Back
Poster Session D
Session: (1830–1855) Miscellaneous Rheumatic and Inflammatory Diseases Poster III
1837: Eales Disease and Vogt-Koyanagi-Harada Syndrome: Not Everything Is Anterior Uveitis in Rheumatology
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SP
Sonia Pastor Navarro, MD
Hospital Universitario de Salamanca
Salamanca, Spain
Abstract Poster Presenter(s)
Sonia Pastor Navarro1, Olga Compán Fernández1, Marta Ibáñez Martínez1, Belén Miguel Ibáñez1, Mireia Molina Pérez2, Ángel Beltrán Mazo2, Olga Martínez González1, Carlos Montilla Morales1, Ana Isabel Turrión Nieves1, Susana Gómez Castro3 and Cristina Hidalgo Calleja1, 1Hospital Universitario de Salamanca, Salamanca, Spain, 2Hospital Universitario de Salamanca, Salamanca, Castilla y Leon, Spain, 3Hospital Universitario Salamanca, Salamanca, Spain
Background/Purpose: Ocular inflammatory involvement for being closely related to systemic autoimmune diseases is monitored and treated in our rheumatology visits. The most frequently studied by rheumatologists are acute anterior uveitis, usually unilateral, which are frequently associated with spondyloarthritis.
However, there are other clinical situations of ocular inflammation, which, although less frequent, are important to know due to the need for a systemic differential diagnosis.
The aim is to describe the clinical characteristics of a group of patients with ocular inflammatory pathology other than anterior uveitis seen in a rheumatology department during the last year.
Methods: A longitudinal, retrospective, descriptive and observational study was conducted. The clinical characteristics and treatment of patients with uveitis not cataloged with anterior pole involvement (intermediate uveitis and panuveitis), as well as ocular vasculitis such as Eales disease were collected. A total of 15 patients seen in the rheumatology department during the last year were included. Both demographic (sex, age…) and clinical characteristics (type of ocular involvement, laterality, number of episodes, treatment and duration of treatment) have been reported.
Results: The mean age of the collected patients was 46.5 years with a predominance of women (60%). The findings in the ophthalmologic examination were panuveitis in 73% of the patients, of which after the performance of various complementary tests, the diagnosis of Vogt-Koyanagi-Harada syndrome (Figure 1) was reached in 4 of these patients, Behcet's syndrome in 3 patients and without being able to identify the origin in 4 of them. Of the remaining 4 patients, 2 of them were diagnosed with intermediate uveitis of unknown cause, and the remaining 2 patients had findings of retinal vasculitis in relation to Eales disease.
Regarding the monocular or binocular involvement of the ophthalmologic manifestations, 47% of the cases had unilateral clinical manifestations. Most of them 12/15 (80%) required immunosuppressive treatment to control the disease, with 80% of the patients presenting less than three flares of activity, which were controlled after the start of treatment. Currently, 2 (13,3%) patients are untreated due to the control of ocular activity. The most commonly used treatments are listed in Table 1.
Conclusion: Although these entities are much less frequent, it is important to be aware of their existence and management, since on several occasions ophthalmologist require our assessment in rheumatology, hence the importance of an adequate differential diagnosis.
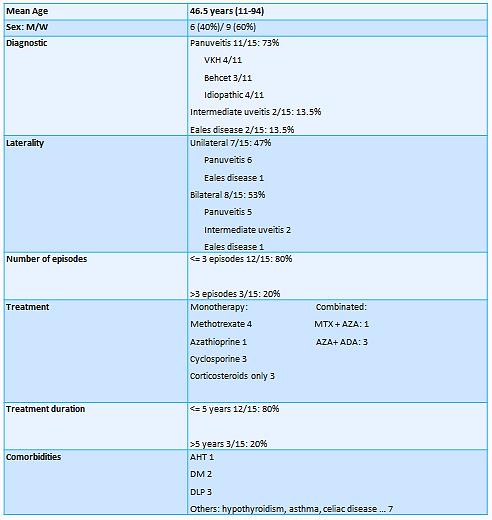 Table 1: Demographic and clinical characteristics of patients.
Table 1: Demographic and clinical characteristics of patients.
.jpg) Figure 1: Eye fundus of patient 11 diagnosed with Vogt-Koyanagi-Harada. On the left, a bud with tortuosity of the vessels and multiple neurosensory detachments is observed. On the right eye fundus after resolution of the flare, without papilledema and with vessels of normal caliber.
Figure 1: Eye fundus of patient 11 diagnosed with Vogt-Koyanagi-Harada. On the left, a bud with tortuosity of the vessels and multiple neurosensory detachments is observed. On the right eye fundus after resolution of the flare, without papilledema and with vessels of normal caliber.
Disclosures: S. Pastor Navarro, None; O. Compán Fernández, None; M. Ibáñez Martínez, None; B. Miguel Ibáñez, None; M. Molina Pérez, None; Á. Beltrán Mazo, None; O. Martínez González, None; C. Montilla Morales, None; A. Turrión Nieves, None; S. Gómez Castro, None; C. Hidalgo Calleja, None.
Background/Purpose: Ocular inflammatory involvement for being closely related to systemic autoimmune diseases is monitored and treated in our rheumatology visits. The most frequently studied by rheumatologists are acute anterior uveitis, usually unilateral, which are frequently associated with spondyloarthritis.
However, there are other clinical situations of ocular inflammation, which, although less frequent, are important to know due to the need for a systemic differential diagnosis.
The aim is to describe the clinical characteristics of a group of patients with ocular inflammatory pathology other than anterior uveitis seen in a rheumatology department during the last year.
Methods: A longitudinal, retrospective, descriptive and observational study was conducted. The clinical characteristics and treatment of patients with uveitis not cataloged with anterior pole involvement (intermediate uveitis and panuveitis), as well as ocular vasculitis such as Eales disease were collected. A total of 15 patients seen in the rheumatology department during the last year were included. Both demographic (sex, age…) and clinical characteristics (type of ocular involvement, laterality, number of episodes, treatment and duration of treatment) have been reported.
Results: The mean age of the collected patients was 46.5 years with a predominance of women (60%). The findings in the ophthalmologic examination were panuveitis in 73% of the patients, of which after the performance of various complementary tests, the diagnosis of Vogt-Koyanagi-Harada syndrome (Figure 1) was reached in 4 of these patients, Behcet's syndrome in 3 patients and without being able to identify the origin in 4 of them. Of the remaining 4 patients, 2 of them were diagnosed with intermediate uveitis of unknown cause, and the remaining 2 patients had findings of retinal vasculitis in relation to Eales disease.
Regarding the monocular or binocular involvement of the ophthalmologic manifestations, 47% of the cases had unilateral clinical manifestations. Most of them 12/15 (80%) required immunosuppressive treatment to control the disease, with 80% of the patients presenting less than three flares of activity, which were controlled after the start of treatment. Currently, 2 (13,3%) patients are untreated due to the control of ocular activity. The most commonly used treatments are listed in Table 1.
Conclusion: Although these entities are much less frequent, it is important to be aware of their existence and management, since on several occasions ophthalmologist require our assessment in rheumatology, hence the importance of an adequate differential diagnosis.
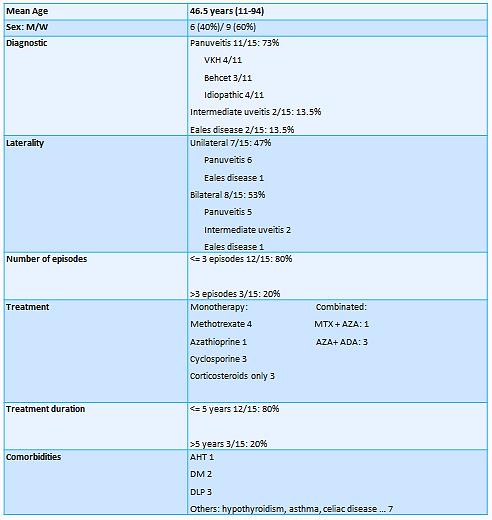 Table 1: Demographic and clinical characteristics of patients.
Table 1: Demographic and clinical characteristics of patients..jpg) Figure 1: Eye fundus of patient 11 diagnosed with Vogt-Koyanagi-Harada. On the left, a bud with tortuosity of the vessels and multiple neurosensory detachments is observed. On the right eye fundus after resolution of the flare, without papilledema and with vessels of normal caliber.
Figure 1: Eye fundus of patient 11 diagnosed with Vogt-Koyanagi-Harada. On the left, a bud with tortuosity of the vessels and multiple neurosensory detachments is observed. On the right eye fundus after resolution of the flare, without papilledema and with vessels of normal caliber.Disclosures: S. Pastor Navarro, None; O. Compán Fernández, None; M. Ibáñez Martínez, None; B. Miguel Ibáñez, None; M. Molina Pérez, None; Á. Beltrán Mazo, None; O. Martínez González, None; C. Montilla Morales, None; A. Turrión Nieves, None; S. Gómez Castro, None; C. Hidalgo Calleja, None.

