Back
Poster Session D
Session: (2052–2107) SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
2074: Poor Executive Function Correlates with Increased Disease Damage and Impaired Patient-Reported Outcomes in Youth with Childhood-Onset Lupus: A Cross-Sectional Study
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall

Tala El Tal, MD
University of Toronto/Hospital for Sick Children
Toronto, ON, Canada
Abstract Poster Presenter(s)
Tala El Tal1, Santiago Arciniegas2, Sarah Mossad3, Ibrahim Mohamed4, Victoria Lishak5, Stephanie Fevrier6, Lawrence Ng3, Paris Moaf3, Joanna Law3, ashley Danguecan3, Linda Hiraki7, Deborah Levy8 and Andrea Knight1, 1The Hospital for Sick Children, Division of Rheumatology, Department of Paediatrics, University of Toronto, Toronto, ON, Canada, 2University of Toronto/Hospital for Sick Children, Toronto, ON, Canada, 3The Hospital for Sick Children, Toronto, ON, Canada, 4The Hospital for Sick Children, Neurosciences and Mental Health, Research Institute, ON, Canada 3Institute of Biomedical Engineering, University of Toronto, Brampton, ON, Canada, 5The Hospital for Sick Children, Department of Psychology, University of Toronto, Toronto, ON, Canada, 6The Hospital for Sick Children/University of Toronto, Toronto, ON, Canada, 7The Hospital for Sick Children, Division of Rheumatology, Department of Paediatrics, University of Toronto, Genetics and Genome Biology, SickKids Research Institute, Toronto, ON, Canada, 8Division of Rheumatology, The Hospital for Sick Children; Child Health Evaluative Services, SickKids Research Institute; Department of Paediatrics, University of Toronto, Toronto, ON, Canada
Background/Purpose: Cognitive dysfunction affects up to 60% of youth with childhood-onset systemic lupus erythematosus (cSLE), particularly executive dysfunction (ED), with adverse effects on treatment adherence, and quality of life. While ED can be a feature of neuropsychiatric SLE, other factors may contribute such as pain, sleep disturbance, fatigue and depression, which can make attribution of ED to SLE challenging. We aimed to examine: 1) the prevalence of ED in cSLE, and 2) its relationship to disease-related factors and patient-reported outcomes.
Methods: We examined a cross-sectional sample of patients with cSLE (ages 12-17, met ACR or SLICC classification criteria for SLE), along with age and sex-matched healthy controls. Participants completed Behavior Rating Inventory of Executive Function 2 (BRIEF-2) that generated a total score global executive composite (GEC), made up of three sub-indices – cognitive regulation index (CRI), emotion regulation index (ERI), and behavioral regulation index (BRI). Patient-Reported Outcomes Measurement Information System (PROMIS) questionnaires for pain behavior, pain interference, sleep disturbance, fatigue, depression and anxiety were completed. Disease measures including SLE Disease Activity Index 2000 (SLEDAI-2K), SLICC/ACR damage index (SDI), glucocorticoid exposure, and disease duration were collected. The primary outcome was ED measured by GEC, further categorized by severity – mild, moderate, and severe difficulties defined as 1.5 >T-score≥1, 2 >T-score≥1.5, and ≥2 standard deviation (SD) below normative mean, respectively. Associations of GEC, disease-related factors and PROMIS measures were assessed using Spearman's rank correlation coefficient. Multivariable partial least squares (PLS) analyses were used to investigate whether disease and PROMIS measures predicted GEC, CRI, ERI, BRI separately.
Results: Twenty-eight patients with cSLE (mean age 15.8 ± SD 1.5 years, 86% female, median SLEDAI-2K score 2 (IQR 2-4) and median disease duration 1.9 years (IQR 1.2-3.4)) and 14 controls were included (Table 1). In cSLE patients compared to controls, mild ED was absent in both; moderate ED was present in 21.4% (n=6) vs 23.1% (n=3); severe ED in 21.4% (n=6) vs 15.4% (n=2). There were no significant differences between groups in ED severity (median GEC score 54 ± SD 12.2 vs 58 ± SD 11.8). Yet, certain PROMIS measures (pain behavior, sleep disturbance pain interference, and fatigue) in cSLE significantly correlated with worse GEC T-scores vs. no correlations found in controls (Table 2). Additionally, no correlations found with disease measures. In the PLS models, increased SDI and pain predicted worse executive function in all areas (GEC, CRI, ERI, and BRI) (Figure 1). Less steroid use at visit predicted worse GEC, ERI and BRI, while shorter disease duration, worse fatigue and sleep disturbance predicted worse CRI.
Conclusion: In this cSLE sample, almost half of patients had at least moderate to severe ED, which significantly correlated with disease damage and patient-reported pain, sleep disturbance and fatigue. More research is needed to identify at-risk groups and targeted intervention for ED.
.jpg) Table 1: cSLE Demographics, Disease Characteristics, and Patient-Reported Outcomes
Table 1: cSLE Demographics, Disease Characteristics, and Patient-Reported Outcomes
.jpg) Table 2: Spearmen correlations between Global Executive Composite (GEC) T scores and disease-related factors, and PROMIS measures.
Table 2: Spearmen correlations between Global Executive Composite (GEC) T scores and disease-related factors, and PROMIS measures.
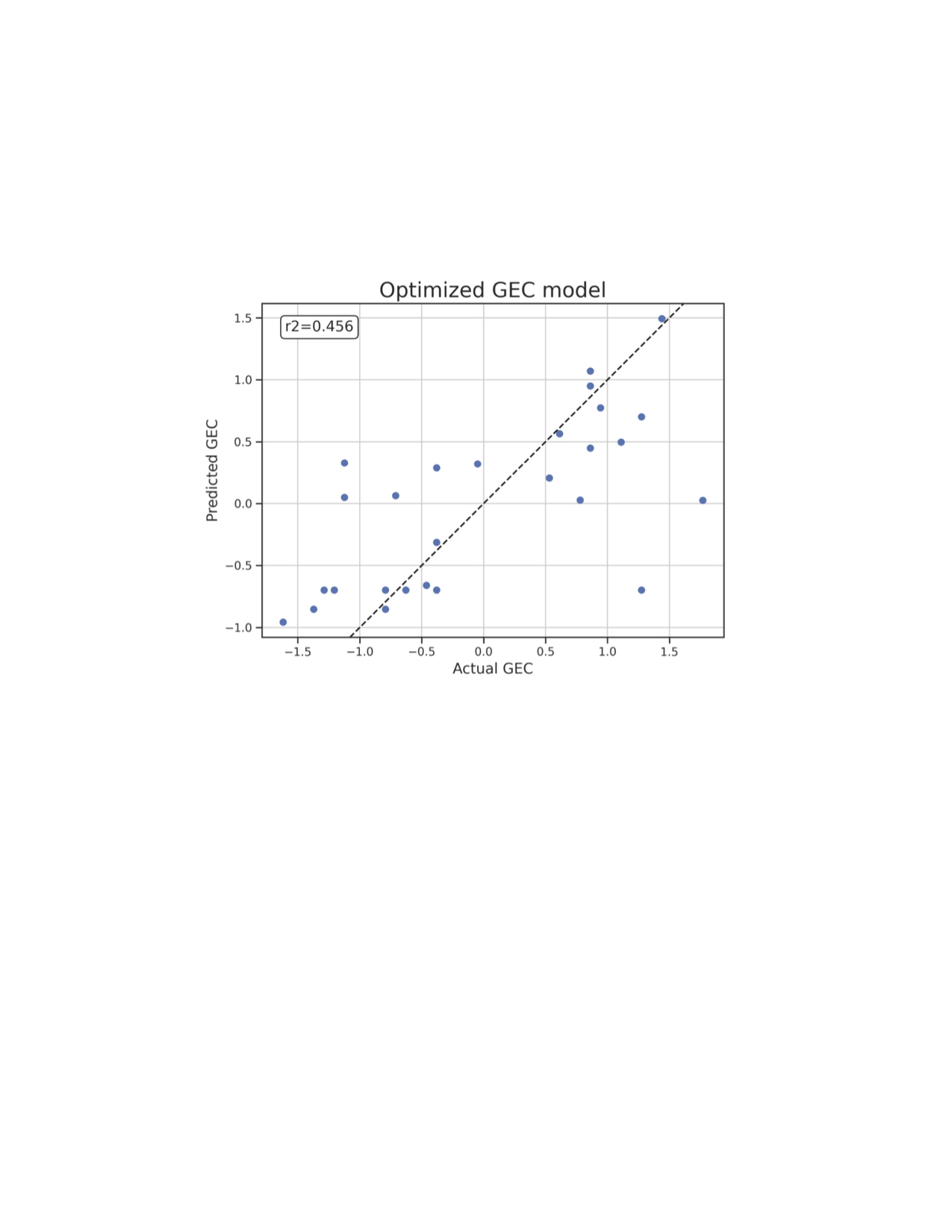 Partial Least Square (PLS2) regression analysis enables description of interactions between multivariate and potentially collinear data with a relatively small sample size. Each predictor’s relevance criterium was based on the bootstrapped sample distribution of its variable importance in projection (VIP) value (significant if VIP > 1, CI = 95%). Relevant predictors for this model include SDI (coeff =0.58), pain behavior (coeff=0.41), and steroid use at visit (coeff=-0.38) and pain interference (coeff=0.35) ranked based on coefficients (coeff). Increased SDI and pain but less steroid use at visit predicts worse GEC scores.
Partial Least Square (PLS2) regression analysis enables description of interactions between multivariate and potentially collinear data with a relatively small sample size. Each predictor’s relevance criterium was based on the bootstrapped sample distribution of its variable importance in projection (VIP) value (significant if VIP > 1, CI = 95%). Relevant predictors for this model include SDI (coeff =0.58), pain behavior (coeff=0.41), and steroid use at visit (coeff=-0.38) and pain interference (coeff=0.35) ranked based on coefficients (coeff). Increased SDI and pain but less steroid use at visit predicts worse GEC scores.
Disclosures: T. El Tal, None; S. Arciniegas, None; S. Mossad, None; I. Mohamed, None; V. Lishak, None; S. Fevrier, None; L. Ng, None; P. Moaf, None; J. Law, None; a. Danguecan, None; L. Hiraki, None; D. Levy, None; A. Knight, None.
Background/Purpose: Cognitive dysfunction affects up to 60% of youth with childhood-onset systemic lupus erythematosus (cSLE), particularly executive dysfunction (ED), with adverse effects on treatment adherence, and quality of life. While ED can be a feature of neuropsychiatric SLE, other factors may contribute such as pain, sleep disturbance, fatigue and depression, which can make attribution of ED to SLE challenging. We aimed to examine: 1) the prevalence of ED in cSLE, and 2) its relationship to disease-related factors and patient-reported outcomes.
Methods: We examined a cross-sectional sample of patients with cSLE (ages 12-17, met ACR or SLICC classification criteria for SLE), along with age and sex-matched healthy controls. Participants completed Behavior Rating Inventory of Executive Function 2 (BRIEF-2) that generated a total score global executive composite (GEC), made up of three sub-indices – cognitive regulation index (CRI), emotion regulation index (ERI), and behavioral regulation index (BRI). Patient-Reported Outcomes Measurement Information System (PROMIS) questionnaires for pain behavior, pain interference, sleep disturbance, fatigue, depression and anxiety were completed. Disease measures including SLE Disease Activity Index 2000 (SLEDAI-2K), SLICC/ACR damage index (SDI), glucocorticoid exposure, and disease duration were collected. The primary outcome was ED measured by GEC, further categorized by severity – mild, moderate, and severe difficulties defined as 1.5 >T-score≥1, 2 >T-score≥1.5, and ≥2 standard deviation (SD) below normative mean, respectively. Associations of GEC, disease-related factors and PROMIS measures were assessed using Spearman's rank correlation coefficient. Multivariable partial least squares (PLS) analyses were used to investigate whether disease and PROMIS measures predicted GEC, CRI, ERI, BRI separately.
Results: Twenty-eight patients with cSLE (mean age 15.8 ± SD 1.5 years, 86% female, median SLEDAI-2K score 2 (IQR 2-4) and median disease duration 1.9 years (IQR 1.2-3.4)) and 14 controls were included (Table 1). In cSLE patients compared to controls, mild ED was absent in both; moderate ED was present in 21.4% (n=6) vs 23.1% (n=3); severe ED in 21.4% (n=6) vs 15.4% (n=2). There were no significant differences between groups in ED severity (median GEC score 54 ± SD 12.2 vs 58 ± SD 11.8). Yet, certain PROMIS measures (pain behavior, sleep disturbance pain interference, and fatigue) in cSLE significantly correlated with worse GEC T-scores vs. no correlations found in controls (Table 2). Additionally, no correlations found with disease measures. In the PLS models, increased SDI and pain predicted worse executive function in all areas (GEC, CRI, ERI, and BRI) (Figure 1). Less steroid use at visit predicted worse GEC, ERI and BRI, while shorter disease duration, worse fatigue and sleep disturbance predicted worse CRI.
Conclusion: In this cSLE sample, almost half of patients had at least moderate to severe ED, which significantly correlated with disease damage and patient-reported pain, sleep disturbance and fatigue. More research is needed to identify at-risk groups and targeted intervention for ED.
.jpg) Table 1: cSLE Demographics, Disease Characteristics, and Patient-Reported Outcomes
Table 1: cSLE Demographics, Disease Characteristics, and Patient-Reported Outcomes .jpg) Table 2: Spearmen correlations between Global Executive Composite (GEC) T scores and disease-related factors, and PROMIS measures.
Table 2: Spearmen correlations between Global Executive Composite (GEC) T scores and disease-related factors, and PROMIS measures. 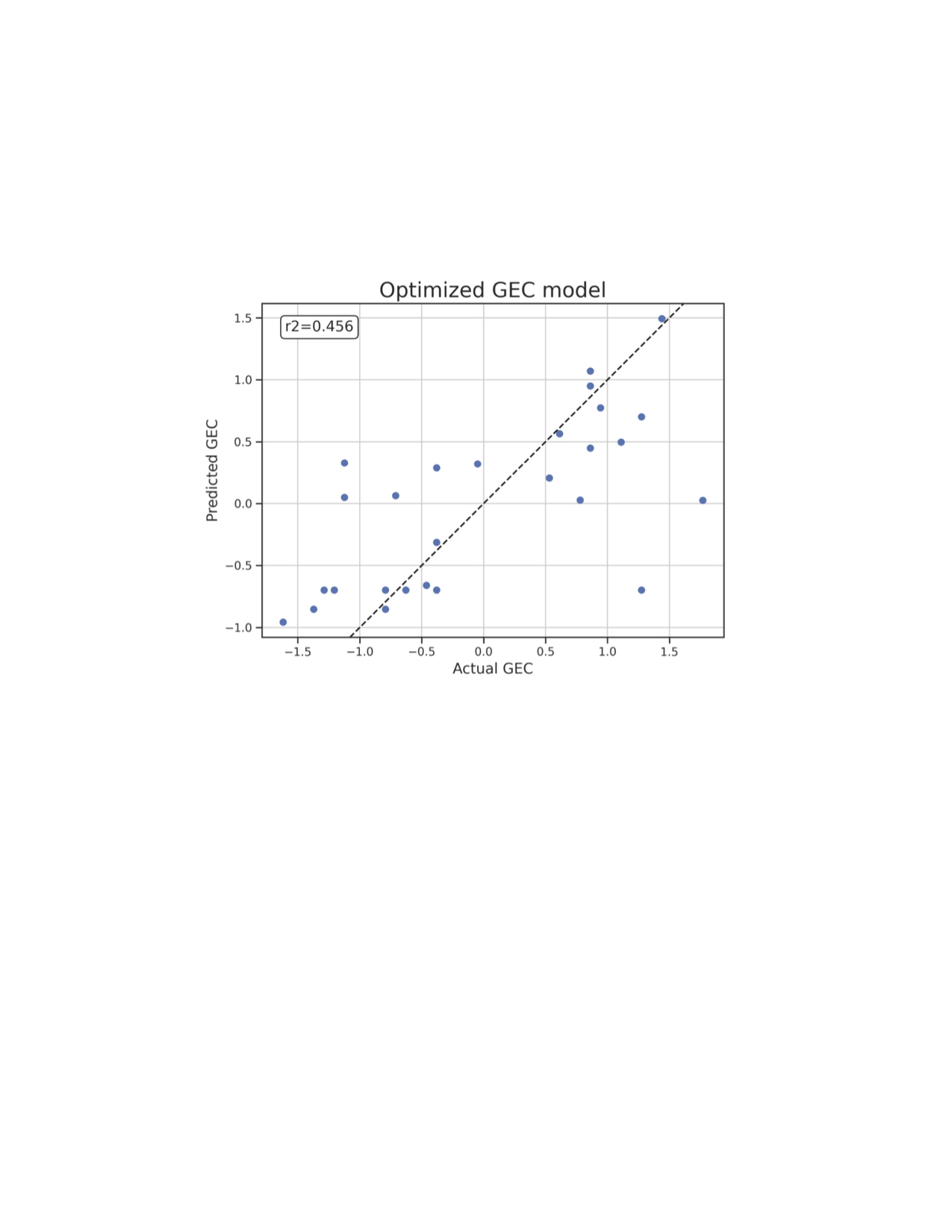 Partial Least Square (PLS2) regression analysis enables description of interactions between multivariate and potentially collinear data with a relatively small sample size. Each predictor’s relevance criterium was based on the bootstrapped sample distribution of its variable importance in projection (VIP) value (significant if VIP > 1, CI = 95%). Relevant predictors for this model include SDI (coeff =0.58), pain behavior (coeff=0.41), and steroid use at visit (coeff=-0.38) and pain interference (coeff=0.35) ranked based on coefficients (coeff). Increased SDI and pain but less steroid use at visit predicts worse GEC scores.
Partial Least Square (PLS2) regression analysis enables description of interactions between multivariate and potentially collinear data with a relatively small sample size. Each predictor’s relevance criterium was based on the bootstrapped sample distribution of its variable importance in projection (VIP) value (significant if VIP > 1, CI = 95%). Relevant predictors for this model include SDI (coeff =0.58), pain behavior (coeff=0.41), and steroid use at visit (coeff=-0.38) and pain interference (coeff=0.35) ranked based on coefficients (coeff). Increased SDI and pain but less steroid use at visit predicts worse GEC scores. Disclosures: T. El Tal, None; S. Arciniegas, None; S. Mossad, None; I. Mohamed, None; V. Lishak, None; S. Fevrier, None; L. Ng, None; P. Moaf, None; J. Law, None; a. Danguecan, None; L. Hiraki, None; D. Levy, None; A. Knight, None.

