Back
Poster Session D
Session: (2052–2107) SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
2057: Outpatient Visit Adherence and Impact on Disease-related Morbidity in Childhood-onset Systemic Lupus Erythematosus (cSLE)
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- MN
Meghan Nelson, DO
Emory
Atlanta, GA, United States
Abstract Poster Presenter(s)
Meghan Nelson1, Colleen Mosley2, D. Sofia Villacis-Nunez3, Kelly Rouster-Stevens3 and Amit Thakral3, 1Division of Pediatric Rheumatology, Department of Pediatrics, Emory University School of Medicine; Children's Healthcare of Atlanta, Atlanta, GA, 2Children’s Healthcare of Atlanta, Atlanta, GA, 3Division of Pediatric Rheumatology, Department of Pediatrics, Emory University School of Medicine; Children’s Healthcare of Atlanta, Atlanta, GA
Background/Purpose: Systemic lupus erythematosus (SLE) is a multisystem autoimmune disease that is associated with significant disease damage, morbidity, and mortality. In comparison to the adult population, childhood onset SLE (cSLE) tends to be more aggressive given the higher preponderance of renal and neuropsychiatric disease and increased disease activity. There is a paucity of literature examining relationship between disease activity, follow up, and health care utilization. The objective of this study is to determine whether early identification of those at risk for loss to follow up would affect compliance with follow-up visits and disease morbidity in patients with childhood-onset systemic lupus erythematosus (cSLE).
Methods: Between July 2021 and January 2022 charts of patients < 18 years of age with SLE who met Systemic Lupus International Collaborative Clinics (SLICC) classification criteria were surveilled and those who were not evaluated in clinic in the previous 120-day period were eligible for inclusion. Identified patients were added to a follow up list and subsequently contacted via telephone for re-establishing care within the month, if eligible.Through retrospective chart review, we assessed disease activity (SLE Disease Activity Index) at last clinic visit. Patients were stratified into two cohorts of lower and higher disease activity, with SLE disease activity index (SLEDAI) < 4 and SLEDAI ≥ 4, respectively. Clinical, epidemiological and serological data, as well as markers of disease morbidity including hospitalizations and Emergency Department (ED) visits were reviewed and compared between the two groups using Fisher exact test for categorical variables and Wilcoxon test for continuous variables.
Results: Forty-one patients were included, of which 34 (83%) were female. Median age was 14 years. Statistically significant differences were identified between the groups, to include age at diagnosis (p< 0.001) associated with higher current SLEDAI score. Of the patients reviewed, participants met an average of 4.6/13 SLICC criteria at diagnosis, with several of these criteria noted to be statistically significant between groups (Table 1). Time to follow up (p< 0.001), high dose prednisone use (p=0.04), hospitalizations (p< 0.001) and ED visits (p< 0.001) were found to be associated with higher SLEDAI scores.
Conclusion: Our findings suggest that cSLE patients with current higher disease activity are at risk for disease related morbidity in the setting of follow-up non-adherence. While further studies are required to enhance our understanding of this association, this links the importance of disease-related outcome and outpatient follow-up visits in this particularly vulnerable patient population.
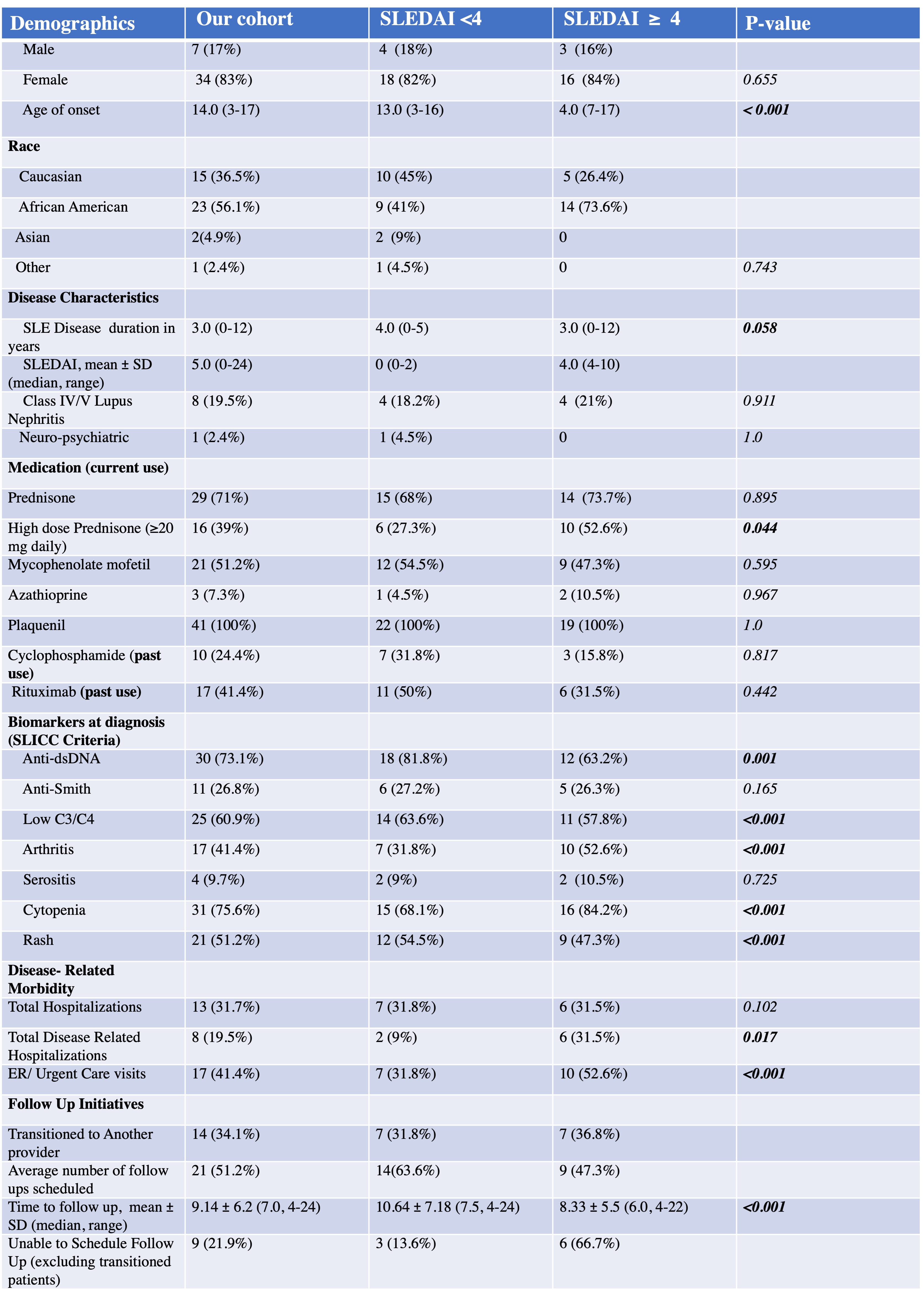 Table 1: Characteristics of cSLE stratified by SLEDAI. This table depicts the patient demographics, clinical features and management of pediatric systemic lupus erythematosus patients for patients stratified be SLEDAI score.
Table 1: Characteristics of cSLE stratified by SLEDAI. This table depicts the patient demographics, clinical features and management of pediatric systemic lupus erythematosus patients for patients stratified be SLEDAI score.
Disclosures: M. Nelson, None; C. Mosley, None; D. Villacis-Nunez, None; K. Rouster-Stevens, Accordant; A. Thakral, None.
Background/Purpose: Systemic lupus erythematosus (SLE) is a multisystem autoimmune disease that is associated with significant disease damage, morbidity, and mortality. In comparison to the adult population, childhood onset SLE (cSLE) tends to be more aggressive given the higher preponderance of renal and neuropsychiatric disease and increased disease activity. There is a paucity of literature examining relationship between disease activity, follow up, and health care utilization. The objective of this study is to determine whether early identification of those at risk for loss to follow up would affect compliance with follow-up visits and disease morbidity in patients with childhood-onset systemic lupus erythematosus (cSLE).
Methods: Between July 2021 and January 2022 charts of patients < 18 years of age with SLE who met Systemic Lupus International Collaborative Clinics (SLICC) classification criteria were surveilled and those who were not evaluated in clinic in the previous 120-day period were eligible for inclusion. Identified patients were added to a follow up list and subsequently contacted via telephone for re-establishing care within the month, if eligible.Through retrospective chart review, we assessed disease activity (SLE Disease Activity Index) at last clinic visit. Patients were stratified into two cohorts of lower and higher disease activity, with SLE disease activity index (SLEDAI) < 4 and SLEDAI ≥ 4, respectively. Clinical, epidemiological and serological data, as well as markers of disease morbidity including hospitalizations and Emergency Department (ED) visits were reviewed and compared between the two groups using Fisher exact test for categorical variables and Wilcoxon test for continuous variables.
Results: Forty-one patients were included, of which 34 (83%) were female. Median age was 14 years. Statistically significant differences were identified between the groups, to include age at diagnosis (p< 0.001) associated with higher current SLEDAI score. Of the patients reviewed, participants met an average of 4.6/13 SLICC criteria at diagnosis, with several of these criteria noted to be statistically significant between groups (Table 1). Time to follow up (p< 0.001), high dose prednisone use (p=0.04), hospitalizations (p< 0.001) and ED visits (p< 0.001) were found to be associated with higher SLEDAI scores.
Conclusion: Our findings suggest that cSLE patients with current higher disease activity are at risk for disease related morbidity in the setting of follow-up non-adherence. While further studies are required to enhance our understanding of this association, this links the importance of disease-related outcome and outpatient follow-up visits in this particularly vulnerable patient population.
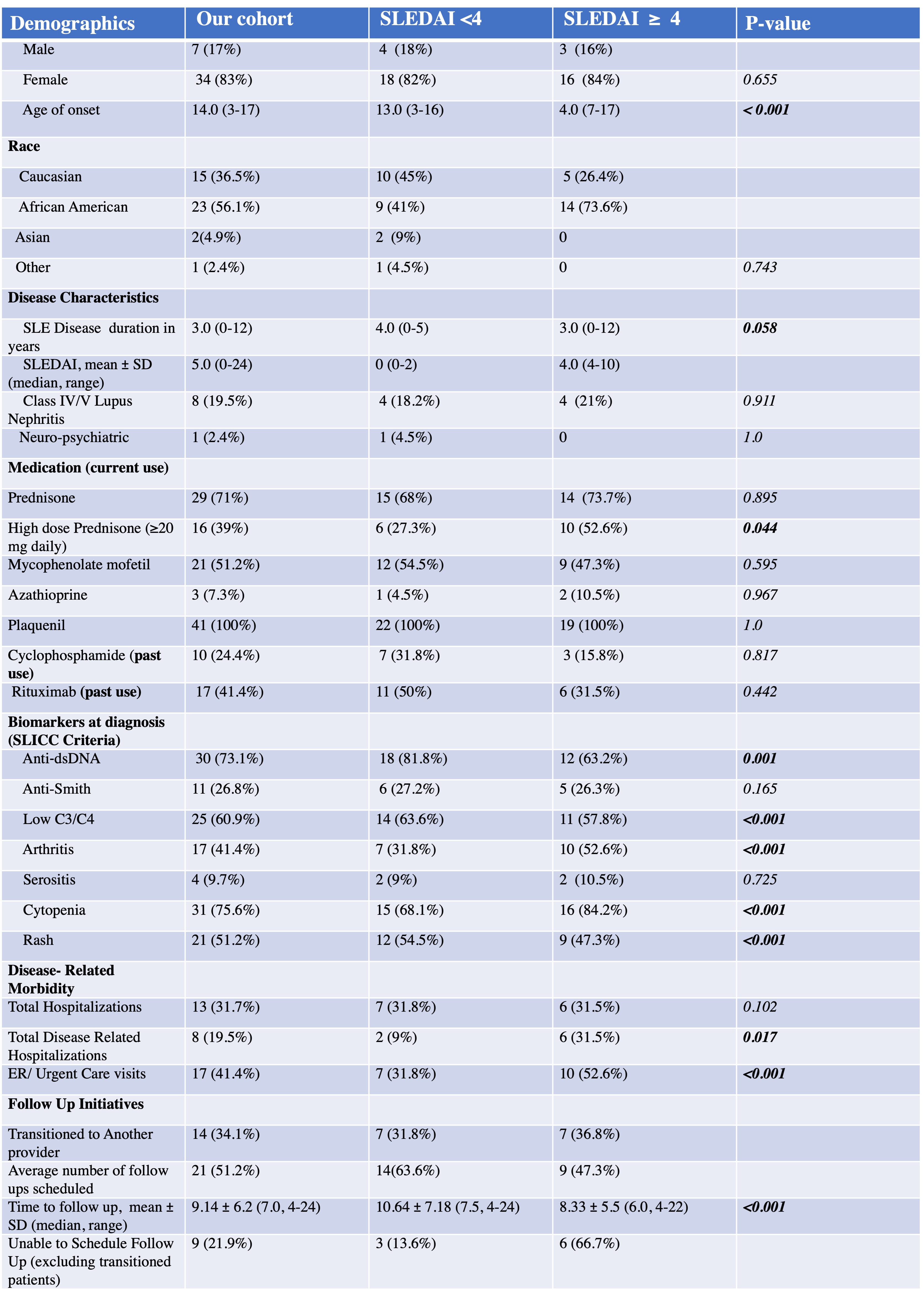 Table 1: Characteristics of cSLE stratified by SLEDAI. This table depicts the patient demographics, clinical features and management of pediatric systemic lupus erythematosus patients for patients stratified be SLEDAI score.
Table 1: Characteristics of cSLE stratified by SLEDAI. This table depicts the patient demographics, clinical features and management of pediatric systemic lupus erythematosus patients for patients stratified be SLEDAI score.Disclosures: M. Nelson, None; C. Mosley, None; D. Villacis-Nunez, None; K. Rouster-Stevens, Accordant; A. Thakral, None.

