Back
Poster Session D
Session: (1950–1979) RA – Diagnosis, Manifestations, and Outcomes Poster IV
1953: Mortality in Rheumatoid Arthritis: Changing Causes and Predictive Factors. Study of a Cohort Followed Prospectively
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- CC
Cristina Corrales, MD
HOSPITAL UNIVERSITARIO MARQUES DE VALDECILLA
Santander, Spain
Abstract Poster Presenter(s)
Cristina Corrales1, Fabricio Benavides Villanueva1, Ivan Ferraz Amaro2, Nuria Vegas Revenga3, Virgi Portilla4, Ricardo Blanco5, Miguel Ángel González-Gay6 and Alfonso Corrales4, 1Hospital Universitario Marqués de Valdecilla, Santander, Spain, 2Division of Rheumatology. Hospital Universitario de Canarias. Spain., Santa Cruz de Tenerife, Spain, 3Hospital Galdakao- Usansolo, Galdakao, Spain, 4Research Group on Genetic Epidemiology and Atherosclerosis in Systemic Diseases and in Metabolic Bone Diseases of the Musculoskeletal System, IDIVAL; and Department of Rheumatology, Hospital Universitario Marqués de Valdecilla, Santander, Spain, 5Hospital Universitario Marqués de Valdecilla, IDIVAL, Santander, Spain, 6Department of Medicine and Psychiatry, Universidad de Cantabria; Rheumatology Division, Hospital Universitario Marqués de Valdecilla; Research group on genetic epidemiology and atherosclerosis in systemic diseases and in metabolic diseases of the musculoskeletal system, IDIVAL, Santander, Spain. Cardiovascular Pathophysiology and Genomics Research Unit, School of Physiology, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
Background/Purpose: Patients with Rheumatoid Arthritis (RA) present an increased risk of mortality. In the last decades, mortality rates tended to decrease but cardiovascular (CV) events remained as the leading cause of death in most series. The main objective is to assess mortality rates and leading causes of death, as well as predictors of mortality related to disease activity in a prospectively followed-up cohort of RA patients.
Methods: We conducted a prospective longitudinal study that included 673 RA patients from a single tertiary center. Univariate and multivariate Cox proportional hazards regression were used to identify predictors of mortality.
Results: We studied 673 patients with RA (75% women), mean age 61±13 years. The main general characteristics, CV risk factors, RA disease activity data and current treatment are summarized in the Table.
After a follow-up of 4,367 person-years (mean 6.4±1.4), 67 deaths were recorded. Considering all causes of mortality, the cumulative incidence was 14% (95% CI 11-18) with a mortality incidence rate of 0.015 (95% CI 0.012-0.020) patient/year. The main causes of mortality in decreasing order of frequency were infections (N=23) (34%), incidence rate-IR: 0.005 [95% CI 0.003-0.008]), cancer (N=18) (27%), IR: 0.004 [95% CI 0.002-0.007]), CV events (N= 12) (18%), IR: 0.003 [95% CI 0.001-0.005]), respiratory diseases (N=2) (3%), IR: 0.0005 [95% CI 0.00007-0.002] and other causes (N=12) (18%), IR: 0.003 [95% CI 0.001-0.005I].
The statistically significant predictive factors of mortality in the univariate analysis were male gender (HR 1.97[95%CI 1.20-3.21, p=0.007), abdominal circumference (HR 1.03 [95% CI 1.01-1.05], p=0,0006), diabetes (HR 2.85 [95%CI 1.68-4.86], p< 0.001) and hypertension (HR 2.92 [95%CI 1.73-4.94], p< 0.001). Also, baseline data of variables associated with disease activity such as increased CRP, ESR, DAS28-CRP, DAS28-ESR were predictors of mortality (Figure). Disease related parameters were adjusted by CV risk factors in a multivariate analysis. Following this procedure, the predictive factors that reached statistical significance; (Hazard Ratio [95%CI]), were an increased in DAS28-VSG (1.40 [1.07-1.83], p=0.016), DAS- 28-PCR (1.40 [1.07-1.83], p=0.016), CRP (1.02 [1.01-1.05] p=0.002), and ESR (1.03 [1.01- 1.05], p=< 0.001) (Figure).
Conclusion: In a cohort of patients with RA followed prospectively in a tertiary hospital, infections and malignancies are the main cause of mortality rather than CV events. Disease activity parameters are associated with an increased risk of mortality in these patients with RA.
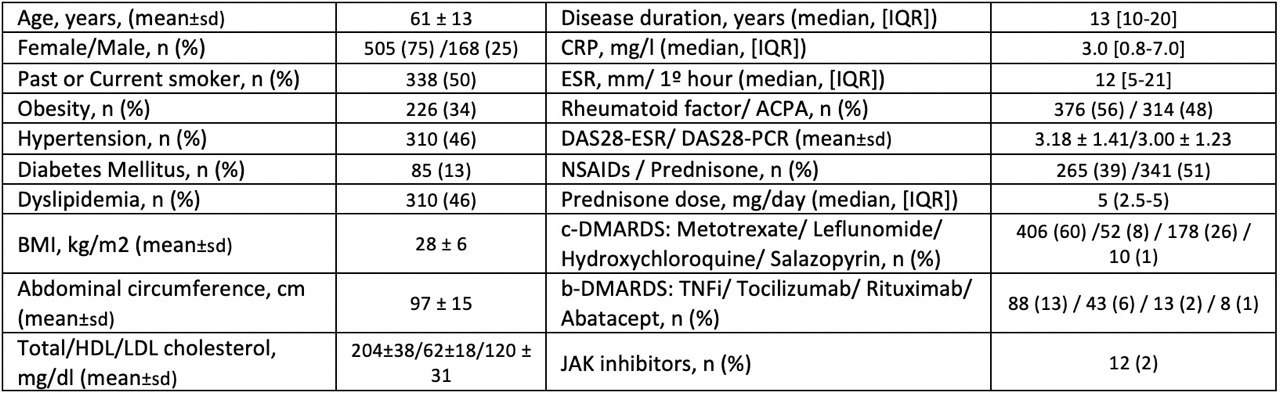 Table. Baseline characteristics of 673 RA patients.
Table. Baseline characteristics of 673 RA patients.
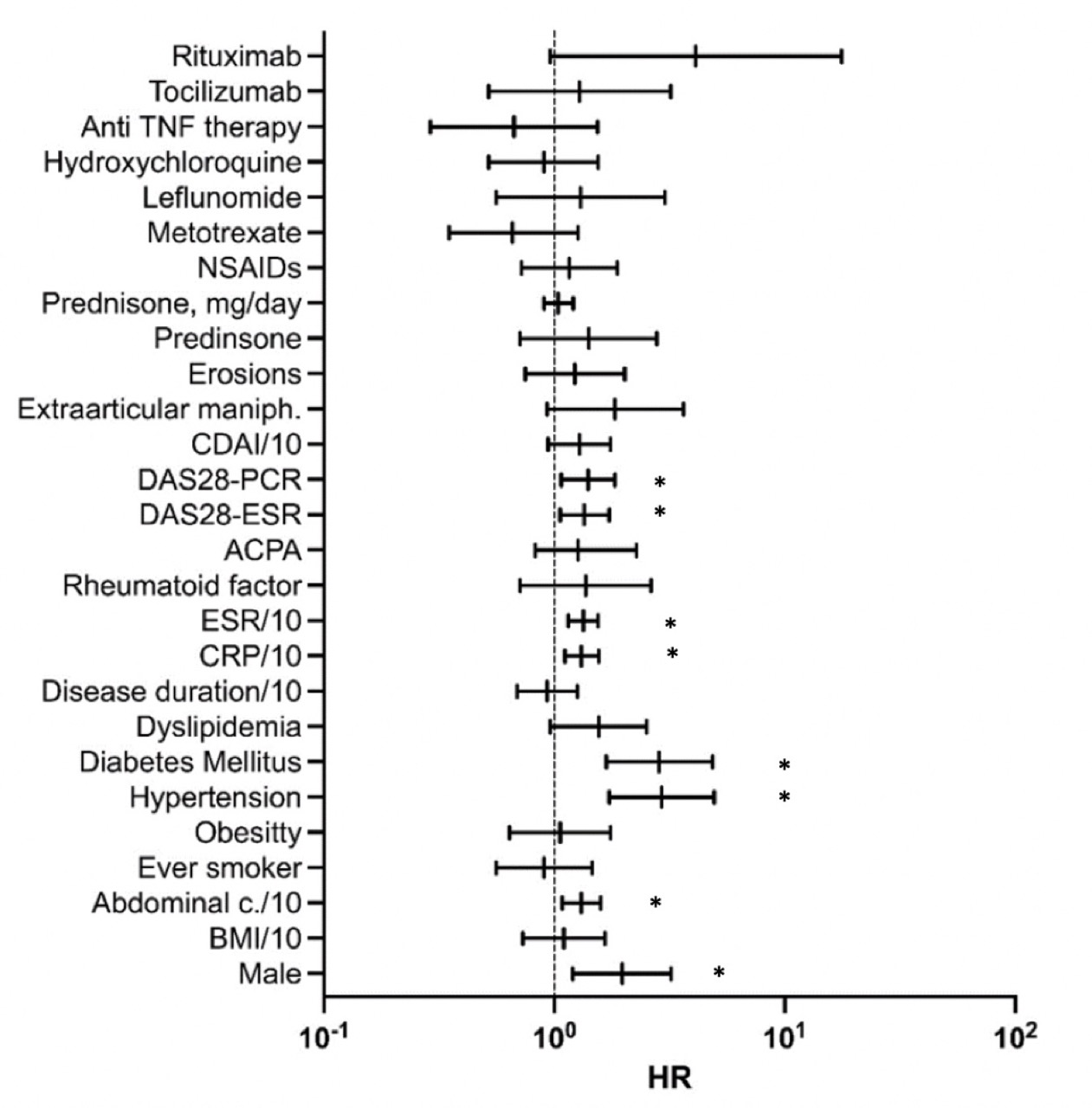 Figure. Forest Plot of mortality (Univariate and multivariate analysis).
Figure. Forest Plot of mortality (Univariate and multivariate analysis).
Results expressed in logarithmic scale. Multivariate analysis: Disease activity related parameters adjusted by age, gender, disease duration, smoker, diabetes, hypertension and abdominal circumference. CDAI, ESR and CPR expressed value/10. (*) p < 0.05.
Disclosures: C. Corrales, None; F. Benavides Villanueva, None; I. Ferraz Amaro, AbbVie/Abbott, Merck/MSD, Janssen, Roche, AbbVie/Abbott, Pfizer, Roche, Amgen, Celgene, Merck/MSD; N. Vegas Revenga, None; V. Portilla, None; R. Blanco, Eli Lilly, Pfizer, Roche, Janssen, MSD, AbbVie, Amgen, AstraZeneca, Bristol Myers Squibb, Galapagos, Novartis, Sanofi; M. González-Gay, AbbVie/Abbott, Merck/MSD, Janssen, Roche, AbbVie/Abbott, Roche, Sanofi, Eli Lilly, Celgene, Sobi, Merck/MSD; A. Corrales, None.
Background/Purpose: Patients with Rheumatoid Arthritis (RA) present an increased risk of mortality. In the last decades, mortality rates tended to decrease but cardiovascular (CV) events remained as the leading cause of death in most series. The main objective is to assess mortality rates and leading causes of death, as well as predictors of mortality related to disease activity in a prospectively followed-up cohort of RA patients.
Methods: We conducted a prospective longitudinal study that included 673 RA patients from a single tertiary center. Univariate and multivariate Cox proportional hazards regression were used to identify predictors of mortality.
Results: We studied 673 patients with RA (75% women), mean age 61±13 years. The main general characteristics, CV risk factors, RA disease activity data and current treatment are summarized in the Table.
After a follow-up of 4,367 person-years (mean 6.4±1.4), 67 deaths were recorded. Considering all causes of mortality, the cumulative incidence was 14% (95% CI 11-18) with a mortality incidence rate of 0.015 (95% CI 0.012-0.020) patient/year. The main causes of mortality in decreasing order of frequency were infections (N=23) (34%), incidence rate-IR: 0.005 [95% CI 0.003-0.008]), cancer (N=18) (27%), IR: 0.004 [95% CI 0.002-0.007]), CV events (N= 12) (18%), IR: 0.003 [95% CI 0.001-0.005]), respiratory diseases (N=2) (3%), IR: 0.0005 [95% CI 0.00007-0.002] and other causes (N=12) (18%), IR: 0.003 [95% CI 0.001-0.005I].
The statistically significant predictive factors of mortality in the univariate analysis were male gender (HR 1.97[95%CI 1.20-3.21, p=0.007), abdominal circumference (HR 1.03 [95% CI 1.01-1.05], p=0,0006), diabetes (HR 2.85 [95%CI 1.68-4.86], p< 0.001) and hypertension (HR 2.92 [95%CI 1.73-4.94], p< 0.001). Also, baseline data of variables associated with disease activity such as increased CRP, ESR, DAS28-CRP, DAS28-ESR were predictors of mortality (Figure). Disease related parameters were adjusted by CV risk factors in a multivariate analysis. Following this procedure, the predictive factors that reached statistical significance; (Hazard Ratio [95%CI]), were an increased in DAS28-VSG (1.40 [1.07-1.83], p=0.016), DAS- 28-PCR (1.40 [1.07-1.83], p=0.016), CRP (1.02 [1.01-1.05] p=0.002), and ESR (1.03 [1.01- 1.05], p=< 0.001) (Figure).
Conclusion: In a cohort of patients with RA followed prospectively in a tertiary hospital, infections and malignancies are the main cause of mortality rather than CV events. Disease activity parameters are associated with an increased risk of mortality in these patients with RA.
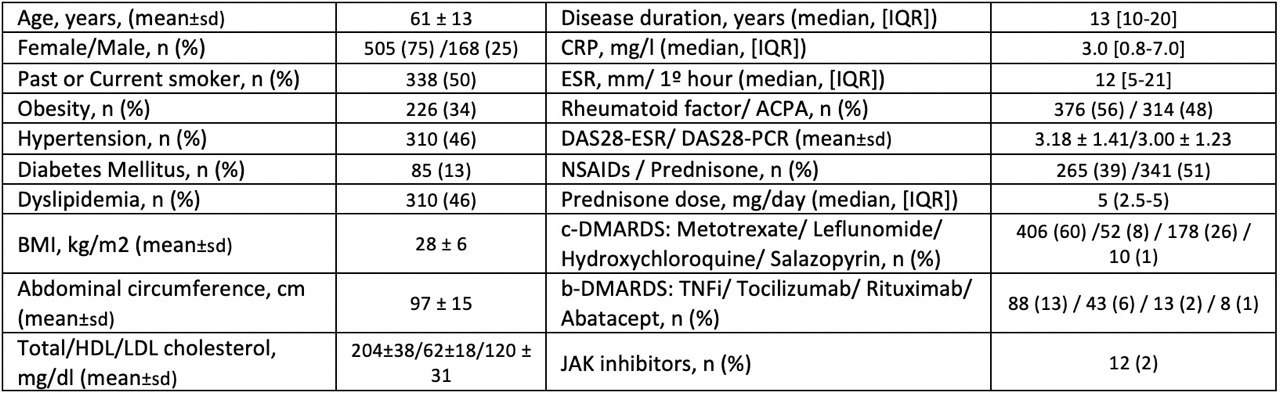 Table. Baseline characteristics of 673 RA patients.
Table. Baseline characteristics of 673 RA patients.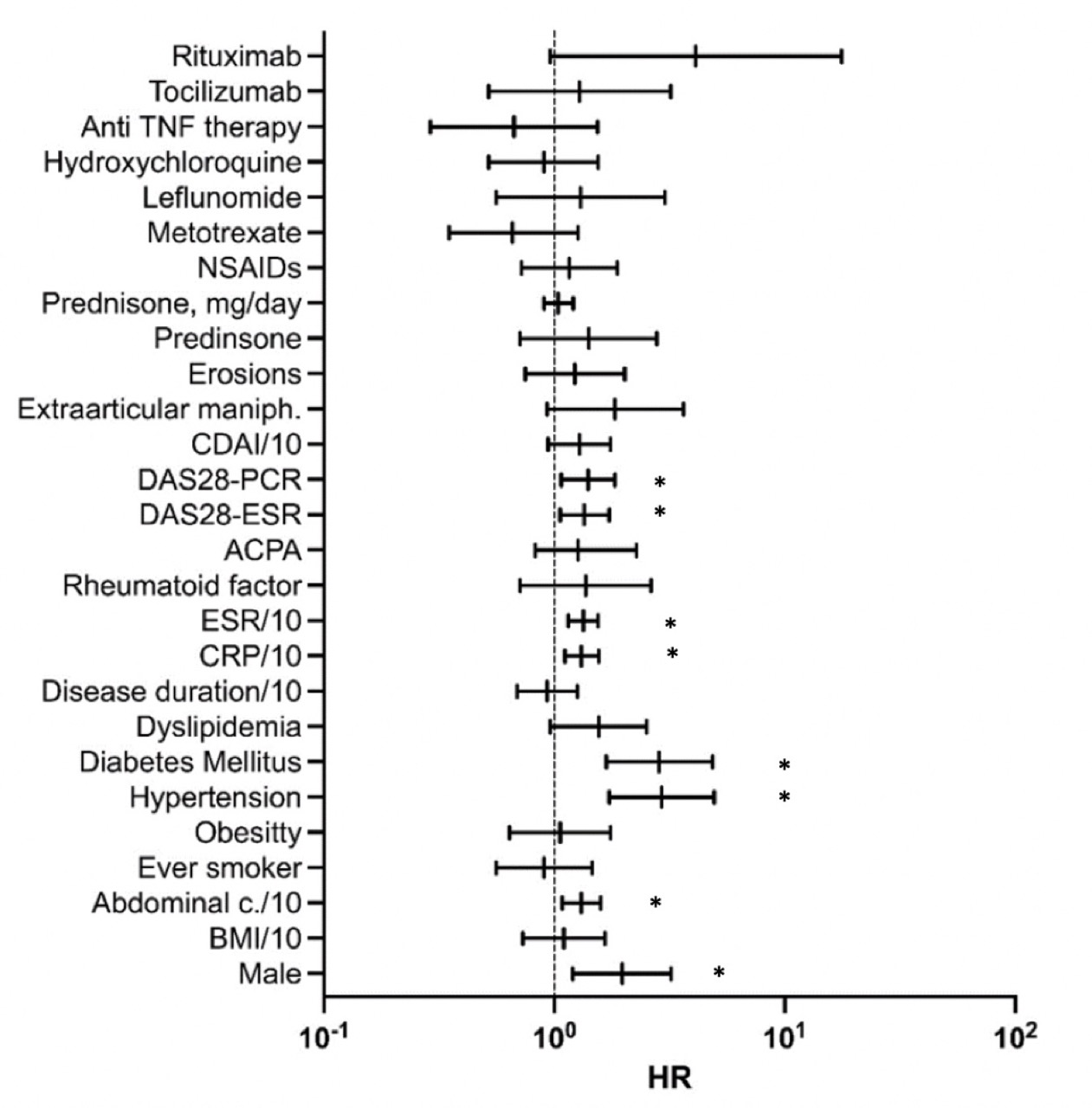 Figure. Forest Plot of mortality (Univariate and multivariate analysis).
Figure. Forest Plot of mortality (Univariate and multivariate analysis).Results expressed in logarithmic scale. Multivariate analysis: Disease activity related parameters adjusted by age, gender, disease duration, smoker, diabetes, hypertension and abdominal circumference. CDAI, ESR and CPR expressed value/10. (*) p < 0.05.
Disclosures: C. Corrales, None; F. Benavides Villanueva, None; I. Ferraz Amaro, AbbVie/Abbott, Merck/MSD, Janssen, Roche, AbbVie/Abbott, Pfizer, Roche, Amgen, Celgene, Merck/MSD; N. Vegas Revenga, None; V. Portilla, None; R. Blanco, Eli Lilly, Pfizer, Roche, Janssen, MSD, AbbVie, Amgen, AstraZeneca, Bristol Myers Squibb, Galapagos, Novartis, Sanofi; M. González-Gay, AbbVie/Abbott, Merck/MSD, Janssen, Roche, AbbVie/Abbott, Roche, Sanofi, Eli Lilly, Celgene, Sobi, Merck/MSD; A. Corrales, None.

