Back
Poster Session D
Session: (2052–2107) SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
2065: Sustained B Cell Depletion in Lupus Nephritis Patients After Treatment with a B Cell Agent Is Associated with Fewer Disease Flares
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- DZ
Diane Zisa, MD
Columbia University Irving Medical Center
New York, NY, United States
Abstract Poster Presenter(s)
Diane Zisa1, Jeffrey Zhang-Sun1, Paul Christos2 and Kyriakos Kirou1, 1Hospital for Special Surgery, New York, NY, 2Weill Cornell Medicine/New York-Presbyterian, New York, NY
Background/Purpose: B cell targeting agents (BCA), including belimumab (BEL) and rituximab (RTX), have been used with success in lupus nephritis (LN) patients, though identifying patients at highest risk for flare after receipt of these agents has not been well studied. We hypothesized that sustained low peripheral B cell counts (BCC) after successful control of LN would be associated with fewer LN and severe SLE flares.
Methods: We performed a retrospective chart review of adult patients with LN seen by the authors at an academic center from July 2013 until February 2022. Patients were eligible for inclusion if they were treated for LN with either BEL and/or RTX and had at least two CD19+ B cell measurements in peripheral blood. Those with end-stage renal disease were excluded. All patients were on background standard-of-care (SOC) therapy for LN.
Renal Response (RR) was characterized as either a partial RR (PRR) or complete RR (CRR) according to consensus definitions in the literature. LN flares (LNF) were identified, after at least a PRR was achieved, by an increase in proteinuria to a UPCR >1g/d if CRR was achieved or two times the UPCR and UPCR >2g/d if PRR was achieved. A severe SLE flare (SLEF) was defined as a flare warranting escalation in immunosuppressive therapy.
After B cell depletions occurred, we characterized the subsequent time periods by the corresponding trajectories of BCC. When B cell depletions were sustained at BCC< 100 cells/μL, they were called "type 1" episodes. Episodes marked by repletion of BCC were defined as "type 2" episodes; those with slow repletion to BCC >100 cells/μL in ≥6 months were "type 2a" and those with rapid repletion of BCC in < 6 months were "type 2b." A patient could have more than one type of episode during the study period.
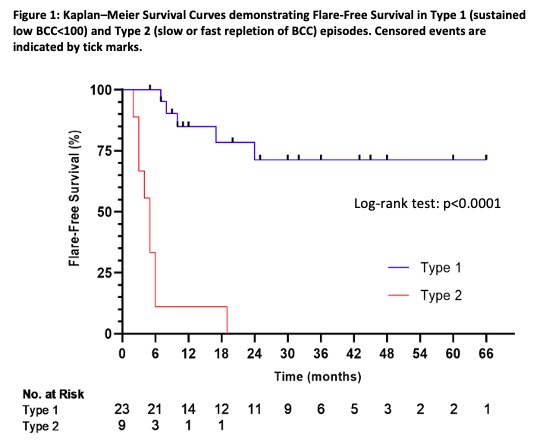
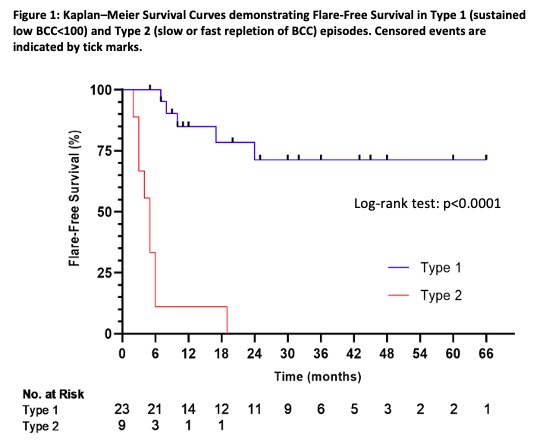
The time from RR until an event, either a LNF or SLEF, or to no event, either at the end of the study period or the end of available patient follow-up, was recorded for each episode type. Descriptive statistics were performed, and Kaplan-Meier survival curves (for event-free survival) were calculated for each episode type. Hazard ratios (HR) and 95% confidence intervals (CI) were also calculated, and the log-rank test was used to compare event-free survival between episode types. An alpha level of 0.05 was used to determine statistical significance.
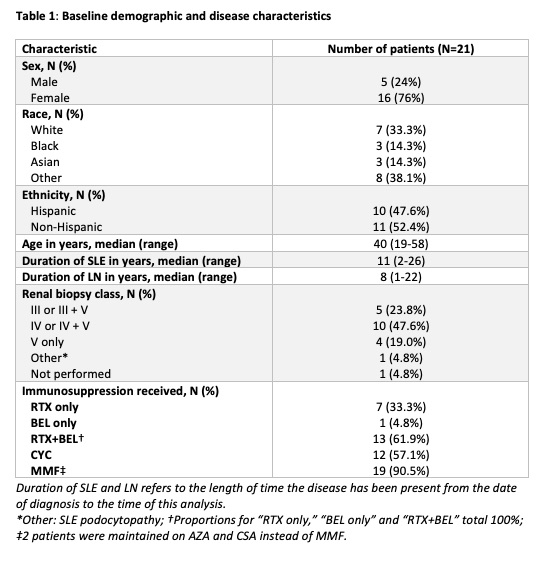
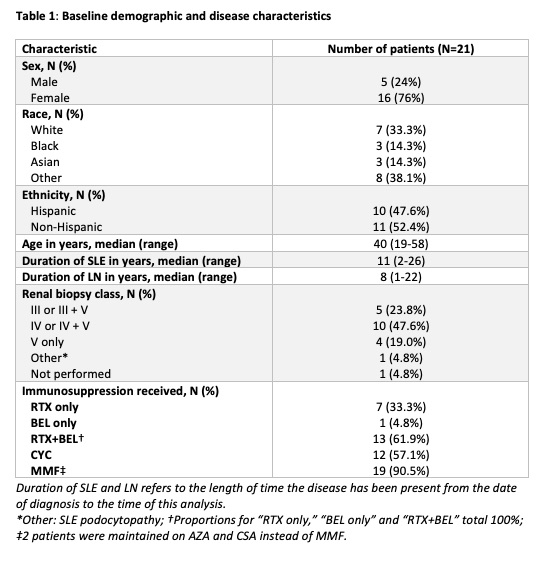
Results: Twenty-one patients were included for analysis (Table 1). There were 32 episodes of B cell depletion experienced by the 21 patients. Twenty-three (71.9%) were type 1 episodes and 9 (28.1%) were type 2 episodes. Of the type 2 episodes, 2 were type 2a and 6 were type 2b; 1 episode could not be further defined.
Flare-free survival significantly differed between type 2 and type 1 episodes, (p < 0.0001) (Fig 1). Compared to type 1 episodes, type 2 episodes had an 11.4 (95% CI 2.5, 52.4) times greater risk for flare over the follow-up period. When type 2 episodes were divided into 2a and 2b, there was a 15.2 (95% CI 1.6, 147) times greater risk of flare for type 2b episodes compared to type 1 episodes.
Conclusion: In our study, repletion of B cells after treatment with BCA, particularly rapid repletion in < 6 months, carries a significantly higher risk of subsequent disease flare when compared to sustained low BCC. Larger studies are needed to confirm our findings.
Disclosures: D. Zisa, None; J. Zhang-Sun, None; P. Christos, None; K. Kirou, None.
Background/Purpose: B cell targeting agents (BCA), including belimumab (BEL) and rituximab (RTX), have been used with success in lupus nephritis (LN) patients, though identifying patients at highest risk for flare after receipt of these agents has not been well studied. We hypothesized that sustained low peripheral B cell counts (BCC) after successful control of LN would be associated with fewer LN and severe SLE flares.
Methods: We performed a retrospective chart review of adult patients with LN seen by the authors at an academic center from July 2013 until February 2022. Patients were eligible for inclusion if they were treated for LN with either BEL and/or RTX and had at least two CD19+ B cell measurements in peripheral blood. Those with end-stage renal disease were excluded. All patients were on background standard-of-care (SOC) therapy for LN.
Renal Response (RR) was characterized as either a partial RR (PRR) or complete RR (CRR) according to consensus definitions in the literature. LN flares (LNF) were identified, after at least a PRR was achieved, by an increase in proteinuria to a UPCR >1g/d if CRR was achieved or two times the UPCR and UPCR >2g/d if PRR was achieved. A severe SLE flare (SLEF) was defined as a flare warranting escalation in immunosuppressive therapy.
After B cell depletions occurred, we characterized the subsequent time periods by the corresponding trajectories of BCC. When B cell depletions were sustained at BCC< 100 cells/μL, they were called "type 1" episodes. Episodes marked by repletion of BCC were defined as "type 2" episodes; those with slow repletion to BCC >100 cells/μL in ≥6 months were "type 2a" and those with rapid repletion of BCC in < 6 months were "type 2b." A patient could have more than one type of episode during the study period.
The time from RR until an event, either a LNF or SLEF, or to no event, either at the end of the study period or the end of available patient follow-up, was recorded for each episode type. Descriptive statistics were performed, and Kaplan-Meier survival curves (for event-free survival) were calculated for each episode type. Hazard ratios (HR) and 95% confidence intervals (CI) were also calculated, and the log-rank test was used to compare event-free survival between episode types. An alpha level of 0.05 was used to determine statistical significance.
Results: Twenty-one patients were included for analysis (Table 1). There were 32 episodes of B cell depletion experienced by the 21 patients. Twenty-three (71.9%) were type 1 episodes and 9 (28.1%) were type 2 episodes. Of the type 2 episodes, 2 were type 2a and 6 were type 2b; 1 episode could not be further defined.
Flare-free survival significantly differed between type 2 and type 1 episodes, (p < 0.0001) (Fig 1). Compared to type 1 episodes, type 2 episodes had an 11.4 (95% CI 2.5, 52.4) times greater risk for flare over the follow-up period. When type 2 episodes were divided into 2a and 2b, there was a 15.2 (95% CI 1.6, 147) times greater risk of flare for type 2b episodes compared to type 1 episodes.
Conclusion: In our study, repletion of B cells after treatment with BCA, particularly rapid repletion in < 6 months, carries a significantly higher risk of subsequent disease flare when compared to sustained low BCC. Larger studies are needed to confirm our findings.
Disclosures: D. Zisa, None; J. Zhang-Sun, None; P. Christos, None; K. Kirou, None.

