Back
Poster Session D
Session: (1950–1979) RA – Diagnosis, Manifestations, and Outcomes Poster IV
1959: Increased Mortality in Patients with RA-Associated Interstitial Lung Disease: Data from a French Administrative Healthcare Database
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- PJ
Pierre-Antoine Juge, MD, PhD
Rheumatology department, Bichat Hospital
Paris, France
Abstract Poster Presenter(s)
Pierre-Antoine Juge1, Lidwine Wemeau2, Sebastien Ottaviani3, guillaume desjeux4, Joe Zhuo5, Virginie Vannier-Moreau6, René-Marc Flipo7, Bruno Crestani8 and Philippe Dieude9, 1Rheumatology department, Bichat Hospital, Paris, France, 2Pulmonology department, Lille University hospital, Lille, France, 3Hopital Bichat-Claude Bernard, Paris, France, 4e-Health Services Sanoia, Gemenos, France, 5BMS, Lawrenceville, NJ, 6BMS, Rueil-Malmaison, 7Hôpital Roger Salengro, Lille, France, 8Hopital Bichat, Paris University, Paris, France, 9Université Paris Cité, Paris, France
Background/Purpose: Interstitial lung disease (ILD) is a common extra-articular manifestation of RA. Studies have shown variability in the prevalence and mortality rate of patients with RA-associated ILD (RA-ILD). Further efforts are needed to better characterize the burden of ILD in patients with RA. Our objective was to compare the mortality rate in RA with and without ILD and to identify factors affecting mortality in patients with RA-ILD.
Methods: Data were analyzed from SNDS, the French national claims database, from between January 1, 2013, and December 31, 2018. Adults with an RA diagnosis (International Classification of Diseases, Tenth Revision [ICD-10] codes M05, M06.0, M06.8, and M06.9) and ≥ 2 distinct dates of DMARD delivery were included. ILD diagnosis was defined as having ICD-10 code J84 and ≥ 1 CT scan within 1 year of the first date of ILD occurrence. The mortality rates were compared between patients with RA-ILD and patients with RA without ILD (RA-noILD) and were matched 1:1 for age, sex, age at RA-ILD onset, and duration of RA using Cox proportional hazards regression.
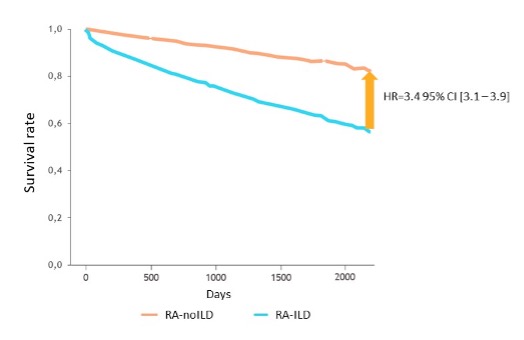
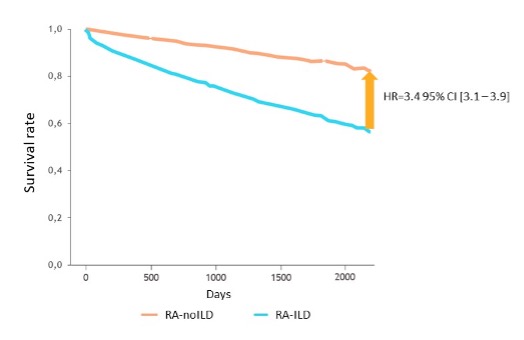
Results: Among the 173,132 patients with RA, ILD was identified in 4330 (2.5%). In patients with RA-ILD, mean age at RA onset was 63.3 ± 13.7 years and 39.8% were male. ILD onset occurred after RA onset in 71.6% of patients, concomitant with RA onset (± 1 year of RA onset) in 25.8%, and before RA onset in 2.5%. After matching, RA-ILD was associated with an increased mortality rate (hazard ratio [HR], 3.4; 95% confidence interval [CI], 3.1–3.9; Figure 1). Sensitivity analyses according to cardiovascular comorbidities and risk factors showed similar findings. The increased mortality rate was higher in patients aged < 75 years (HR, 4.8; 95% CI, 3.9–5.9) compared with patients aged > 75 years (HR, 3.0; 95% CI, 2.6–3.5); patients with ILD onset occurring before RA onset (HR, 8.4; 95% CI, 5.5–13.0) compared with patients with concomitant onset (HR, 5.3; 95% CI, 4.6–6.2) and with patients with ILD onset after RA onset (HR, 2.9; 95% CI, 2.6–3.3); and male patients (HR, 5.2; 95% CI, 4.4–6.2) compared with female patients (HR, 3.6; 95% CI, 3.0–4.2). The number of patients with ≥ 1 hospitalization was 1.45 times greater for patients with RA-ILD compared with RA-noILD.
Conclusion: In this nationwide cohort study, RA-ILD was associated with a strong increase in mortality rate in patients with RA, notably in younger patients, males, and patients whose ILD occurred before RA onset.
Disclosures: P. Juge, Bristol-Myers Squibb(BMS), Novartis, AstraZeneca, Boehringer-Ingelheim; L. Wemeau, Boehringer-Ingelheim, Bristol-Myers Squibb(BMS), Roche, Sanofi, Pfizer; S. Ottaviani, None; g. desjeux, None; J. Zhuo, Bristol-Myers Squibb(BMS); V. Vannier-Moreau, Bristol-Myers Squibb(BMS); R. Flipo, AbbVie/Abbott, Biogen, Bristol-Myers Squibb(BMS), Eli Lilly, Janssen, MSD, Mylan, Nordic Pharma France, Novartis, Pfizer, Roche-Chugaï, Sandoz, Sanofi, UCB; B. Crestani, Roche, Boehringer-Ingelheim; P. Dieude, None.
Background/Purpose: Interstitial lung disease (ILD) is a common extra-articular manifestation of RA. Studies have shown variability in the prevalence and mortality rate of patients with RA-associated ILD (RA-ILD). Further efforts are needed to better characterize the burden of ILD in patients with RA. Our objective was to compare the mortality rate in RA with and without ILD and to identify factors affecting mortality in patients with RA-ILD.
Methods: Data were analyzed from SNDS, the French national claims database, from between January 1, 2013, and December 31, 2018. Adults with an RA diagnosis (International Classification of Diseases, Tenth Revision [ICD-10] codes M05, M06.0, M06.8, and M06.9) and ≥ 2 distinct dates of DMARD delivery were included. ILD diagnosis was defined as having ICD-10 code J84 and ≥ 1 CT scan within 1 year of the first date of ILD occurrence. The mortality rates were compared between patients with RA-ILD and patients with RA without ILD (RA-noILD) and were matched 1:1 for age, sex, age at RA-ILD onset, and duration of RA using Cox proportional hazards regression.
Results: Among the 173,132 patients with RA, ILD was identified in 4330 (2.5%). In patients with RA-ILD, mean age at RA onset was 63.3 ± 13.7 years and 39.8% were male. ILD onset occurred after RA onset in 71.6% of patients, concomitant with RA onset (± 1 year of RA onset) in 25.8%, and before RA onset in 2.5%. After matching, RA-ILD was associated with an increased mortality rate (hazard ratio [HR], 3.4; 95% confidence interval [CI], 3.1–3.9; Figure 1). Sensitivity analyses according to cardiovascular comorbidities and risk factors showed similar findings. The increased mortality rate was higher in patients aged < 75 years (HR, 4.8; 95% CI, 3.9–5.9) compared with patients aged > 75 years (HR, 3.0; 95% CI, 2.6–3.5); patients with ILD onset occurring before RA onset (HR, 8.4; 95% CI, 5.5–13.0) compared with patients with concomitant onset (HR, 5.3; 95% CI, 4.6–6.2) and with patients with ILD onset after RA onset (HR, 2.9; 95% CI, 2.6–3.3); and male patients (HR, 5.2; 95% CI, 4.4–6.2) compared with female patients (HR, 3.6; 95% CI, 3.0–4.2). The number of patients with ≥ 1 hospitalization was 1.45 times greater for patients with RA-ILD compared with RA-noILD.
Conclusion: In this nationwide cohort study, RA-ILD was associated with a strong increase in mortality rate in patients with RA, notably in younger patients, males, and patients whose ILD occurred before RA onset.
Disclosures: P. Juge, Bristol-Myers Squibb(BMS), Novartis, AstraZeneca, Boehringer-Ingelheim; L. Wemeau, Boehringer-Ingelheim, Bristol-Myers Squibb(BMS), Roche, Sanofi, Pfizer; S. Ottaviani, None; g. desjeux, None; J. Zhuo, Bristol-Myers Squibb(BMS); V. Vannier-Moreau, Bristol-Myers Squibb(BMS); R. Flipo, AbbVie/Abbott, Biogen, Bristol-Myers Squibb(BMS), Eli Lilly, Janssen, MSD, Mylan, Nordic Pharma France, Novartis, Pfizer, Roche-Chugaï, Sandoz, Sanofi, UCB; B. Crestani, Roche, Boehringer-Ingelheim; P. Dieude, None.

