Back
Poster Session D
Session: (2052–2107) SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
2075: Risk of Bloodstream Infection in Patients with Systemic Lupus Erythematosus Exposed to Prolonged Moderate to High Dose Glucocorticoids
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- MK
Mi Hyeon Kim, MD
Seoul National University Hospital
Seocho-gu, Seoul, South Korea
Abstract Poster Presenter(s)
MI HYEON KIM1, Eun Bong Lee1, Eun Young Lee2, Jin Kyun Park3 and Jun Won Park1, 1Seoul National University Hospital, Seoul, Republic of Korea, 2Seoul National University College of Medicine, Seoul, Republic of Korea, 3Seoul National University College of Medicine, Jongno-gu, Seoul, South Korea
Background/Purpose: This study aimed to investigate the incidence and risk factors of bloodstream infection (BSI) in patients with systemic lupus erythematosus (SLE) receiving moderate-to-high dose of glucocorticoids.
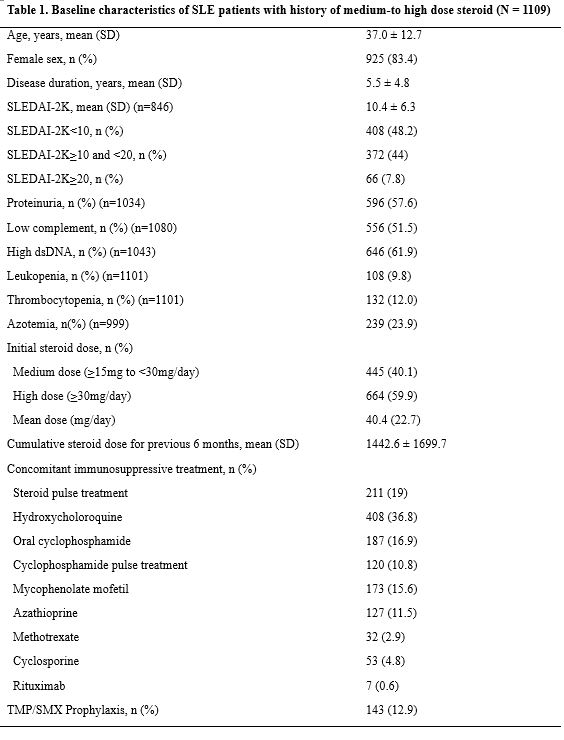
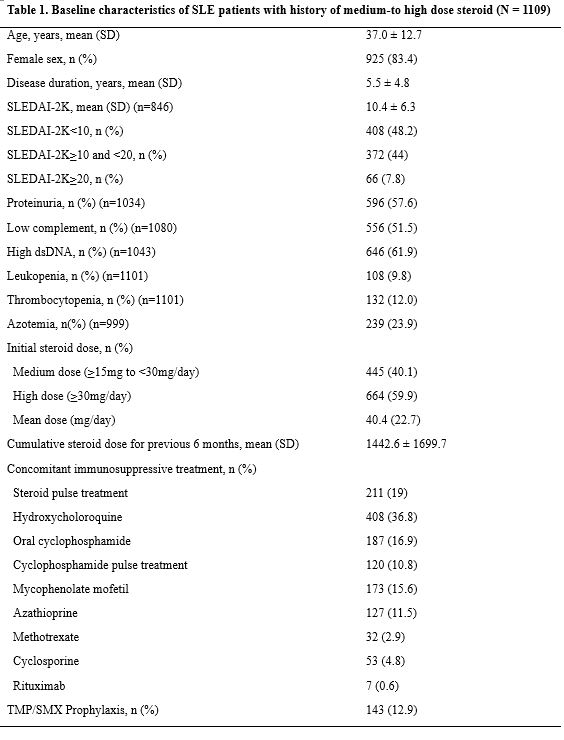
Methods: This study included 1109 treatment episodes with prolonged (≥4 weeks), moderate-to-high dose glucocorticoids (≥ 15mg/day prednisolone) in 612 patients with SLE over 14-year period. All patients were fulfilled four or more of the 1997 ACR revised classification criteria for SLE. Clinical features regarding disease activity (SLEDAI-2K), immunosuppressant use and laboratory results were collected from the electronic medical database. Baseline date was defined as the date of initiating moderate-to-high dose steroid and observation period was 1 year from the baseline date. Incidence rate and risk factors for BSI were investigated using generalized estimating equation poisson regression.
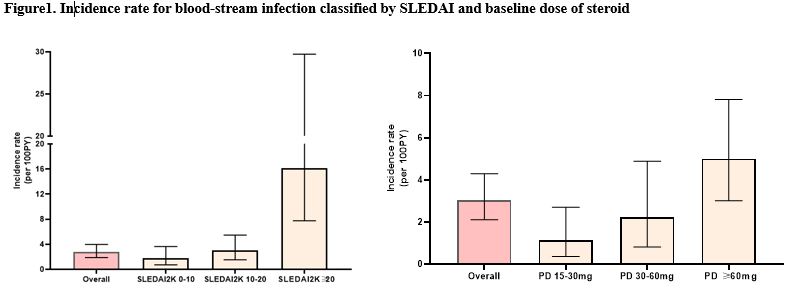
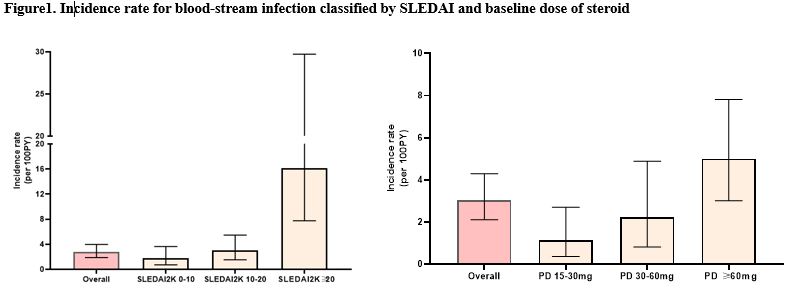
Results: During a total of 1078.64 person-years, 30 cases of BSI occurred in 27 treatment episodes, with an incidence rate of 2.78 [95% confidence interval (CI) 1.88 - 3.97] per 100 person-years. When the incidence rate was stratified by baseline steroid dose and SLEDAI-2K score, higher incidence of BSI occurred with the higher dose of baseline steroid and disease activity score. Treatment episodes with SLEDAI-2K≥20 showed remarkably high incidence rate. In the multivariable analysis, SLEDAI-2K≥20 (incidence rate ratio [IRR]: 5.54, 95% CI 2.56-11.99), cumulative prednisolone≥15mg/day for previous 6 months (IRR 2.66, 95% CI 1.36-5.22) and initial prednisolone≥60mg/day (IRR 2.52, 95% CI 1.18-5.44) were highly associated with increased risk of the BSI. The trimethoprim–sulfamethoxazole(TMP-SMX) prophylaxis was associated with a lower incidence of BSI (IRR 0.42, 95% CI 0.18 to 0.99, p=0.047).
Conclusion: In SLE patients exposed to prolonged moderate-to-high dose glucocorticoids, high disease activity and high intensity of previous and concurrent glucocorticoid use are important factors that increase the risk of BSI. The prophylactic use of TMP-SMX should be considered when initiating high dose glucocorticoids for controlling disease activity in SLE pateints.

Disclosures: M. KIM, None; E. Lee, None; E. Lee, None; J. Park, None; J. Park, None.
Background/Purpose: This study aimed to investigate the incidence and risk factors of bloodstream infection (BSI) in patients with systemic lupus erythematosus (SLE) receiving moderate-to-high dose of glucocorticoids.
Methods: This study included 1109 treatment episodes with prolonged (≥4 weeks), moderate-to-high dose glucocorticoids (≥ 15mg/day prednisolone) in 612 patients with SLE over 14-year period. All patients were fulfilled four or more of the 1997 ACR revised classification criteria for SLE. Clinical features regarding disease activity (SLEDAI-2K), immunosuppressant use and laboratory results were collected from the electronic medical database. Baseline date was defined as the date of initiating moderate-to-high dose steroid and observation period was 1 year from the baseline date. Incidence rate and risk factors for BSI were investigated using generalized estimating equation poisson regression.
Results: During a total of 1078.64 person-years, 30 cases of BSI occurred in 27 treatment episodes, with an incidence rate of 2.78 [95% confidence interval (CI) 1.88 - 3.97] per 100 person-years. When the incidence rate was stratified by baseline steroid dose and SLEDAI-2K score, higher incidence of BSI occurred with the higher dose of baseline steroid and disease activity score. Treatment episodes with SLEDAI-2K≥20 showed remarkably high incidence rate. In the multivariable analysis, SLEDAI-2K≥20 (incidence rate ratio [IRR]: 5.54, 95% CI 2.56-11.99), cumulative prednisolone≥15mg/day for previous 6 months (IRR 2.66, 95% CI 1.36-5.22) and initial prednisolone≥60mg/day (IRR 2.52, 95% CI 1.18-5.44) were highly associated with increased risk of the BSI. The trimethoprim–sulfamethoxazole(TMP-SMX) prophylaxis was associated with a lower incidence of BSI (IRR 0.42, 95% CI 0.18 to 0.99, p=0.047).
Conclusion: In SLE patients exposed to prolonged moderate-to-high dose glucocorticoids, high disease activity and high intensity of previous and concurrent glucocorticoid use are important factors that increase the risk of BSI. The prophylactic use of TMP-SMX should be considered when initiating high dose glucocorticoids for controlling disease activity in SLE pateints.

Disclosures: M. KIM, None; E. Lee, None; E. Lee, None; J. Park, None; J. Park, None.

