Back
Abstract Session
Pediatric autoimmune diseases: Kawasaki disease, juvenile dermatomyositis and juvenile localized scleroderma
Session: Abstracts: Pediatric Rheumatology – Clinical I: Connective Tissue Disease (0512–0517)
0517: Cortical Surface Area Correlates with Cognitive Efficiency and Disease Measures in Childhood-Onset Systemic Lupus Erythematosus
Saturday, November 12, 2022
4:15 PM – 4:25 PM Eastern Time
Location: Room 126

Santiago Arciniegas, BSc
University of Toronto
Toronto, ON, Canada
Presenting Author(s)
Santiago Arciniegas1, Sarah Mossad2, Tala El Tal3, Victoria Lishak4, Stephanie Fevrier5, Ibrahim Mohamed6, Joanna Law2, Lawrence Ng2, Paris Moaf2, Helen Branson2, Adrienne Davis2, Linda Hiraki7, Deborah Levy8, ashley Danguecan2, George Ibrahim5 and Andrea Knight3, 1University of Toronto/Hospital for Sick Children, Toronto, ON, Canada, 2The Hospital for Sick Children, Toronto, ON, Canada, 3The Hospital for Sick Children, Division of Rheumatology, Department of Paediatrics, University of Toronto, Toronto, ON, Canada, 4The Hospital for Sick Children, Department of Psychology, University of Toronto, Toronto, ON, Canada, 5The Hospital for Sick Children/University of Toronto, Toronto, ON, Canada, 6The Hospital for Sick Children, Neurosciences and Mental Health, Research Institute, ON, Canada 3Institute of Biomedical Engineering, University of Toronto, Brampton, ON, Canada, 7The Hospital for Sick Children, Division of Rheumatology, Department of Paediatrics, University of Toronto, Genetics and Genome Biology, SickKids Research Institute, Toronto, ON, Canada, 8Division of Rheumatology, The Hospital for Sick Children; Child Health Evaluative Services, SickKids Research Institute; Department of Paediatrics, University of Toronto, Toronto, ON, Canada
Background/Purpose: Cognitive difficulties are common in children with childhood-onset SLE (cSLE), but neuropsychiatric lupus (NPSLE) remains challenging to diagnose and treat. To increase understanding of underlying mechanisms, we examined the association of cortical surface area with cognitive performance and disease measures.
Methods: We examined a cross-sectional sample of patients with cSLE (ages 12-17) meeting ACR, SLICC or EULAR classification criteria and healthy controls (ages 12-17). Demographic and disease measures were collected from questionnaires and medical records, respectively. Subjects completed standardized cognitive tests on attention, executive function, and processing speed. We explored group differences using t-tests for each score. T1-weighted brain magnetic resonance images were obtained using a 3T scanner. The FreeSurfer software package was used to build cortical surface area maps for each subject. We probed structural differences between groups using a vertex-wise general linear model controlled for subject age and corrected for multiple comparisons. From this whole-brain analysis, only regions of interest (ROIs) showing significant group differences were considered for further analysis. We then examined the association between the surface area of each significant ROI and each cognitive task with significant group differences, using the Spearman correlation coefficient corrected for multiple comparisons. In the cSLE group, we used Partial Least-Squares Regression (PLS) to examine the association between disease measures and surface area in the significant ROIs.
Results: We recruited 30 patients with cSLE and 18 healthy controls; only one patient had a NPSLE diagnosis (Table 1). On average, lupus patients and controls scored within the normal range across cognitive tests. However, lupus patients performed worse than controls on measures of cognitive efficiency (attention reaction time p=0.056, processing speed colour naming p=0.02) (Fig. 1). Lupus patients were found to have a significantly reduced cortical surface area across 14 different ROIs when compared to controls (pcorr < 0.05), mostly in the right temporal and frontal lobes (Fig. 2). Brain-behaviour correlations suggest that reaction time is correlated with altered surface area in the left precentral area (pcorr=0.045), the right superior temporal gyrus (pcorr=0.046), post-cingulate gyrus (pcorr=0.042), the right middle frontal gyrus (pcorr=0.05) and the right intraparietal area (pcorr=0.056). In PLS analysis, cumulative steroid dose, and levels of CRP, ESR, and anti-dsDNA were found to be significant predictors of surface area.
Conclusion: Lupus patients exhibited cortical surface area abnormalities when compared to controls and performed worse on measures of cognitive efficiency. Structural abnormalities and poor cognitive efficiency were significantly associated. Cumulative steroid dose, CRP, ESR and anti-dsDNA were found to be significant predictors of brain surface area. Our findings suggest a relationship between disease activity, cortical surface area, and cognitive efficiency in patients with cSLE. Further study is needed to characterize the underlying mechanisms of this relationship.
.jpg) Table 1. All variables listed under Disease Measures were used in PLS Analysis, except for the “NPSLE diagnosis” variable.
Table 1. All variables listed under Disease Measures were used in PLS Analysis, except for the “NPSLE diagnosis” variable.
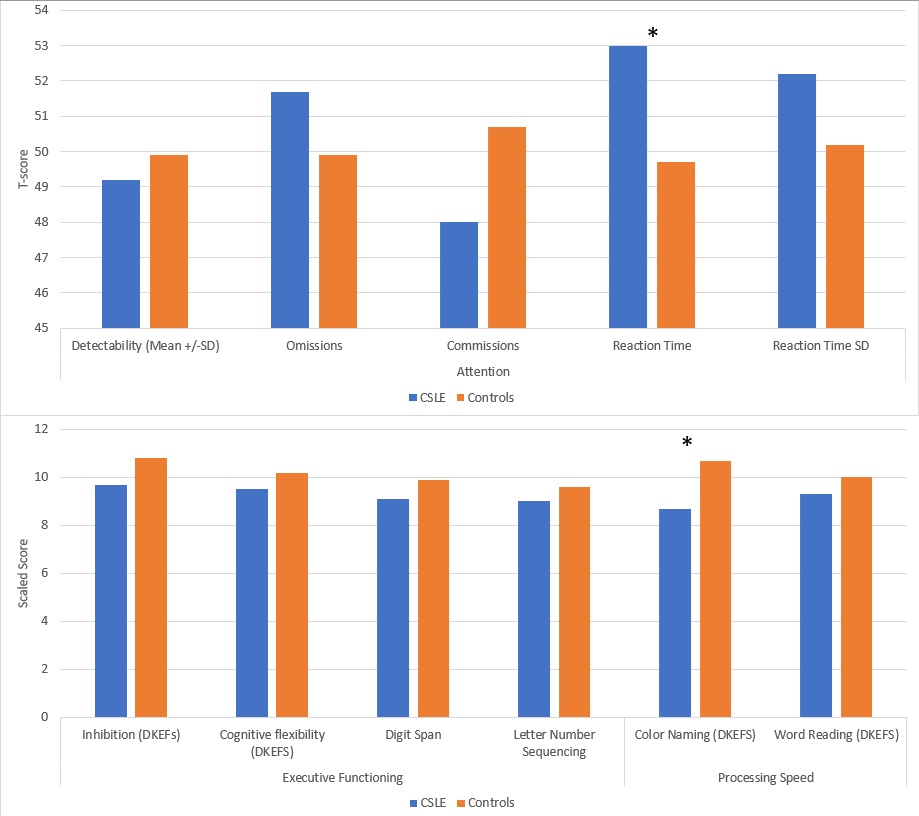 Figure 1. Mean scores of patients with cSLE (n=30) and healthy controls (n=18). An asterisk (*) represents statistically significant group differences for a particular measure (p < 0.05). Attention was measured by the Conners’ Continuous Performance Task III via standardized T scores (normative mean of 50, standard deviation of 10); higher scores indicate more difficulties. Measures of executive functioning and processing speed were measured by the Delis-Kaplan Executive Function System (D-KEFS, normative mean of 10, standard deviation of 3); lower scores indicate more difficulties.
Figure 1. Mean scores of patients with cSLE (n=30) and healthy controls (n=18). An asterisk (*) represents statistically significant group differences for a particular measure (p < 0.05). Attention was measured by the Conners’ Continuous Performance Task III via standardized T scores (normative mean of 50, standard deviation of 10); higher scores indicate more difficulties. Measures of executive functioning and processing speed were measured by the Delis-Kaplan Executive Function System (D-KEFS, normative mean of 10, standard deviation of 3); lower scores indicate more difficulties.
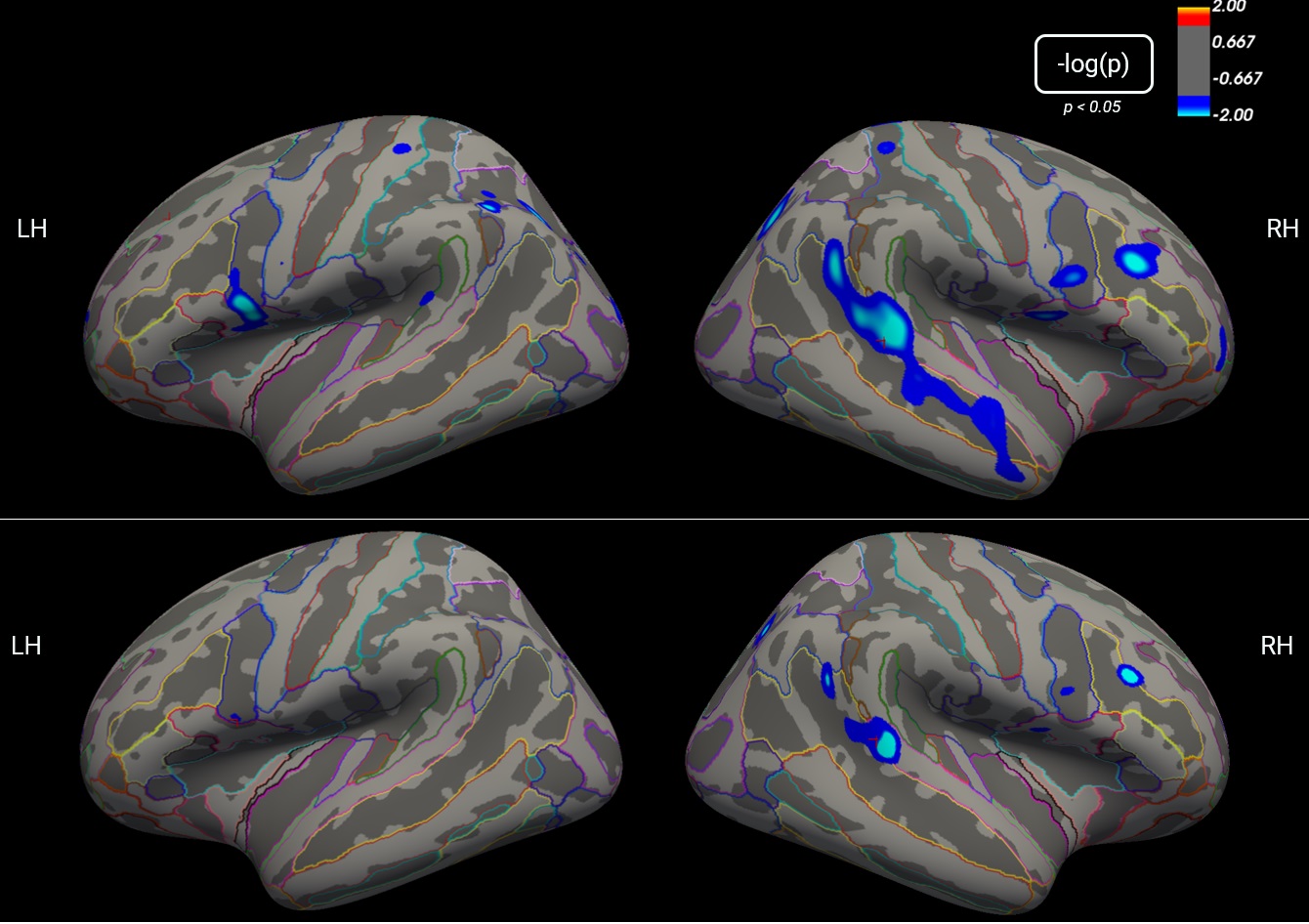 Figure 2. Cortical maps representing vertex-wise differences in surface area between patients with cSLE (n=30), and age/sex-matched controls (n=18). Blue colour indicates regions with statistically significant decreases in surface area in the cSLE group when compared to controls (p < 0.05). Coloured outlines annotate brain regions according to the Destrieux atlas. The top and bottom panels represent structural results before and after correcting for multiple comparisons, respectively.
Figure 2. Cortical maps representing vertex-wise differences in surface area between patients with cSLE (n=30), and age/sex-matched controls (n=18). Blue colour indicates regions with statistically significant decreases in surface area in the cSLE group when compared to controls (p < 0.05). Coloured outlines annotate brain regions according to the Destrieux atlas. The top and bottom panels represent structural results before and after correcting for multiple comparisons, respectively.
Disclosures: S. Arciniegas, None; S. Mossad, None; T. El Tal, None; V. Lishak, None; S. Fevrier, None; I. Mohamed, None; J. Law, None; L. Ng, None; P. Moaf, None; H. Branson, None; A. Davis, None; L. Hiraki, None; D. Levy, None; a. Danguecan, None; G. Ibrahim, None; A. Knight, None.
Background/Purpose: Cognitive difficulties are common in children with childhood-onset SLE (cSLE), but neuropsychiatric lupus (NPSLE) remains challenging to diagnose and treat. To increase understanding of underlying mechanisms, we examined the association of cortical surface area with cognitive performance and disease measures.
Methods: We examined a cross-sectional sample of patients with cSLE (ages 12-17) meeting ACR, SLICC or EULAR classification criteria and healthy controls (ages 12-17). Demographic and disease measures were collected from questionnaires and medical records, respectively. Subjects completed standardized cognitive tests on attention, executive function, and processing speed. We explored group differences using t-tests for each score. T1-weighted brain magnetic resonance images were obtained using a 3T scanner. The FreeSurfer software package was used to build cortical surface area maps for each subject. We probed structural differences between groups using a vertex-wise general linear model controlled for subject age and corrected for multiple comparisons. From this whole-brain analysis, only regions of interest (ROIs) showing significant group differences were considered for further analysis. We then examined the association between the surface area of each significant ROI and each cognitive task with significant group differences, using the Spearman correlation coefficient corrected for multiple comparisons. In the cSLE group, we used Partial Least-Squares Regression (PLS) to examine the association between disease measures and surface area in the significant ROIs.
Results: We recruited 30 patients with cSLE and 18 healthy controls; only one patient had a NPSLE diagnosis (Table 1). On average, lupus patients and controls scored within the normal range across cognitive tests. However, lupus patients performed worse than controls on measures of cognitive efficiency (attention reaction time p=0.056, processing speed colour naming p=0.02) (Fig. 1). Lupus patients were found to have a significantly reduced cortical surface area across 14 different ROIs when compared to controls (pcorr < 0.05), mostly in the right temporal and frontal lobes (Fig. 2). Brain-behaviour correlations suggest that reaction time is correlated with altered surface area in the left precentral area (pcorr=0.045), the right superior temporal gyrus (pcorr=0.046), post-cingulate gyrus (pcorr=0.042), the right middle frontal gyrus (pcorr=0.05) and the right intraparietal area (pcorr=0.056). In PLS analysis, cumulative steroid dose, and levels of CRP, ESR, and anti-dsDNA were found to be significant predictors of surface area.
Conclusion: Lupus patients exhibited cortical surface area abnormalities when compared to controls and performed worse on measures of cognitive efficiency. Structural abnormalities and poor cognitive efficiency were significantly associated. Cumulative steroid dose, CRP, ESR and anti-dsDNA were found to be significant predictors of brain surface area. Our findings suggest a relationship between disease activity, cortical surface area, and cognitive efficiency in patients with cSLE. Further study is needed to characterize the underlying mechanisms of this relationship.
.jpg) Table 1. All variables listed under Disease Measures were used in PLS Analysis, except for the “NPSLE diagnosis” variable.
Table 1. All variables listed under Disease Measures were used in PLS Analysis, except for the “NPSLE diagnosis” variable.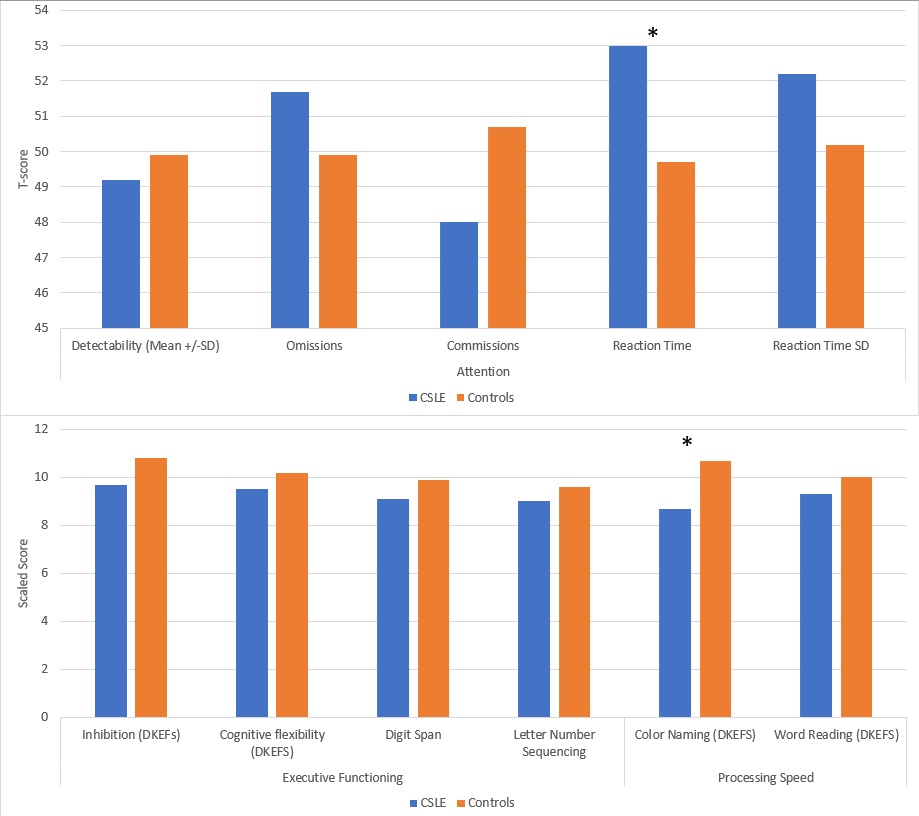 Figure 1. Mean scores of patients with cSLE (n=30) and healthy controls (n=18). An asterisk (*) represents statistically significant group differences for a particular measure (p < 0.05). Attention was measured by the Conners’ Continuous Performance Task III via standardized T scores (normative mean of 50, standard deviation of 10); higher scores indicate more difficulties. Measures of executive functioning and processing speed were measured by the Delis-Kaplan Executive Function System (D-KEFS, normative mean of 10, standard deviation of 3); lower scores indicate more difficulties.
Figure 1. Mean scores of patients with cSLE (n=30) and healthy controls (n=18). An asterisk (*) represents statistically significant group differences for a particular measure (p < 0.05). Attention was measured by the Conners’ Continuous Performance Task III via standardized T scores (normative mean of 50, standard deviation of 10); higher scores indicate more difficulties. Measures of executive functioning and processing speed were measured by the Delis-Kaplan Executive Function System (D-KEFS, normative mean of 10, standard deviation of 3); lower scores indicate more difficulties.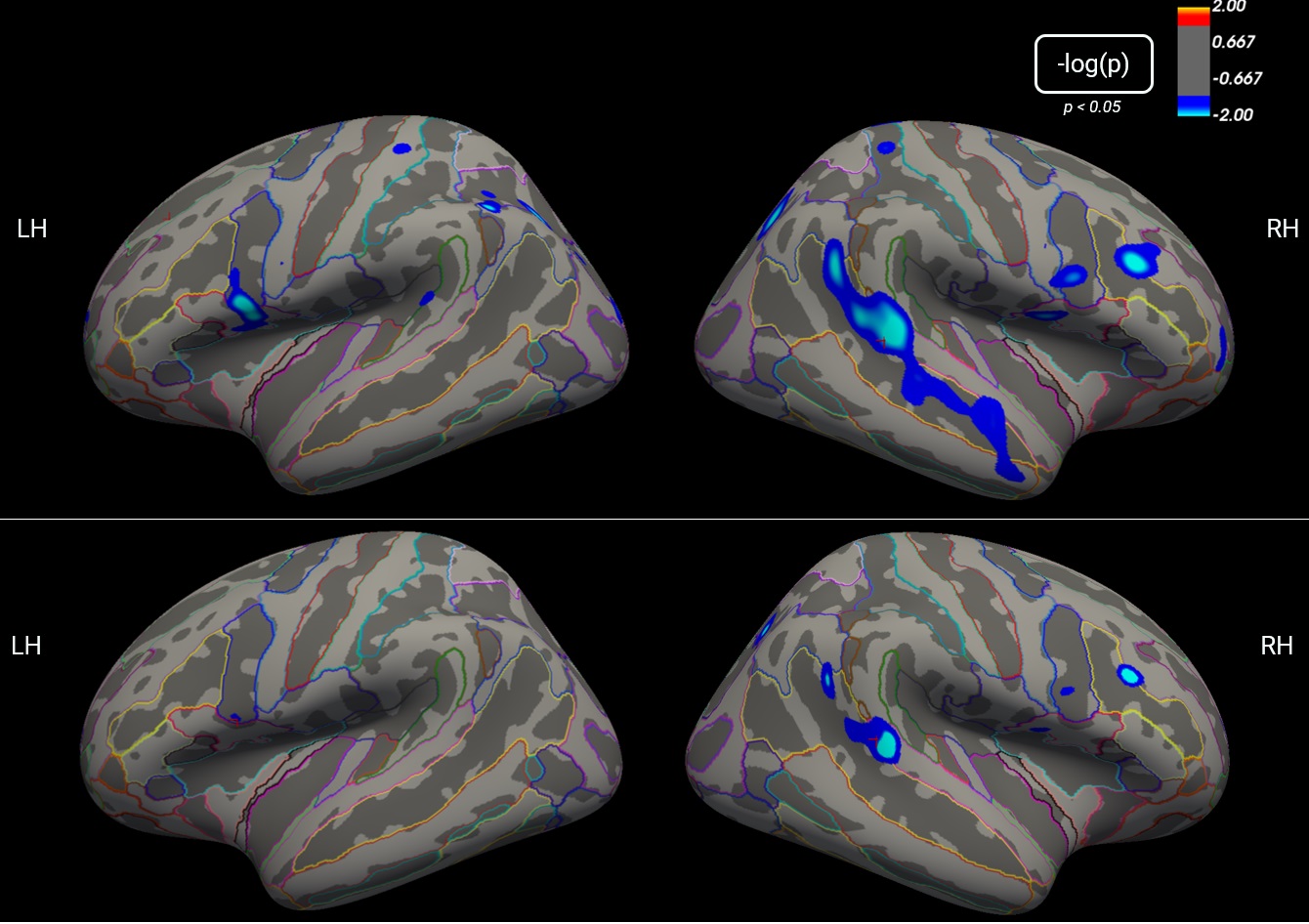 Figure 2. Cortical maps representing vertex-wise differences in surface area between patients with cSLE (n=30), and age/sex-matched controls (n=18). Blue colour indicates regions with statistically significant decreases in surface area in the cSLE group when compared to controls (p < 0.05). Coloured outlines annotate brain regions according to the Destrieux atlas. The top and bottom panels represent structural results before and after correcting for multiple comparisons, respectively.
Figure 2. Cortical maps representing vertex-wise differences in surface area between patients with cSLE (n=30), and age/sex-matched controls (n=18). Blue colour indicates regions with statistically significant decreases in surface area in the cSLE group when compared to controls (p < 0.05). Coloured outlines annotate brain regions according to the Destrieux atlas. The top and bottom panels represent structural results before and after correcting for multiple comparisons, respectively.Disclosures: S. Arciniegas, None; S. Mossad, None; T. El Tal, None; V. Lishak, None; S. Fevrier, None; I. Mohamed, None; J. Law, None; L. Ng, None; P. Moaf, None; H. Branson, None; A. Davis, None; L. Hiraki, None; D. Levy, None; a. Danguecan, None; G. Ibrahim, None; A. Knight, None.

