Back
Abstract Session
Session: Abstracts: Exemplary Interprofessional Research (0548–0553)
0551: Medical Cannabis Use by Rheumatology Patients According to Inflammatory versus Non-Inflammatory Condition
Saturday, November 12, 2022
5:15 PM – 5:25 PM Eastern Time
Location: Room 113
.png)
Mary-Ann Fitzcharles, MD, FRCPC
McGill University
Montreal-West, QC, Canada
Presenting Author(s)
kevin boehnke1, Tristin Smith1, Ying He1, marc martel2, david williams1 and Mary-Ann Fitzcharles3, 1University of Michigan, Ann Arbor, MI, 2McGill University, Montréal-Ouest, Canada, 3McGill University, Montréal, QC, Canada
Background/Purpose: Persistent pain and poor sleep are common symptoms experienced by patients with rheumatic diseases. Medical cannabis (MC) may offer symptomatic relief and is increasingly accessible to patients. Recent recreational cannabis legalization in many United State (US) states and Canada has opened this access gateway for patients who may be using MC with physician oversight or by self-administration. Improved understanding of the current MC culture will facilitate empathetic patient centered care. The objective of this survey was to characterize MC use amongst rheumatology patients in the US and Canada and to understand demographic and clinical differences between those with inflammatory versus non inflammatory rheumatic conditions.
Methods: Partnering with the Arthritis Foundation (US) and the Arthritis Society (Canada), we investigated MC use by persons self reporting a rheumatic condition via an online anonymous survey. We categorized 797 survey participants who currently use MC for symptom treatment as having an inflammatory (n=441) or non-inflammatory (n=356) rheumatic condition. Excluded were those under 18, residing outside the US or Canada, not fluent in English or French, without a rheumatic condition, who failed to provide consent or did not complete the survey. Symptom burden was assessed using the 2011 Fibromyalgia diagnostic criteria and the PROMIS Global Health (v1.2) instrument, with physical and mental health scores converted to respective t-scores for analysis. Symptom change was assessed using a 7-point Likert scale ranging from very much worse to very much better. R (version 4.1.1) was used for statistical analyses.
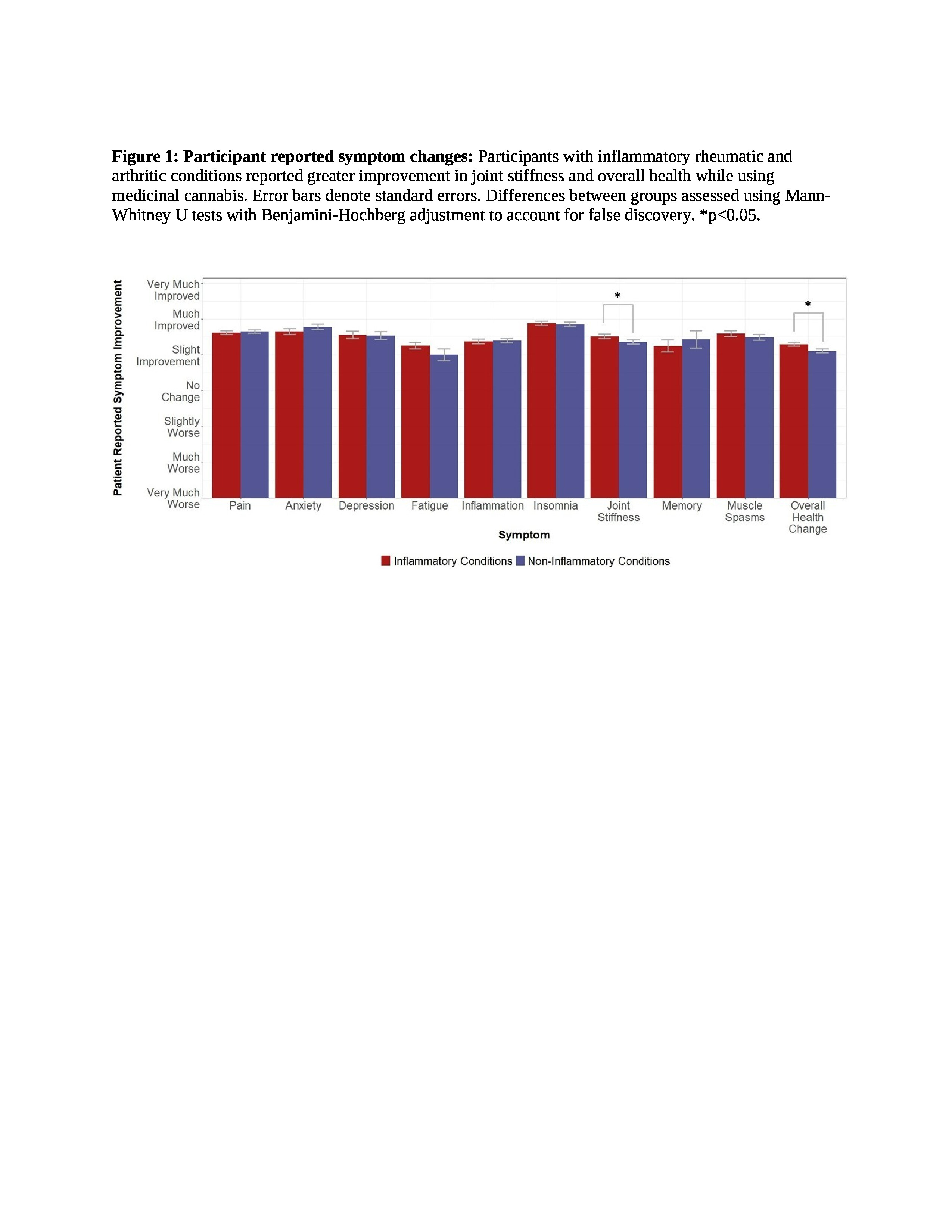
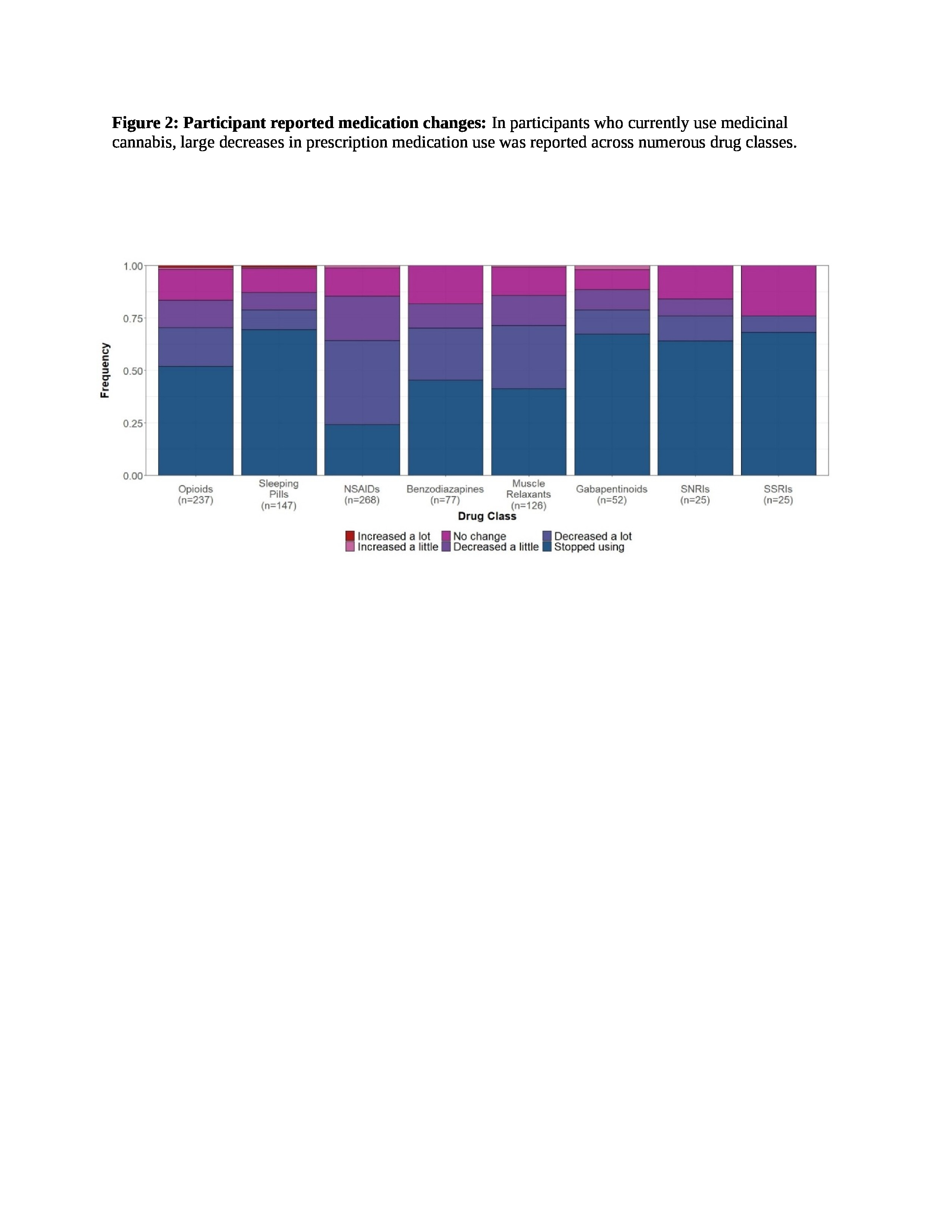
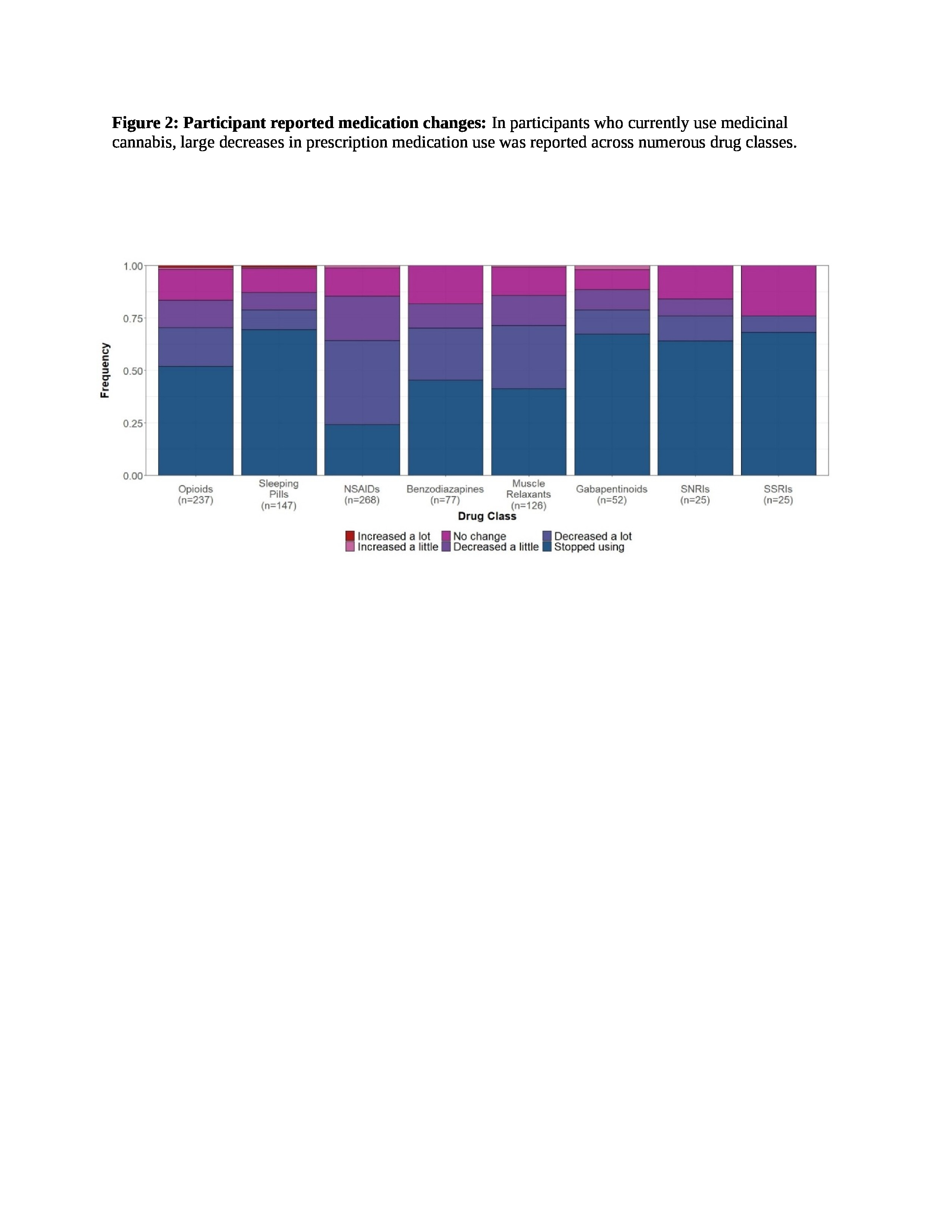
Results: Participants were predominantly white females, with some education beyond high school, and about 1/3 were employed (Table 1). Both groups reported high symptom burden with the inflammatory group reporting higher FM scores (p< 0.0001) and lower PROMIS physical (p< 0.0001) and mental health (p=0.0011) scores despite being younger on average (p< 0.0001) (Table 1). Both groups reported moderate symptom relief across all domains, with greater improvements in joint stiffness and global health for the inflammatory group compared to the non-inflammatory group (Figure 1, p< 0.05). Respondents also reported substantial medication substitution across prescription drug classes related to MC use (Figure 2). Notably, over half of participants who used opioids (51.9%), SNRIs (64.0%), SSRIs (68.0%), gabapentinoids (67.3%), and sleeping pills (69.4%) reported discontinuing these medications entirely as a result of MC substitute. No significant differences were observed between the two groups within any of these prescription medication classes.
Conclusion: High symptom burden is likely a driver for MC use by persons with both inflammatory and non-inflammatory rheumatic conditions. The substantial symptom relief and reported reduction or discontinuation of prescribed symptomatic treatments warrants formal study.
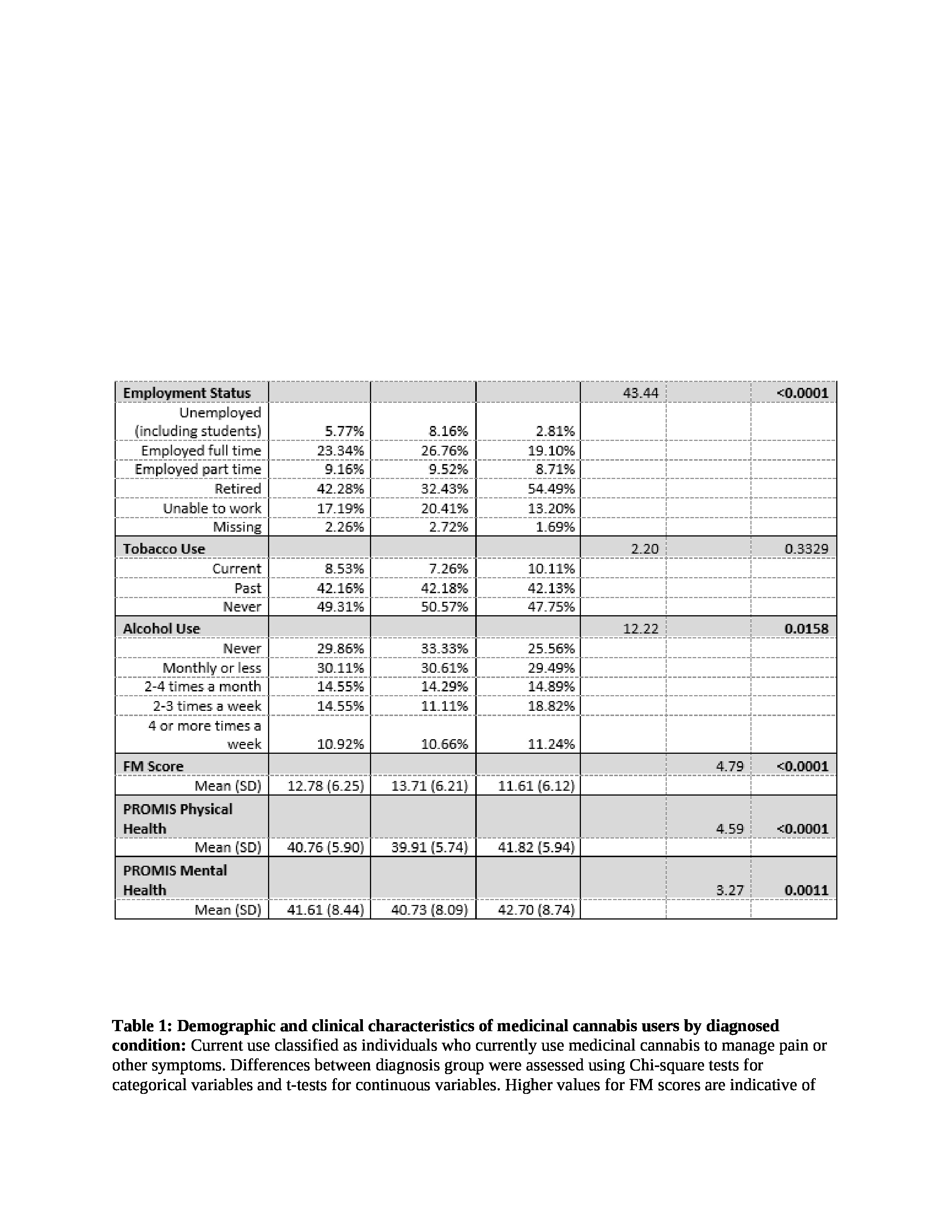 Table 1: Demographic and clinical characteristics of medicinal cannabis users by diagnosed condition: Current use classified as individuals who currently use medicinal cannabis to manage pain or other symptoms. Differences between diagnosis group were assessed using Chi-square tests for categorical variables and t-tests for continuous variables. Higher values for FM scores are indicative of more severe fibromyalgia symptoms, whereas higher PROMIS scores demonstrate greater physical and mental health.
Table 1: Demographic and clinical characteristics of medicinal cannabis users by diagnosed condition: Current use classified as individuals who currently use medicinal cannabis to manage pain or other symptoms. Differences between diagnosis group were assessed using Chi-square tests for categorical variables and t-tests for continuous variables. Higher values for FM scores are indicative of more severe fibromyalgia symptoms, whereas higher PROMIS scores demonstrate greater physical and mental health.
Disclosures: k. boehnke, Tryp therapeutics; T. Smith, None; Y. He, None; m. martel, Sant cannabis; d. williams, Swing therapeutics; M. Fitzcharles, None.
Background/Purpose: Persistent pain and poor sleep are common symptoms experienced by patients with rheumatic diseases. Medical cannabis (MC) may offer symptomatic relief and is increasingly accessible to patients. Recent recreational cannabis legalization in many United State (US) states and Canada has opened this access gateway for patients who may be using MC with physician oversight or by self-administration. Improved understanding of the current MC culture will facilitate empathetic patient centered care. The objective of this survey was to characterize MC use amongst rheumatology patients in the US and Canada and to understand demographic and clinical differences between those with inflammatory versus non inflammatory rheumatic conditions.
Methods: Partnering with the Arthritis Foundation (US) and the Arthritis Society (Canada), we investigated MC use by persons self reporting a rheumatic condition via an online anonymous survey. We categorized 797 survey participants who currently use MC for symptom treatment as having an inflammatory (n=441) or non-inflammatory (n=356) rheumatic condition. Excluded were those under 18, residing outside the US or Canada, not fluent in English or French, without a rheumatic condition, who failed to provide consent or did not complete the survey. Symptom burden was assessed using the 2011 Fibromyalgia diagnostic criteria and the PROMIS Global Health (v1.2) instrument, with physical and mental health scores converted to respective t-scores for analysis. Symptom change was assessed using a 7-point Likert scale ranging from very much worse to very much better. R (version 4.1.1) was used for statistical analyses.
Results: Participants were predominantly white females, with some education beyond high school, and about 1/3 were employed (Table 1). Both groups reported high symptom burden with the inflammatory group reporting higher FM scores (p< 0.0001) and lower PROMIS physical (p< 0.0001) and mental health (p=0.0011) scores despite being younger on average (p< 0.0001) (Table 1). Both groups reported moderate symptom relief across all domains, with greater improvements in joint stiffness and global health for the inflammatory group compared to the non-inflammatory group (Figure 1, p< 0.05). Respondents also reported substantial medication substitution across prescription drug classes related to MC use (Figure 2). Notably, over half of participants who used opioids (51.9%), SNRIs (64.0%), SSRIs (68.0%), gabapentinoids (67.3%), and sleeping pills (69.4%) reported discontinuing these medications entirely as a result of MC substitute. No significant differences were observed between the two groups within any of these prescription medication classes.
Conclusion: High symptom burden is likely a driver for MC use by persons with both inflammatory and non-inflammatory rheumatic conditions. The substantial symptom relief and reported reduction or discontinuation of prescribed symptomatic treatments warrants formal study.
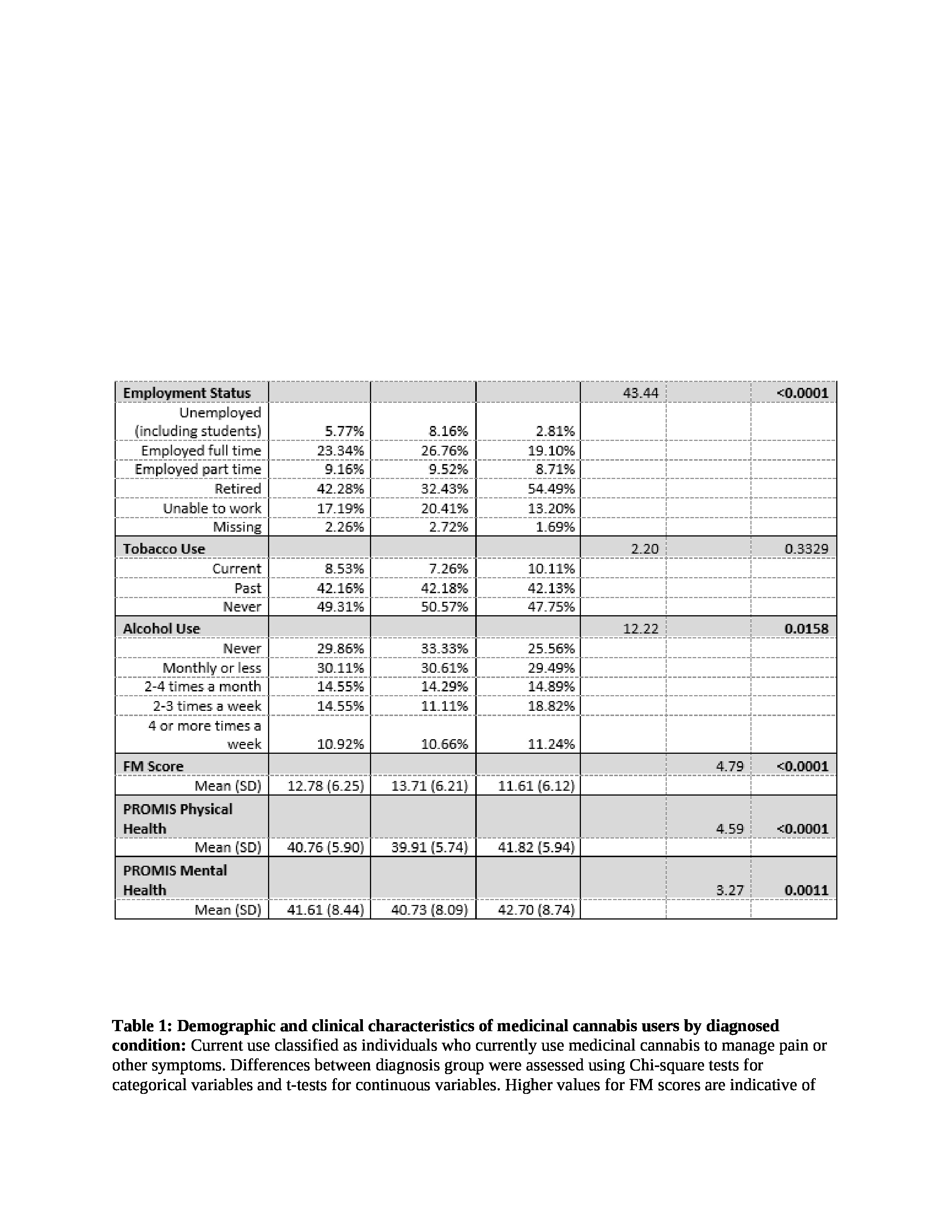 Table 1: Demographic and clinical characteristics of medicinal cannabis users by diagnosed condition: Current use classified as individuals who currently use medicinal cannabis to manage pain or other symptoms. Differences between diagnosis group were assessed using Chi-square tests for categorical variables and t-tests for continuous variables. Higher values for FM scores are indicative of more severe fibromyalgia symptoms, whereas higher PROMIS scores demonstrate greater physical and mental health.
Table 1: Demographic and clinical characteristics of medicinal cannabis users by diagnosed condition: Current use classified as individuals who currently use medicinal cannabis to manage pain or other symptoms. Differences between diagnosis group were assessed using Chi-square tests for categorical variables and t-tests for continuous variables. Higher values for FM scores are indicative of more severe fibromyalgia symptoms, whereas higher PROMIS scores demonstrate greater physical and mental health.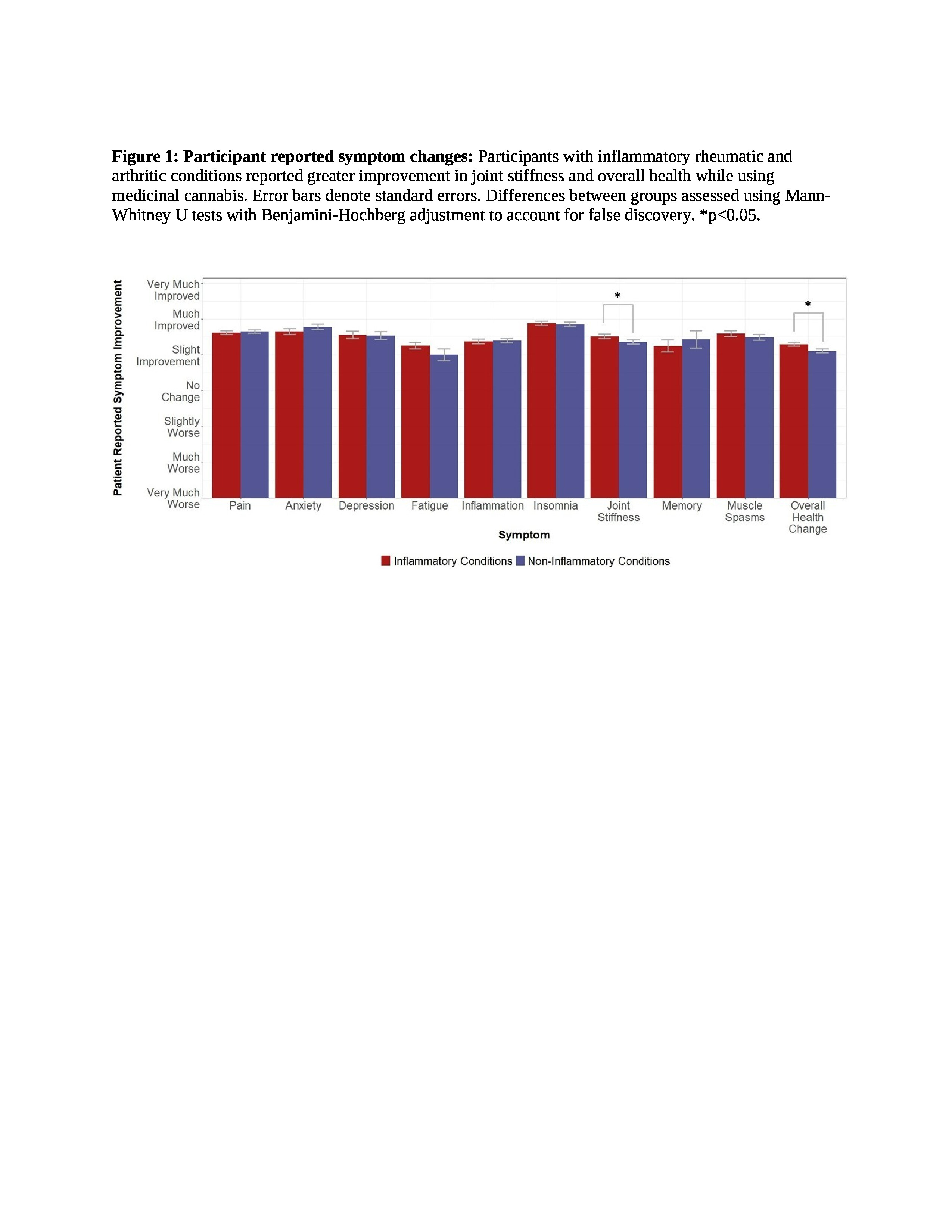
Disclosures: k. boehnke, Tryp therapeutics; T. Smith, None; Y. He, None; m. martel, Sant cannabis; d. williams, Swing therapeutics; M. Fitzcharles, None.

