Back
Poster Session B
Antiphospholipid Syndrome
Session: (0671–0694) Antiphospholipid Syndrome Poster
0686: Anti-β2GP1/HLA-DR Antibody Is Associated with Arterial Thrombosis in Female Patients with Connective Tissue Diseases: A Cross-Sectional Study in Japan
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- KY
Katsuhiko Yoneda, MD
Kobe University Graduate School of Medicine
Kobe, Japan
Abstract Poster Presenter(s)
Katsuhiko Yoneda1, Yo Ueda1, Kenji Tanimura2, Hirotaka Yamada1, Takaichi Okano3, Keisuke Nishimura1, Hisashi Arase4, Hideto Yamada5 and Jun Saegusa1, 1Rheumatology and Clinical Immunology, Kobe University Graduate School of Medicine, Kobe, Japan, 2Department of Obstetrics and Gynecology, Kobe University Hospital, Kobe, Japan, 3Kobe University Hospital, Kobe, Japan, 4Department of Immunochemistry, Research Institute for Microbial Disease, Osaka University, Suita, Japan, 5Department of Obstetrics and Gynecology, Kobe University Hospital / Center for Recurrent Pregnancy Loss, Teine Keijinkai Hospital, Sapporo, Japan
Background/Purpose: Antiphospholipid syndrome (APS) is an autoimmune disorder characterized by thrombosis and/or pregnancy complications. Recently, β2-glycoprotein I (β2GPI) complexed with HLA class II molecules (β2GPI/HLA-DR) was found to be a major autoantibody target in APS. The purpose of this study is to reveal the association between anti-β2GPI/HLA-DR antibody and arterial thrombosis in women with connective tissue diseases.
Methods: Blood samples from female outpatients with connective tissue diseases between 2020-2021 were collected to measure anti-β2GPI/HLA-DR antibody and anti-phospholipid antibody (aPL) panel including anti-cardiolipin (aCL) IgG/IgM and anti-β2GPI IgG/IgM. Clinical and laboratory data about the underlying disease, thrombotic episodes, and comorbidities known as risk factors for arterial thrombosis were retrieved from medical records and patient questionaries. Anti-β2GPI/HLA-DR antibody titers were compared to the results of aPL panel assay and adjusted global APS score (aGAPSS), as a composite measure to estimate the risk of arterial thrombosis. The cutoff titer of anti-β2GPI/HLA-DR antibody was calculated to estimate the risk of arterial thrombosis by using receiver operating characteristic (ROC) analysis. Finally, we assessed the impact of anti-β2GPI/HLA-DR antibody on arterial thrombosis in addition to the conventional risk factors.
Results: Samples were collected and analyzed with 704 patients, that include 260 SLE or MCTD, 180 RA, 59 systemic sclerosis, 57 idiopathic inflammatory myopathies, 38 large vessel vasculitis, 36 ANCA-associated vasculitis, 30 Behçet's disease. Sixty-six patients fulfilled the APS classification criteria. Seventy-seven patients had history of arterial thrombosis, and 14 patients among them also had the history of venous thrombosis. Anti-β2GPI/HLA-DR antibody titers were significantly high in patients who had history of both arterial and venous thrombosis than those of no thrombosis. In cases with aGAPSS >10 or triple positivity of aPL, the titers of anti-β2GPI/HLA-DR antibody tended to be higher. The ROC test showed the sensitivity, the specificity, and the area under the curve (AUC) for arterial thrombosis were 33.8%, 91.4%, and 0.6009 with the cutoff value, 172.359 (Figure 1). When using this cutoff titer, adding the positivity of anti-β2GP1/HLA-DR antibody to the conventional risk factors improved the AUC from 0.677 to 0.730 (p = 0.0878) (Figure 2). Determined net reclassification improvement (NRI) and integrated discrimination improvement (IDI) were statistically significant. By the multivariable logistic regression analysis with multiple imputation, the odds ratio of the positivity of anti-β2GP1/HLA-DR antibody for arterial thrombosis was 5.11 (95% confidence interval: 2.84-9.19; P< 0.001) (Table 1).
Conclusion: Anti-β2GP1/HLA-DR antibody is suggested to be associated with arterial thrombosis in female patients with connective tissue diseases.
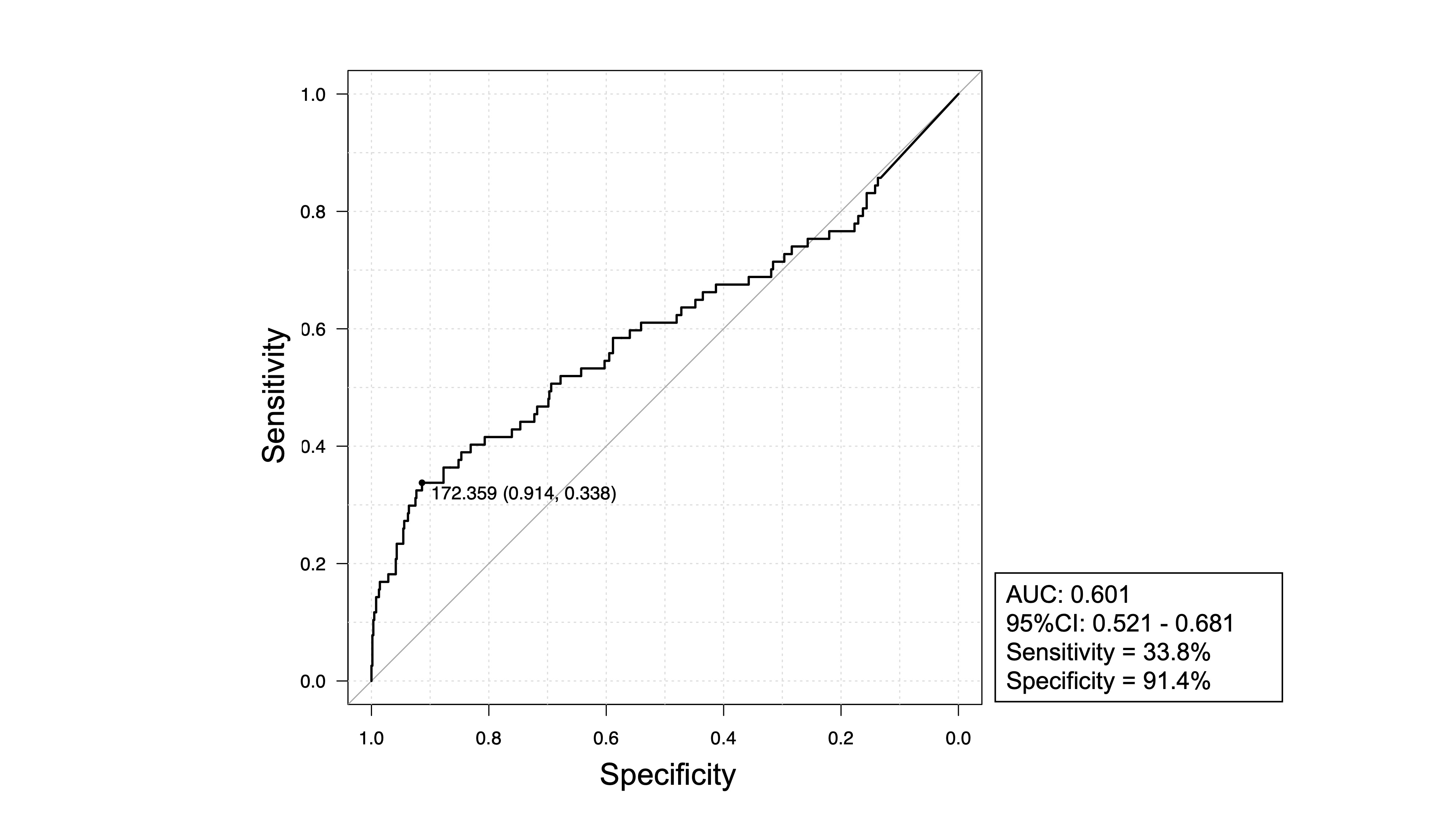 Figure.1: receiver operating characteristic (ROC) curve analysis
Figure.1: receiver operating characteristic (ROC) curve analysis
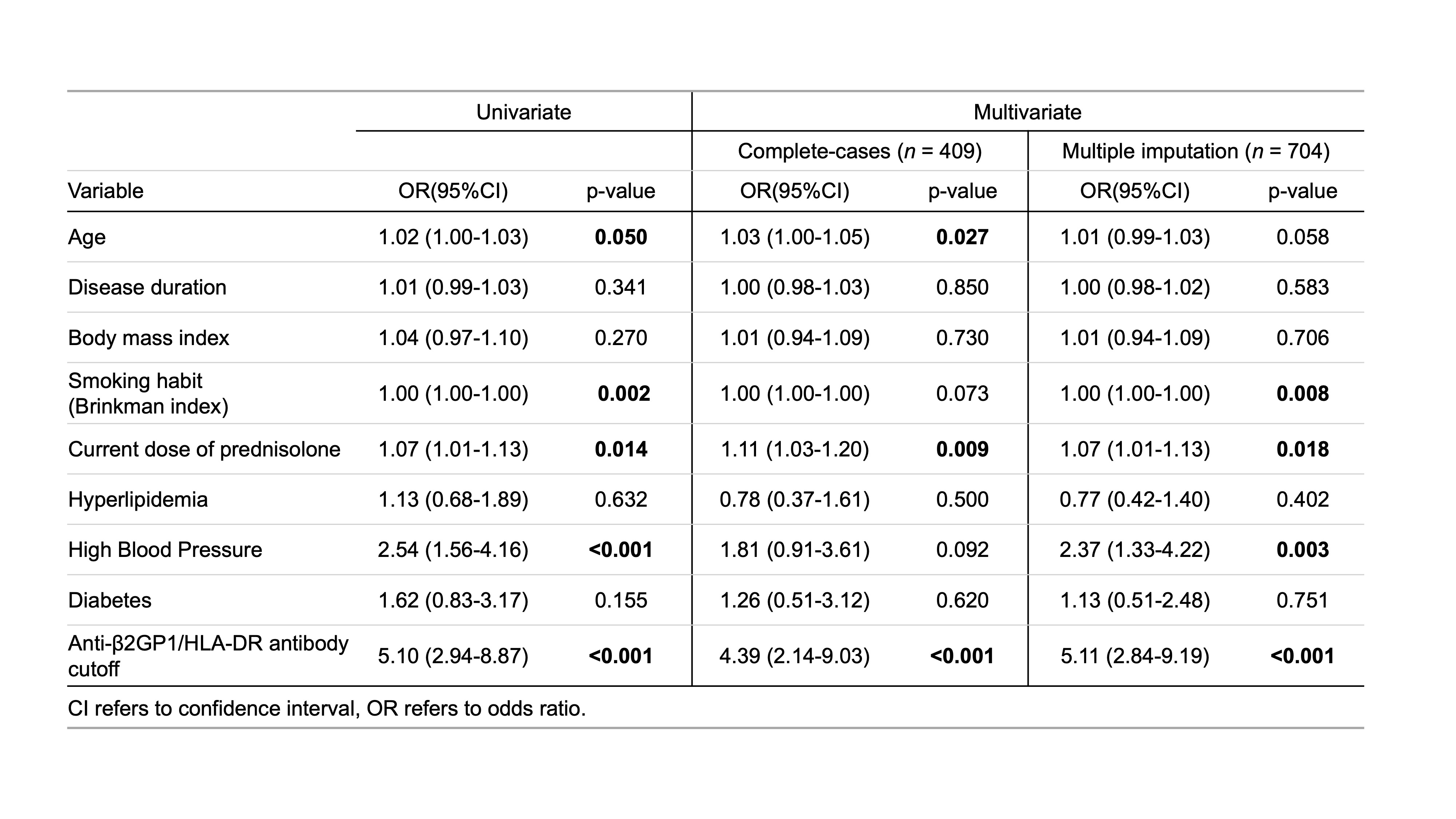 Table.1: logistic regression analysis
Table.1: logistic regression analysis
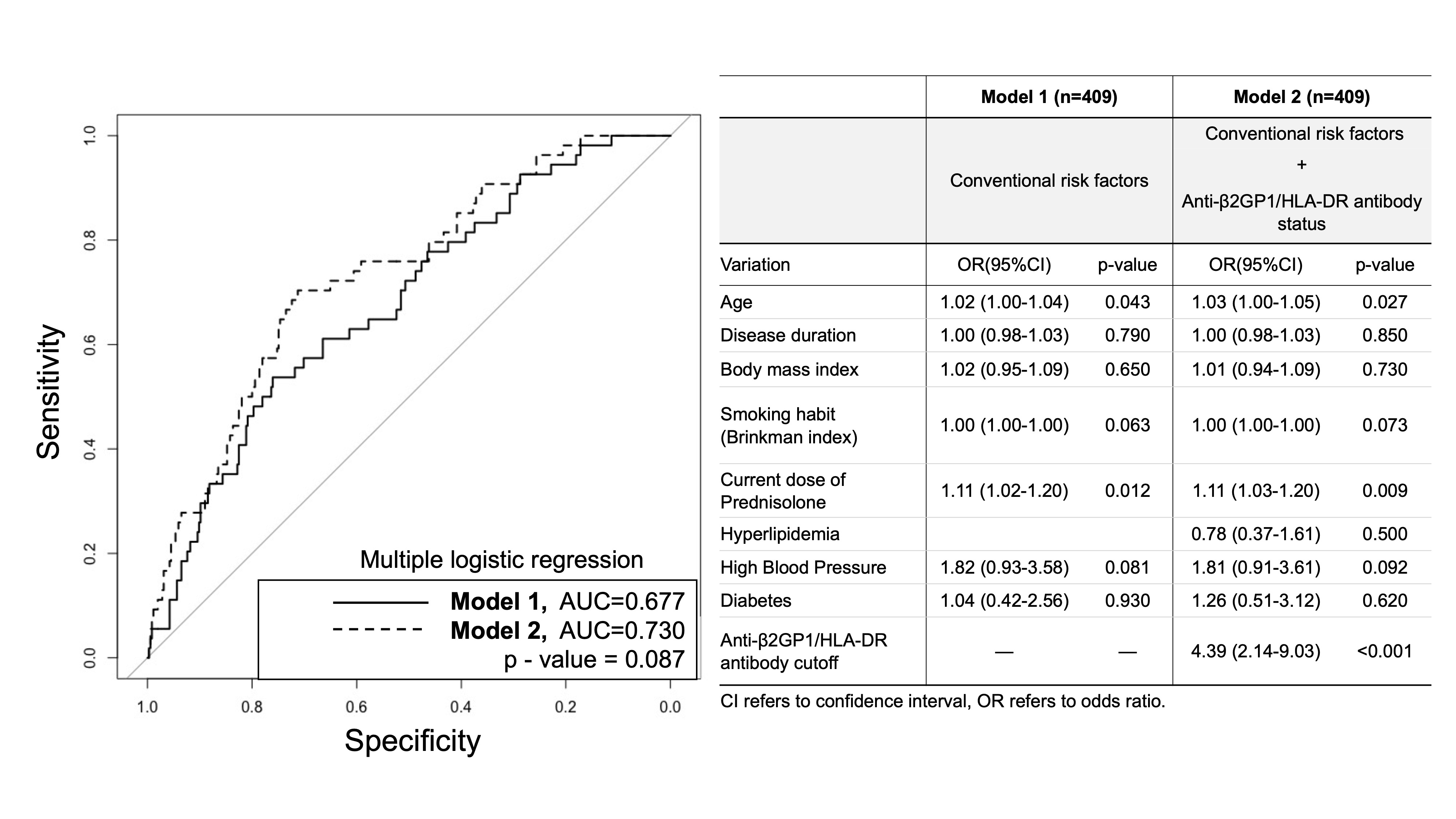 Figure.2: ROC curves for conventional risk model and the model that adds anti-β2GP1/HLA-DR antibody-cutoff status
Figure.2: ROC curves for conventional risk model and the model that adds anti-β2GP1/HLA-DR antibody-cutoff status
Disclosures: K. Yoneda, None; Y. Ueda, None; K. Tanimura, None; H. Yamada, None; T. Okano, None; K. Nishimura, None; H. Arase, None; H. Yamada, None; J. Saegusa, None.
Background/Purpose: Antiphospholipid syndrome (APS) is an autoimmune disorder characterized by thrombosis and/or pregnancy complications. Recently, β2-glycoprotein I (β2GPI) complexed with HLA class II molecules (β2GPI/HLA-DR) was found to be a major autoantibody target in APS. The purpose of this study is to reveal the association between anti-β2GPI/HLA-DR antibody and arterial thrombosis in women with connective tissue diseases.
Methods: Blood samples from female outpatients with connective tissue diseases between 2020-2021 were collected to measure anti-β2GPI/HLA-DR antibody and anti-phospholipid antibody (aPL) panel including anti-cardiolipin (aCL) IgG/IgM and anti-β2GPI IgG/IgM. Clinical and laboratory data about the underlying disease, thrombotic episodes, and comorbidities known as risk factors for arterial thrombosis were retrieved from medical records and patient questionaries. Anti-β2GPI/HLA-DR antibody titers were compared to the results of aPL panel assay and adjusted global APS score (aGAPSS), as a composite measure to estimate the risk of arterial thrombosis. The cutoff titer of anti-β2GPI/HLA-DR antibody was calculated to estimate the risk of arterial thrombosis by using receiver operating characteristic (ROC) analysis. Finally, we assessed the impact of anti-β2GPI/HLA-DR antibody on arterial thrombosis in addition to the conventional risk factors.
Results: Samples were collected and analyzed with 704 patients, that include 260 SLE or MCTD, 180 RA, 59 systemic sclerosis, 57 idiopathic inflammatory myopathies, 38 large vessel vasculitis, 36 ANCA-associated vasculitis, 30 Behçet's disease. Sixty-six patients fulfilled the APS classification criteria. Seventy-seven patients had history of arterial thrombosis, and 14 patients among them also had the history of venous thrombosis. Anti-β2GPI/HLA-DR antibody titers were significantly high in patients who had history of both arterial and venous thrombosis than those of no thrombosis. In cases with aGAPSS >10 or triple positivity of aPL, the titers of anti-β2GPI/HLA-DR antibody tended to be higher. The ROC test showed the sensitivity, the specificity, and the area under the curve (AUC) for arterial thrombosis were 33.8%, 91.4%, and 0.6009 with the cutoff value, 172.359 (Figure 1). When using this cutoff titer, adding the positivity of anti-β2GP1/HLA-DR antibody to the conventional risk factors improved the AUC from 0.677 to 0.730 (p = 0.0878) (Figure 2). Determined net reclassification improvement (NRI) and integrated discrimination improvement (IDI) were statistically significant. By the multivariable logistic regression analysis with multiple imputation, the odds ratio of the positivity of anti-β2GP1/HLA-DR antibody for arterial thrombosis was 5.11 (95% confidence interval: 2.84-9.19; P< 0.001) (Table 1).
Conclusion: Anti-β2GP1/HLA-DR antibody is suggested to be associated with arterial thrombosis in female patients with connective tissue diseases.
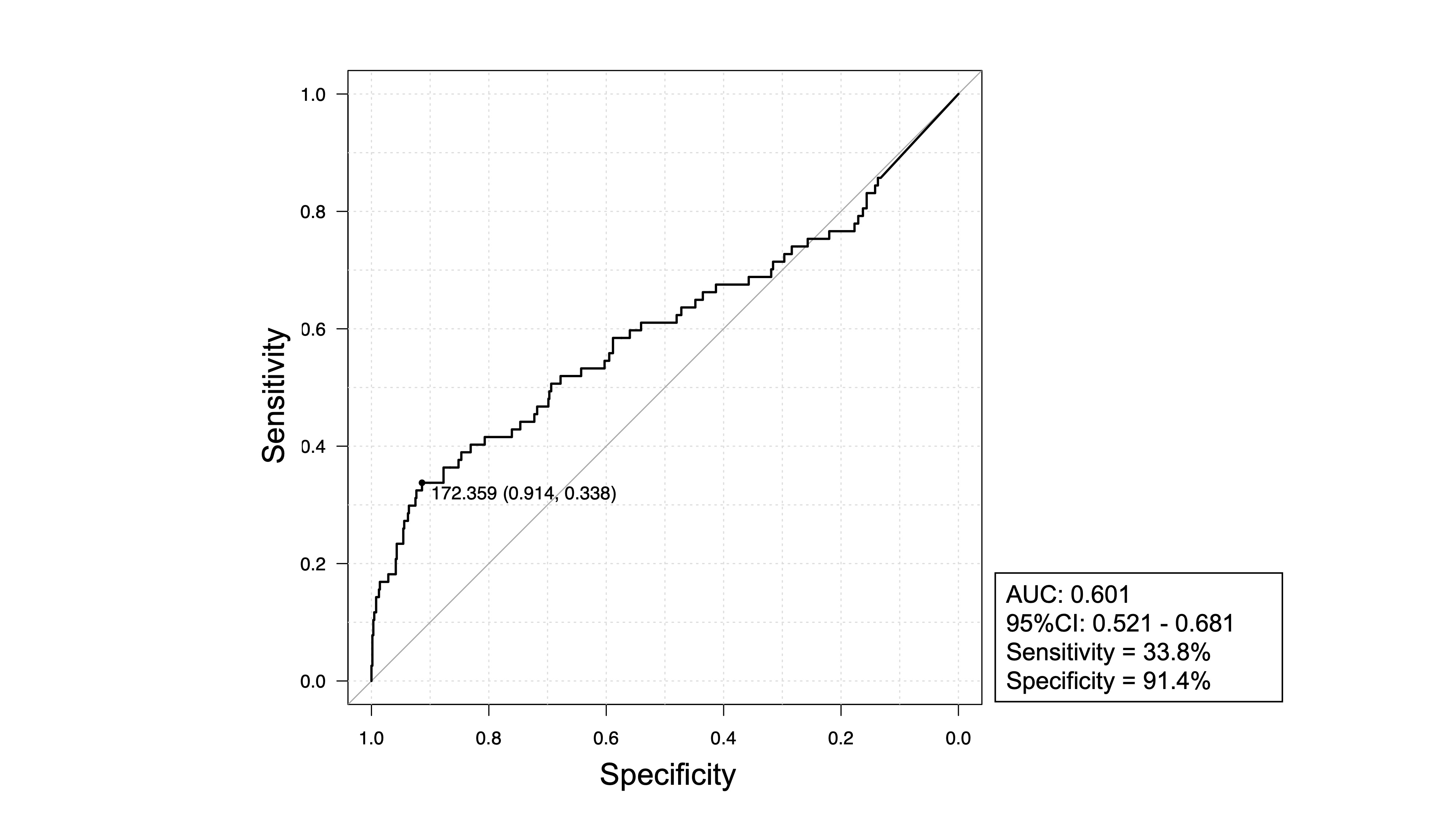 Figure.1: receiver operating characteristic (ROC) curve analysis
Figure.1: receiver operating characteristic (ROC) curve analysis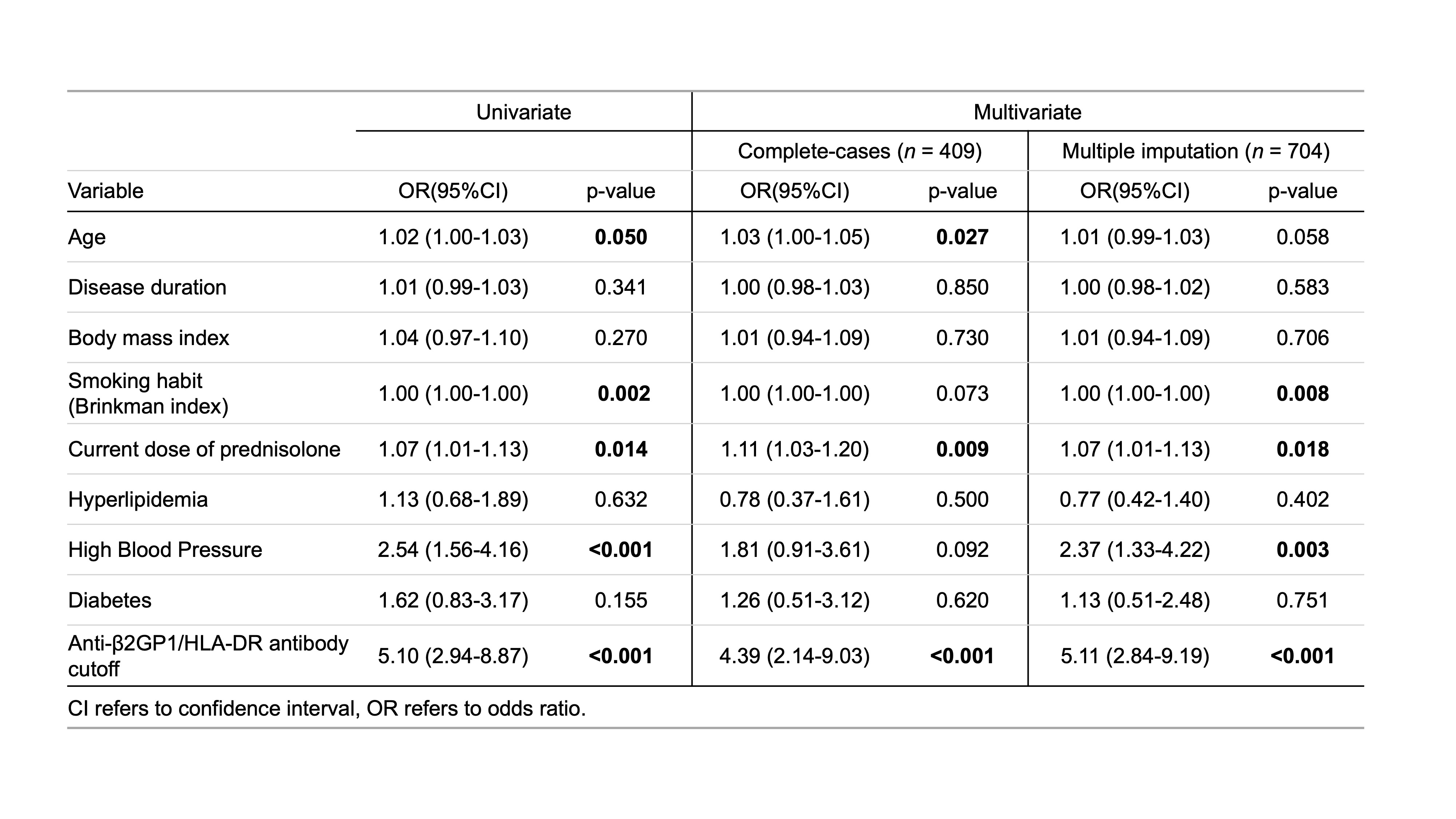 Table.1: logistic regression analysis
Table.1: logistic regression analysis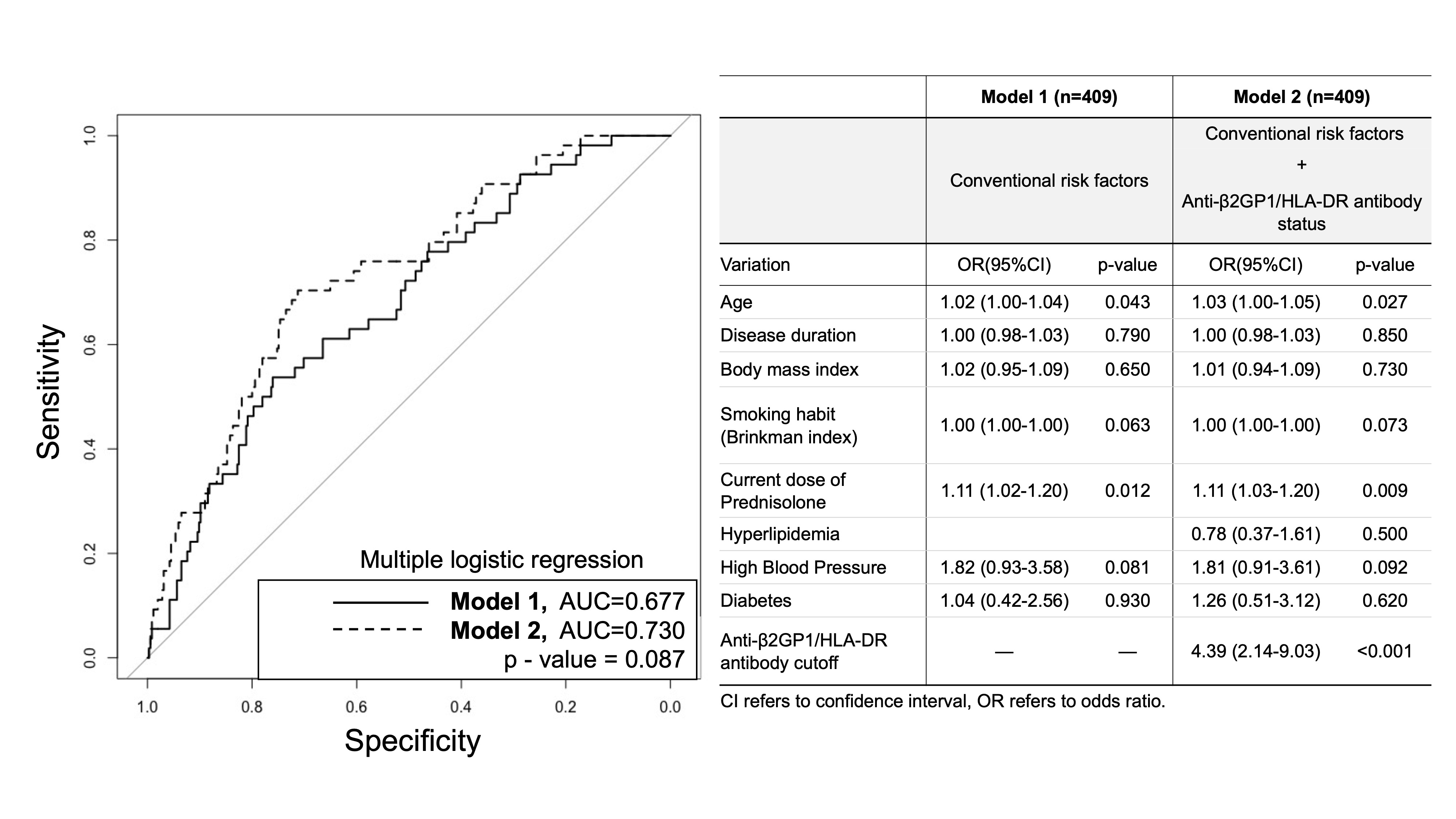 Figure.2: ROC curves for conventional risk model and the model that adds anti-β2GP1/HLA-DR antibody-cutoff status
Figure.2: ROC curves for conventional risk model and the model that adds anti-β2GP1/HLA-DR antibody-cutoff statusDisclosures: K. Yoneda, None; Y. Ueda, None; K. Tanimura, None; H. Yamada, None; T. Okano, None; K. Nishimura, None; H. Arase, None; H. Yamada, None; J. Saegusa, None.

