Back
Poster Session D
Session: (1924–1949) Pediatric Rheumatology – Clinical Poster III: Other
1942: Maybe Silent: Spine Disease in Chronic Recurrent Multifocal Osteomyelitis, Clinical Features, Risk Factors, and Red Flags
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SY
Shima Yasin, MD, MSc
University of Iowa Carver College of Medicine
Coralville, IA, United States
Abstract Poster Presenter(s)
Shima Yasin1, T. Shawn Sato2, Emma Leisinger2, Aleksander Lenert2, Yongdong (Dan) Zhao3 and Polly Ferguson1, 1University of Iowa Carver College of Medicine, Iowa City, IA, 2University of Iowa, Iowa City, IA, 3University of Washington, Redmond, WA
Background/Purpose: Chronic recurrent multifocal osteomyelitis (CRMO) is a female predominant autoinflammatory bone disease. The average age at disease onset is 9-10 years. The majority have favorable long-term outcomes. With wide utilization of whole-body MRI (WBMRI), increased reports of spine disease (SD) with variable degree of severity and vertebral plana were highlighted. SD is now considered a classic finding in CRMO, its incidence is reported at 10-35% in CRMO. To date, risk factors for SD in CRMO are unknown. SD can result in damaging outcomes such as vertebral fractures and deformities. Leveraging our large cohort, we aimed at characterizing clinical and radiological features of SD in CRMO, and identifying candidate clinical risk factors and red flags for SD in CRMO patients.
Methods: This study was approved by Institutional Review Board. Using retrospective chart review we identified cases of any degree SD in CRMO based on MRI findings (N:36), and matched those with 36 controls (CRMO patients without SD) using current age in case-control design. Clinical data was abstracted from medical records. We used Fischer exact and T.test for comparisons.
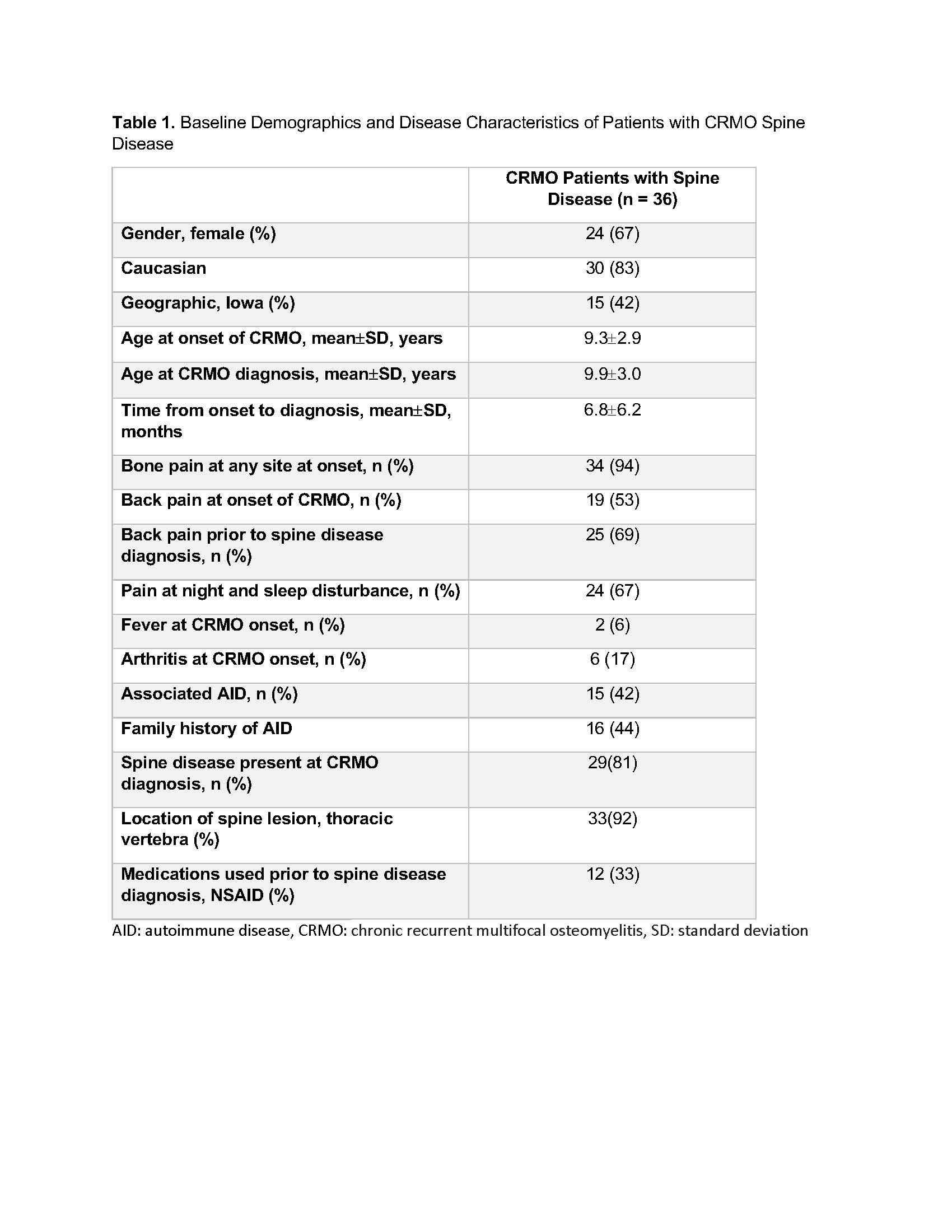
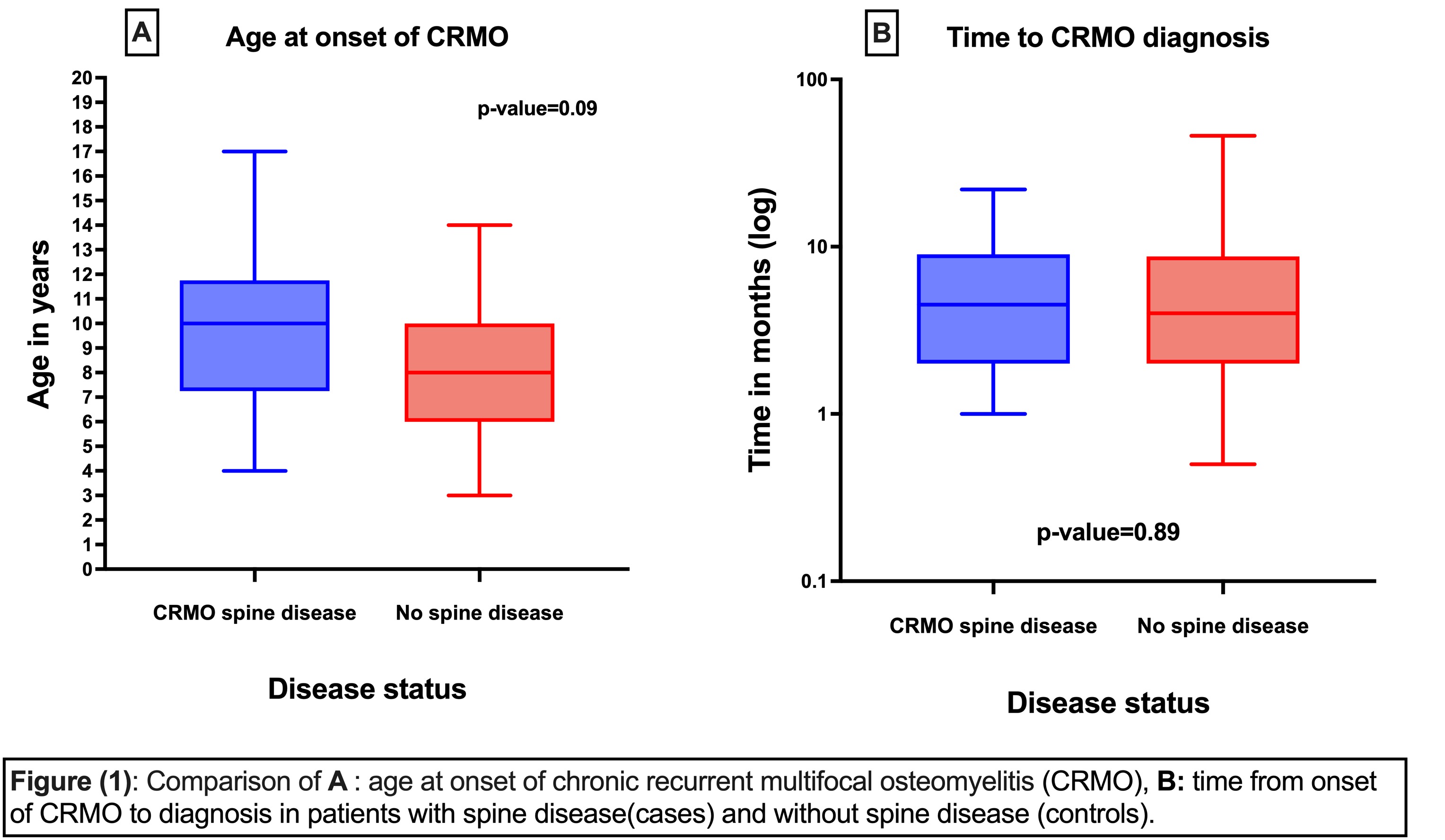
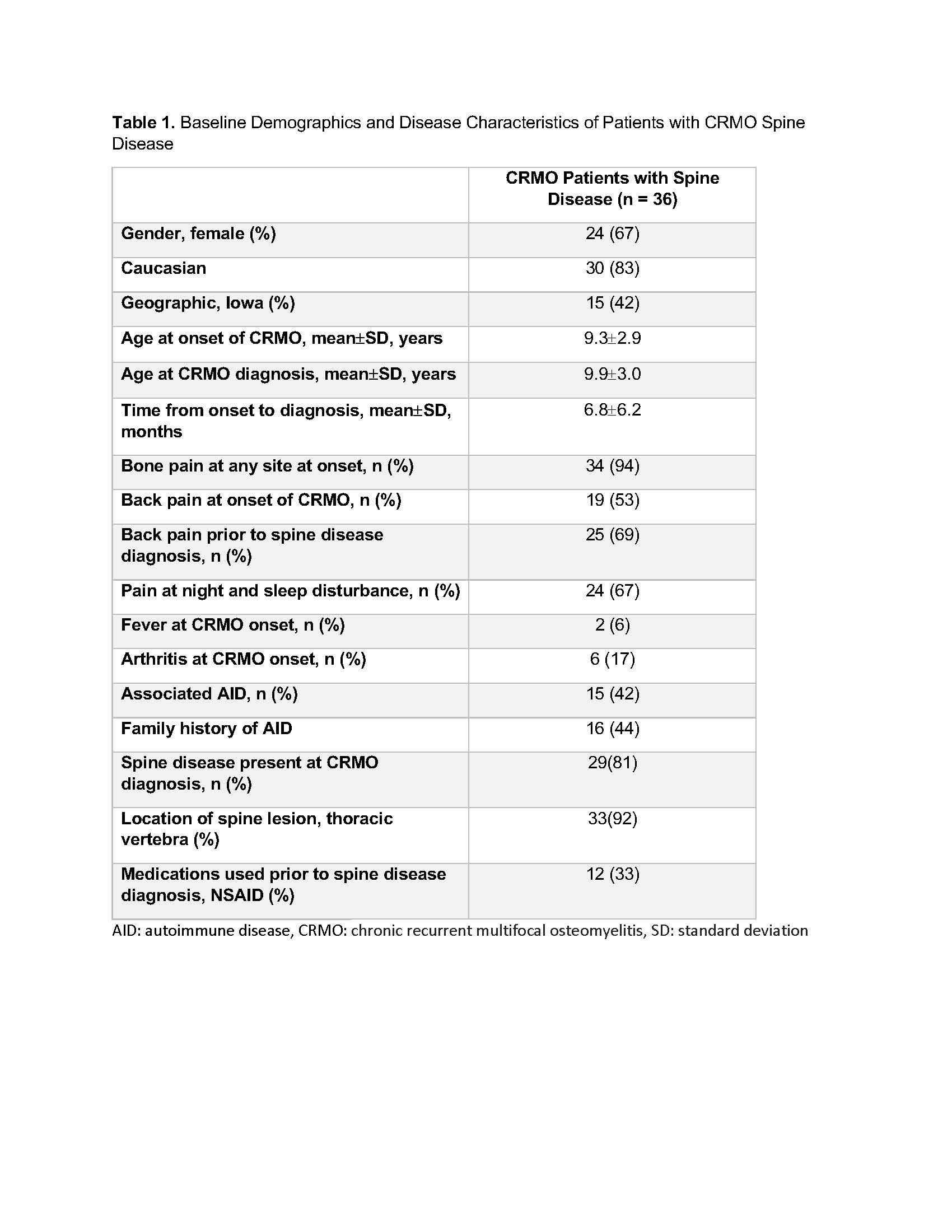
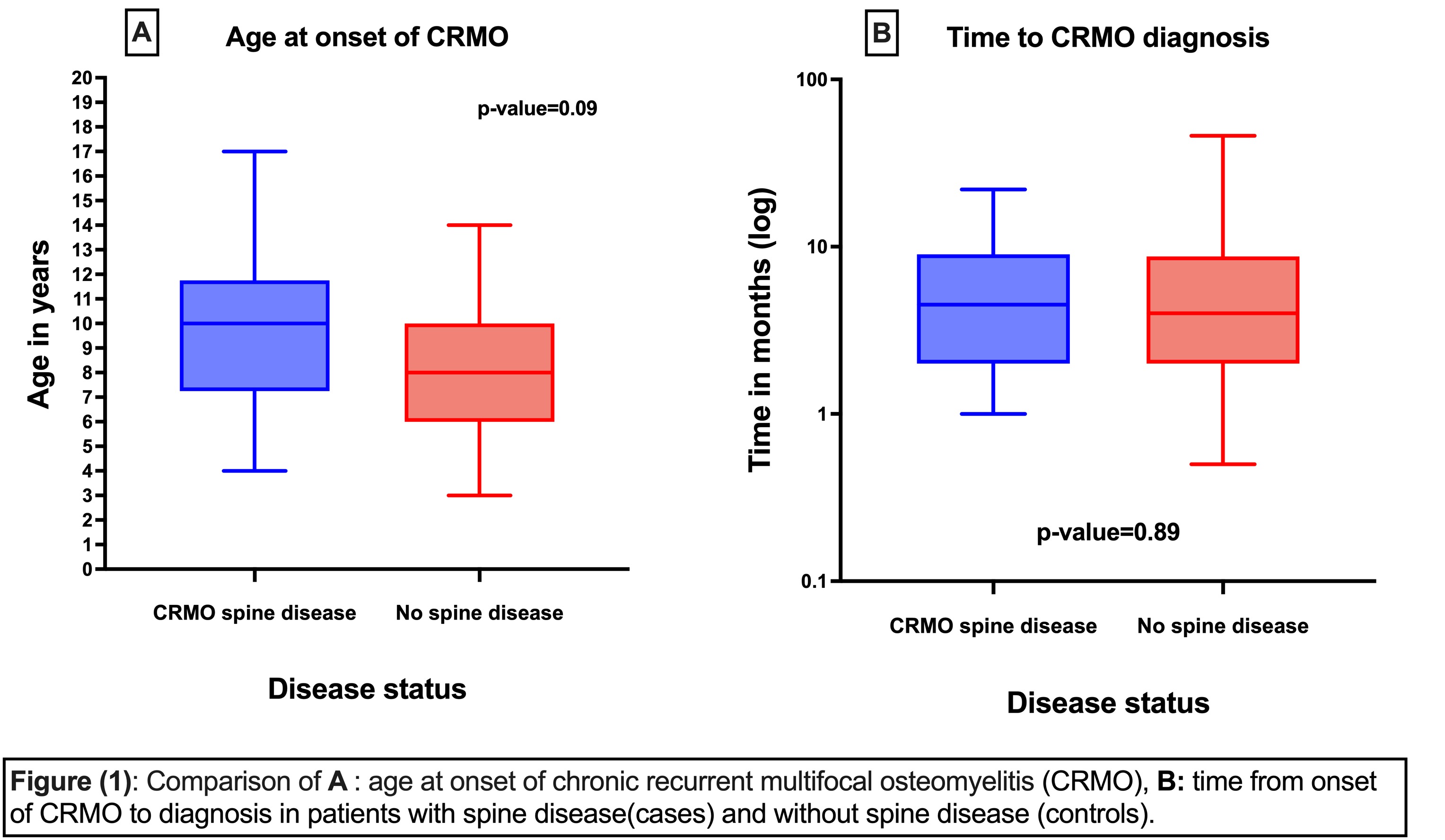
Results: In our cohort, patients with SD (summarized in table 1) were mostly Caucasian (83%), and two-thirds from out of state (second opinion). Despite female predominance (67%), the proportion of male with SD in the whole study (cases and control) was higher than female proportion (57% (12/21) vs 47% (24/51)). The majority (92%) had thoracic vertebra involvement, and 20% had vertebra plana. 42% had associated autoimmune disease (AID). Mean age at CRMO onset was 9.3 ± 2.9 years, and time to diagnosis was 6.8±6.2 months. Notably presenting at slightly older age, SD cases were not significantly different from controls in age at onset (p:0.09) or time to diagnosis (p 0.89) (Figure 1).
In SD, 47% of patients did not have back pain at CRMO onset and only 69% complained of back pain just prior to SD diagnosis. Most alarming, 31% (11/36) were asymptomatic with SD diagnosed incidentally on WBMRI. Pain at night and sleep disturbances were present in 67%, with significant difference compared to control (OR 3.5, p: 0.018) (Figure 2-A). Similarly, presence of back pain was a significant risk factor for SD (OR 39, p < 0.0001) (Figure 2-B). When compared to controls, SD patients did not have significant difference in presence of fever (p 0.15), arthritis (p 0.39), AID (p 0.21), or family history of AID (p 0.3). 33% were on NSAIDs when SD developed, of those 89% reported pain and poor CRMO control despite NSAIDs.
Conclusion: SD in CRMO is not as rare as previously suggested. Patients with SD present at slightly older age, and males might be affected at higher proportion. Nearly half of patients with SD did not report back pain at onset of CRMO symptoms and one-third had no back pain despite active lesions on WBMRI at the time of SD diagnosis. Utilization of universal WBMRI for every child with suspected or diagnosed CRMO initially and at subsequent follow up is crucial. Early and prompt targeted therapy for SD is critical in preventing long term sequalae such as vertebra plana and deformities. Complains of back pain, pain at night, and sleep disturbances are risk factors and red flags for SD and should prompt immediate screening.
.jpg)
Disclosures: S. Yasin, None; T. Sato, None; E. Leisinger, None; A. Lenert, None; Y. Zhao, None; P. Ferguson, None.
Background/Purpose: Chronic recurrent multifocal osteomyelitis (CRMO) is a female predominant autoinflammatory bone disease. The average age at disease onset is 9-10 years. The majority have favorable long-term outcomes. With wide utilization of whole-body MRI (WBMRI), increased reports of spine disease (SD) with variable degree of severity and vertebral plana were highlighted. SD is now considered a classic finding in CRMO, its incidence is reported at 10-35% in CRMO. To date, risk factors for SD in CRMO are unknown. SD can result in damaging outcomes such as vertebral fractures and deformities. Leveraging our large cohort, we aimed at characterizing clinical and radiological features of SD in CRMO, and identifying candidate clinical risk factors and red flags for SD in CRMO patients.
Methods: This study was approved by Institutional Review Board. Using retrospective chart review we identified cases of any degree SD in CRMO based on MRI findings (N:36), and matched those with 36 controls (CRMO patients without SD) using current age in case-control design. Clinical data was abstracted from medical records. We used Fischer exact and T.test for comparisons.
Results: In our cohort, patients with SD (summarized in table 1) were mostly Caucasian (83%), and two-thirds from out of state (second opinion). Despite female predominance (67%), the proportion of male with SD in the whole study (cases and control) was higher than female proportion (57% (12/21) vs 47% (24/51)). The majority (92%) had thoracic vertebra involvement, and 20% had vertebra plana. 42% had associated autoimmune disease (AID). Mean age at CRMO onset was 9.3 ± 2.9 years, and time to diagnosis was 6.8±6.2 months. Notably presenting at slightly older age, SD cases were not significantly different from controls in age at onset (p:0.09) or time to diagnosis (p 0.89) (Figure 1).
In SD, 47% of patients did not have back pain at CRMO onset and only 69% complained of back pain just prior to SD diagnosis. Most alarming, 31% (11/36) were asymptomatic with SD diagnosed incidentally on WBMRI. Pain at night and sleep disturbances were present in 67%, with significant difference compared to control (OR 3.5, p: 0.018) (Figure 2-A). Similarly, presence of back pain was a significant risk factor for SD (OR 39, p < 0.0001) (Figure 2-B). When compared to controls, SD patients did not have significant difference in presence of fever (p 0.15), arthritis (p 0.39), AID (p 0.21), or family history of AID (p 0.3). 33% were on NSAIDs when SD developed, of those 89% reported pain and poor CRMO control despite NSAIDs.
Conclusion: SD in CRMO is not as rare as previously suggested. Patients with SD present at slightly older age, and males might be affected at higher proportion. Nearly half of patients with SD did not report back pain at onset of CRMO symptoms and one-third had no back pain despite active lesions on WBMRI at the time of SD diagnosis. Utilization of universal WBMRI for every child with suspected or diagnosed CRMO initially and at subsequent follow up is crucial. Early and prompt targeted therapy for SD is critical in preventing long term sequalae such as vertebra plana and deformities. Complains of back pain, pain at night, and sleep disturbances are risk factors and red flags for SD and should prompt immediate screening.
.jpg)
Disclosures: S. Yasin, None; T. Sato, None; E. Leisinger, None; A. Lenert, None; Y. Zhao, None; P. Ferguson, None.

