apostolopoulos9, Lauren Host10, Gabor Major11, Kathleen Morrisroe3 and Mandana Nikpour12, 1St Vincent's Hospital Melbourne and the University of Melbourne, Melbourne, Australia, 2Liverpool Hospital, Sydney, Australia, 3St Vincent's Hospital Melbourne, Melbourne, Australia, 4The University of Melbourne at St. Vincent's Hospital, Brunswick, Australia, 5University of Adelaide, Medindie, Australia, 6Flinders Medical Centre, Flinders University, Daw Park, Australia, 7Monash Health, Melbourne, Australia, 8Melbourne Health, Northcote, Australia, 9Monash University, Melbourne, Australia, 10Fiona Stanley Hospital, London, United Kingdom, 11Hunter New England Health Service, Rankin Park - Newcastle, New South Wales, Australia, 12The University of Melbourne at St. Vincent's Hospital Melbourne, Melbourne, Australia
Background/Purpose: To investigate the association between gastroesophageal reflux disease (GORD) and interstitial lung disease (ILD) and determine the effect of GORD treatment on survival in Australian scleroderma (SSc) patients.
Methods: One thousand, six hundred and forty consecutive SSc patients from the Australian Scleroderma Cohort Study (ASCS) were included. Patients were considered to have GORD if they had reported reflux symptoms, had reflux oesophagitis (diagnosed on endoscopy) or were currently being treated with a proton pump inhibitor (PPI) or histamine 2 receptor antagonist (H2 ant). The association between the presence of GORD and demographic and SSc disease features (including presence of ILD) was evaluated. In patients with ILD, we evaluated the relationship between the presence of GORD and severity of ILD as well as time to development of ILD (from onset of first non-RP manifestation). Finally, we assessed the impact of treatment of GORD on survival in all SSc patients and in those with ILD.
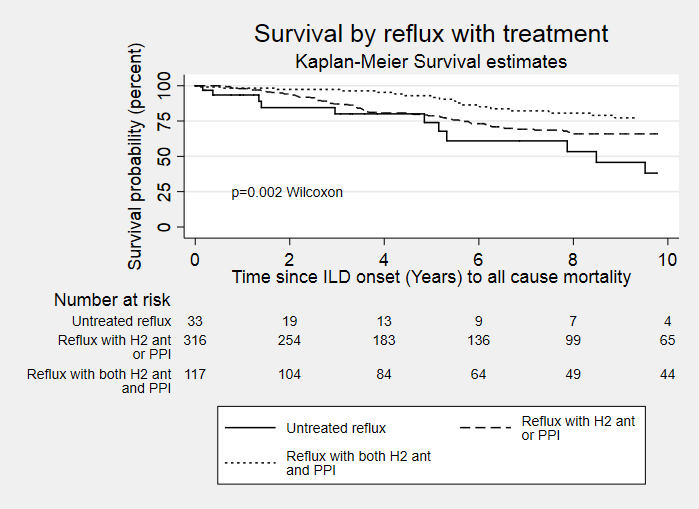
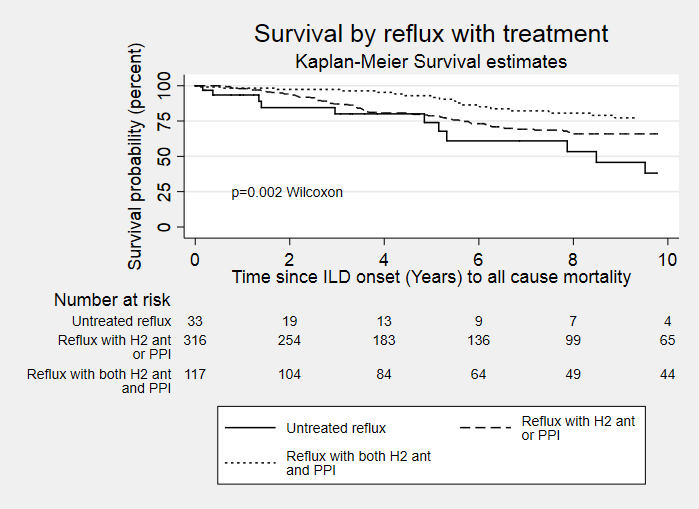
Results: GORD was a common manifestation in SSc affecting 93.8% of Australian SSc patients. Development of GORD was associated with longer SSc disease duration (p=0.001) but was not significantly associated with sex, disease subtype or autoantibody status. With regard to disease manifestations, GORD was significantly associated with digital ulcers, higher skin scores (defined using modified Rodnan skin score) and presence of joint contractures, sicca symptoms, faecal incontinence and need for hospitalisation (all p< 0.001). GORD was not significantly associated with PAH. With regard to ILD, there was no significant association between GORD and the presence of ILD, its severity, or the time to development of ILD. Treatment of GORD with anti-reflux medications (either PPI, H2 ant or combination) was associated with improved survival (HR 0.58, p = 0.006). Treatment of GORD did not delay the onset of ILD but was associated with improved overall survival in those with ILD (p=0.002). In patients with GORD and ILD, combination therapy with both PPI and H2 ant improved survival to a greater degree than monotherapy with either agent (Figure 1).
Conclusion: GORD is a common disease manifestation in SSc and its treatment improves survival in all patients, including those with ILD. While the presence or treatment of GORD does not influence the development of ILD, aggressive GORD treatment, ideally with combination therapy, improves survival in those with ILD.
Disclosures: A. Quinlivan, None; D. Neuen, None; D. Hansen, None; W. Stevens, None; L. Ross, None; N. Ferdowsi, None; S. Proudman, Jznssen; J. Walker, None; J. Sahhar, Boehringer-Ingelheim; G. Ngian, None; D. Apostolopoulos, None; L. Host, The limbic; G. Major, None; K. Morrisroe, None; M. Nikpour, Janssen, AstraZeneca, GlaxoSmithKlein(GSK), Boehringer-Ingelheim, Bristol-Myers Squibb(BMS).
Background/Purpose: To investigate the association between gastroesophageal reflux disease (GORD) and interstitial lung disease (ILD) and determine the effect of GORD treatment on survival in Australian scleroderma (SSc) patients.
Methods: One thousand, six hundred and forty consecutive SSc patients from the Australian Scleroderma Cohort Study (ASCS) were included. Patients were considered to have GORD if they had reported reflux symptoms, had reflux oesophagitis (diagnosed on endoscopy) or were currently being treated with a proton pump inhibitor (PPI) or histamine 2 receptor antagonist (H2 ant). The association between the presence of GORD and demographic and SSc disease features (including presence of ILD) was evaluated. In patients with ILD, we evaluated the relationship between the presence of GORD and severity of ILD as well as time to development of ILD (from onset of first non-RP manifestation). Finally, we assessed the impact of treatment of GORD on survival in all SSc patients and in those with ILD.
Results: GORD was a common manifestation in SSc affecting 93.8% of Australian SSc patients. Development of GORD was associated with longer SSc disease duration (p=0.001) but was not significantly associated with sex, disease subtype or autoantibody status. With regard to disease manifestations, GORD was significantly associated with digital ulcers, higher skin scores (defined using modified Rodnan skin score) and presence of joint contractures, sicca symptoms, faecal incontinence and need for hospitalisation (all p< 0.001). GORD was not significantly associated with PAH. With regard to ILD, there was no significant association between GORD and the presence of ILD, its severity, or the time to development of ILD. Treatment of GORD with anti-reflux medications (either PPI, H2 ant or combination) was associated with improved survival (HR 0.58, p = 0.006). Treatment of GORD did not delay the onset of ILD but was associated with improved overall survival in those with ILD (p=0.002). In patients with GORD and ILD, combination therapy with both PPI and H2 ant improved survival to a greater degree than monotherapy with either agent (Figure 1).
Conclusion: GORD is a common disease manifestation in SSc and its treatment improves survival in all patients, including those with ILD. While the presence or treatment of GORD does not influence the development of ILD, aggressive GORD treatment, ideally with combination therapy, improves survival in those with ILD.
Disclosures: A. Quinlivan, None; D. Neuen, None; D. Hansen, None; W. Stevens, None; L. Ross, None; N. Ferdowsi, None; S. Proudman, Jznssen; J. Walker, None; J. Sahhar, Boehringer-Ingelheim; G. Ngian, None; D. Apostolopoulos, None; L. Host, The limbic; G. Major, None; K. Morrisroe, None; M. Nikpour, Janssen, AstraZeneca, GlaxoSmithKlein(GSK), Boehringer-Ingelheim, Bristol-Myers Squibb(BMS).

