Back
Poster Session B
Systemic lupus erythematosus (SLE)
Session: (0974–1003) SLE – Treatment Poster II
0977: Effect of Belimumab (BEL) on B-cells and Serological Biomarkers for SLE: Results of the Large Integrated Analysis BEL Summary of Lupus Efficacy (Be-SLE)
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
.png)
Jason Knight, MD, PhD
University of Michigan
Ann Arbor, MI, United States
Abstract Poster Presenter(s)
Jason S Knight1, Winn Walter Chatham2, Christine Henning3, Julia H N Harris4, Andre Van Maurik5, Roger A Levy6 and David Pisetsky7, 1University of Michigan, Division of Rheumatology, Ann Arbor, MI, 2University of Alabama at Birmingham, Clinical Immunology and Rheumatology, Birmingham, AL, 3GlaxoSmithKline, Global Medical Affairs, Durham, NC, 4GlaxoSmithKline, Immunology Biostatistics, Brentford, United Kingdom, 5GlaxoSmithKline, Clinical Pharmacology and Experimental Medicine, Stevenage, United Kingdom, 6GlaxoSmithKline, Global Medical Affairs, Collegeville, PA, 7Duke University Medical Center, Durham, NC
Background/Purpose: Serological and cellular biomarkers are used in clinical practice to guide the management of SLE. Increased levels of anti-dsDNA and decreased levels of complement are often associated with active disease, and predictive of disease flares and progression.1,2 The monoclonal antibody BEL (approved for SLE and LN) inhibits B-lymphocyte stimulator and has been shown to improve biomarkers in individual studies.3 This analysis used pooled data from five studies to evaluate the effects of BEL on B-cells and various serological biomarkers (Igs, autoantibodies, complement) in a large population of adult patients (pts) with SLE.
Methods: The Be-SLE integrated, post hoc analysis assessed data from five double-blind, placebo (PBO)-controlled BEL studies: BLISS-76, BLISS-52, BLISS-NEA, BLISS-SC, and EMBRACE. In all studies, pts with active SLE received BEL (10 mg/kg intravenously or 200 mg subcutaneously) or PBO, plus standard therapy. Median percent changes (interquartile range [IQR]) from baseline over 52 weeks (Wks) were reported for B-cells, Igs, autoantibodies and complement. Wilcoxon rank sum tests (for Igs and autoantibodies) and analysis of covariance (for B-cells and complement) were used to determine statistical differences between BEL- and PBO-treated groups.
Results: In total, 1869 and 1217 pts received BEL and PBO, respectively. Most were female (BEL, 95%; PBO, 94%) and of Asian, White, or Black African ancestry (BEL, 37%, 32%, and 22%; PBO, 33%, 36%, and 19%, respectively), with a mean (SD) age of 36.7 (11.4) and 37.4 (12.0) among BEL- and PBO-treated pts. Levels of B-cells, Igs, autoantibodies, and complement generally showed larger median (IQR) percent changes among pts receiving BEL versus PBO (Table). For example, CD19+ total B-cells (BEL, -55.8% [-73.9, -25.6]; PBO, -10.1% [-39.7, 29.1]), naïve CD20+ CD27- B-cells (BEL, -70.0% [-83.1, -49.2]; PBO -10.4% [-38.7, 31.7]) and IgM (BEL, -29.5% [-40.2, -18.8]; PBO, -3.2% [-15.4, 9.9]) had significantly greater reductions with BEL than PBO at Wk 52 (all p< 0.0001). Levels of anti-dsDNA (BEL, -30.0% [-61.8, 0.0]; PBO, 0.0% [-37.5, 0.0]), anti-Sm (BEL, -49.5% [-66.7, -22.2]; PBO, -29.9% [-49.3, -4.2]) and anti-RNP (BEL, -55.0% [-71.0, -26.2]; PBO, -24.6% [-47.2, 0.0]) had significantly greater reductions with BEL versus PBO at Wk 52 (all p< 0.0001). Pts receiving BEL also showed a significant increase in levels of complement versus PBO (Table). Changes in B-cells and these serological biomarkers were observed as early as Wk 8 (data not shown).
Conclusion: BEL treatment showed significant improvements in serological biomarkers (including reductions in autoantibodies and increased complement) and B-cell populations versus PBO. Improvements in autoantibodies were observed by Wk 8 and continued to improve over 52 weeks. By combining multiple studies, this analysis provides insights using a larger dataset than would otherwise be available and confirms the benefits of BEL on biomarkers in a large, pooled population.
Funding: GSK
References
1Capecchi R, et al. Rheumatology (Oxford). 2020;59:v12–v18
2Bertsias G, et al. EULAR Textbook on Rheumatic Diseases. 2012;5:476–505
3Levy RA, et al. Lupus. 2021;30:1705–21
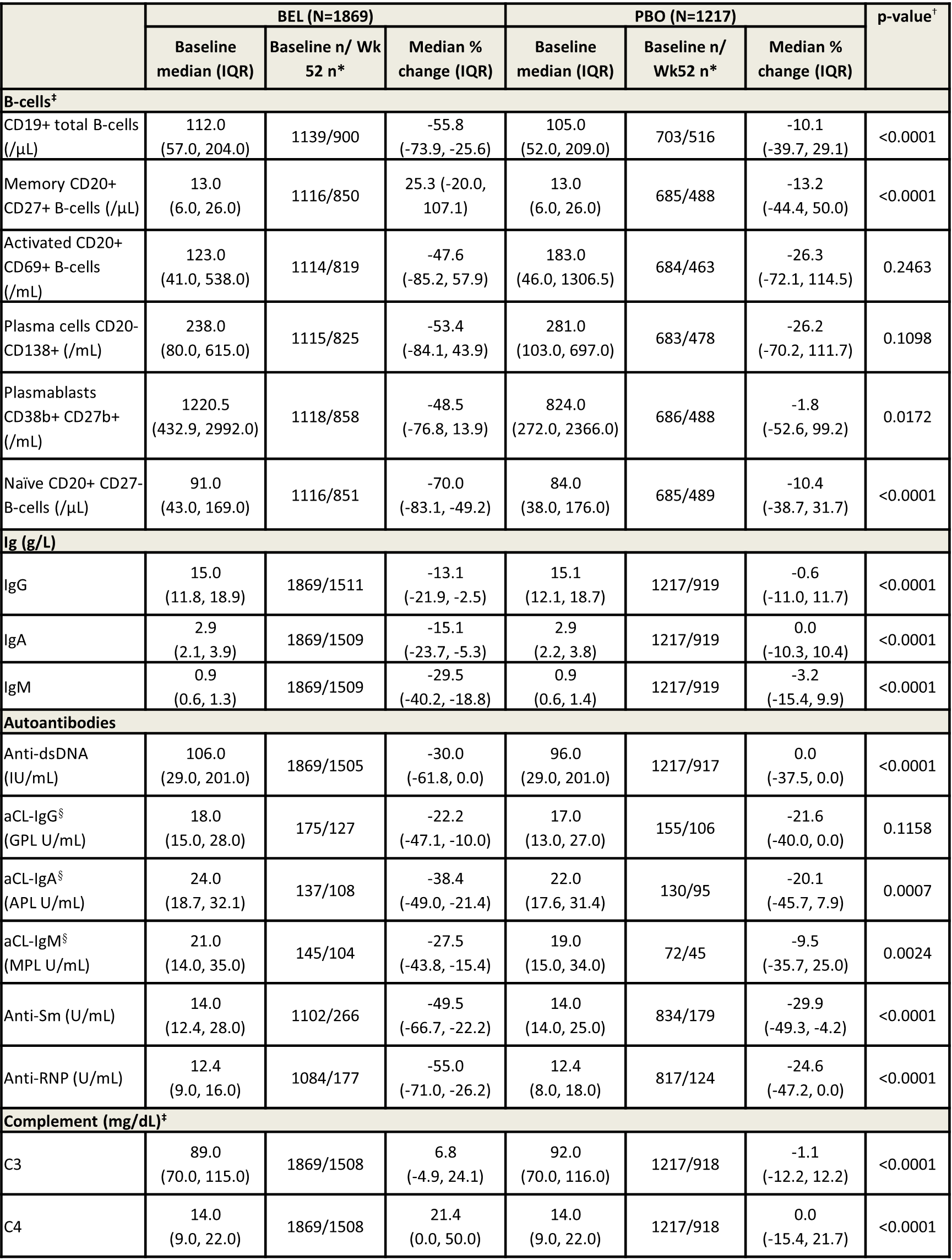 Table. B-cell and serological biomarker levels, median percent change from baseline at Wk 52 (mITT population).
Table. B-cell and serological biomarker levels, median percent change from baseline at Wk 52 (mITT population).
*Patients with a baseline value of zero were excluded from analysis at Wk 52; †a p-value of < 0.05 was considered significant; ‡covariates for the ANCOVA were treatment group, study, baseline B-cell value or baseline complement value, and baseline SELENA-SLEDAI score; §among patients who were positive at baseline.
ANCOVA, analysis of covariance; mITT, modified intent-to-treat; SELENA, Safety of Estrogens in Systemic Lupus Erythematosus National Assessment
Disclosures: J. Knight, Jazz Pharmaceuticals, Bristol Myers Squibb; W. Chatham, GlaxoSmithKline; C. Henning, GlaxoSmithKline; J. Harris, GlaxoSmithKline; A. Van Maurik, GlaxoSmithKline, GlaxoSmithKlein(GSK); R. Levy, GlaxoSmithKline (GSK); D. Pisetsky, DILI-Sym Immunovant BMS, Exagen, Immunovant.
Background/Purpose: Serological and cellular biomarkers are used in clinical practice to guide the management of SLE. Increased levels of anti-dsDNA and decreased levels of complement are often associated with active disease, and predictive of disease flares and progression.1,2 The monoclonal antibody BEL (approved for SLE and LN) inhibits B-lymphocyte stimulator and has been shown to improve biomarkers in individual studies.3 This analysis used pooled data from five studies to evaluate the effects of BEL on B-cells and various serological biomarkers (Igs, autoantibodies, complement) in a large population of adult patients (pts) with SLE.
Methods: The Be-SLE integrated, post hoc analysis assessed data from five double-blind, placebo (PBO)-controlled BEL studies: BLISS-76, BLISS-52, BLISS-NEA, BLISS-SC, and EMBRACE. In all studies, pts with active SLE received BEL (10 mg/kg intravenously or 200 mg subcutaneously) or PBO, plus standard therapy. Median percent changes (interquartile range [IQR]) from baseline over 52 weeks (Wks) were reported for B-cells, Igs, autoantibodies and complement. Wilcoxon rank sum tests (for Igs and autoantibodies) and analysis of covariance (for B-cells and complement) were used to determine statistical differences between BEL- and PBO-treated groups.
Results: In total, 1869 and 1217 pts received BEL and PBO, respectively. Most were female (BEL, 95%; PBO, 94%) and of Asian, White, or Black African ancestry (BEL, 37%, 32%, and 22%; PBO, 33%, 36%, and 19%, respectively), with a mean (SD) age of 36.7 (11.4) and 37.4 (12.0) among BEL- and PBO-treated pts. Levels of B-cells, Igs, autoantibodies, and complement generally showed larger median (IQR) percent changes among pts receiving BEL versus PBO (Table). For example, CD19+ total B-cells (BEL, -55.8% [-73.9, -25.6]; PBO, -10.1% [-39.7, 29.1]), naïve CD20+ CD27- B-cells (BEL, -70.0% [-83.1, -49.2]; PBO -10.4% [-38.7, 31.7]) and IgM (BEL, -29.5% [-40.2, -18.8]; PBO, -3.2% [-15.4, 9.9]) had significantly greater reductions with BEL than PBO at Wk 52 (all p< 0.0001). Levels of anti-dsDNA (BEL, -30.0% [-61.8, 0.0]; PBO, 0.0% [-37.5, 0.0]), anti-Sm (BEL, -49.5% [-66.7, -22.2]; PBO, -29.9% [-49.3, -4.2]) and anti-RNP (BEL, -55.0% [-71.0, -26.2]; PBO, -24.6% [-47.2, 0.0]) had significantly greater reductions with BEL versus PBO at Wk 52 (all p< 0.0001). Pts receiving BEL also showed a significant increase in levels of complement versus PBO (Table). Changes in B-cells and these serological biomarkers were observed as early as Wk 8 (data not shown).
Conclusion: BEL treatment showed significant improvements in serological biomarkers (including reductions in autoantibodies and increased complement) and B-cell populations versus PBO. Improvements in autoantibodies were observed by Wk 8 and continued to improve over 52 weeks. By combining multiple studies, this analysis provides insights using a larger dataset than would otherwise be available and confirms the benefits of BEL on biomarkers in a large, pooled population.
Funding: GSK
References
1Capecchi R, et al. Rheumatology (Oxford). 2020;59:v12–v18
2Bertsias G, et al. EULAR Textbook on Rheumatic Diseases. 2012;5:476–505
3Levy RA, et al. Lupus. 2021;30:1705–21
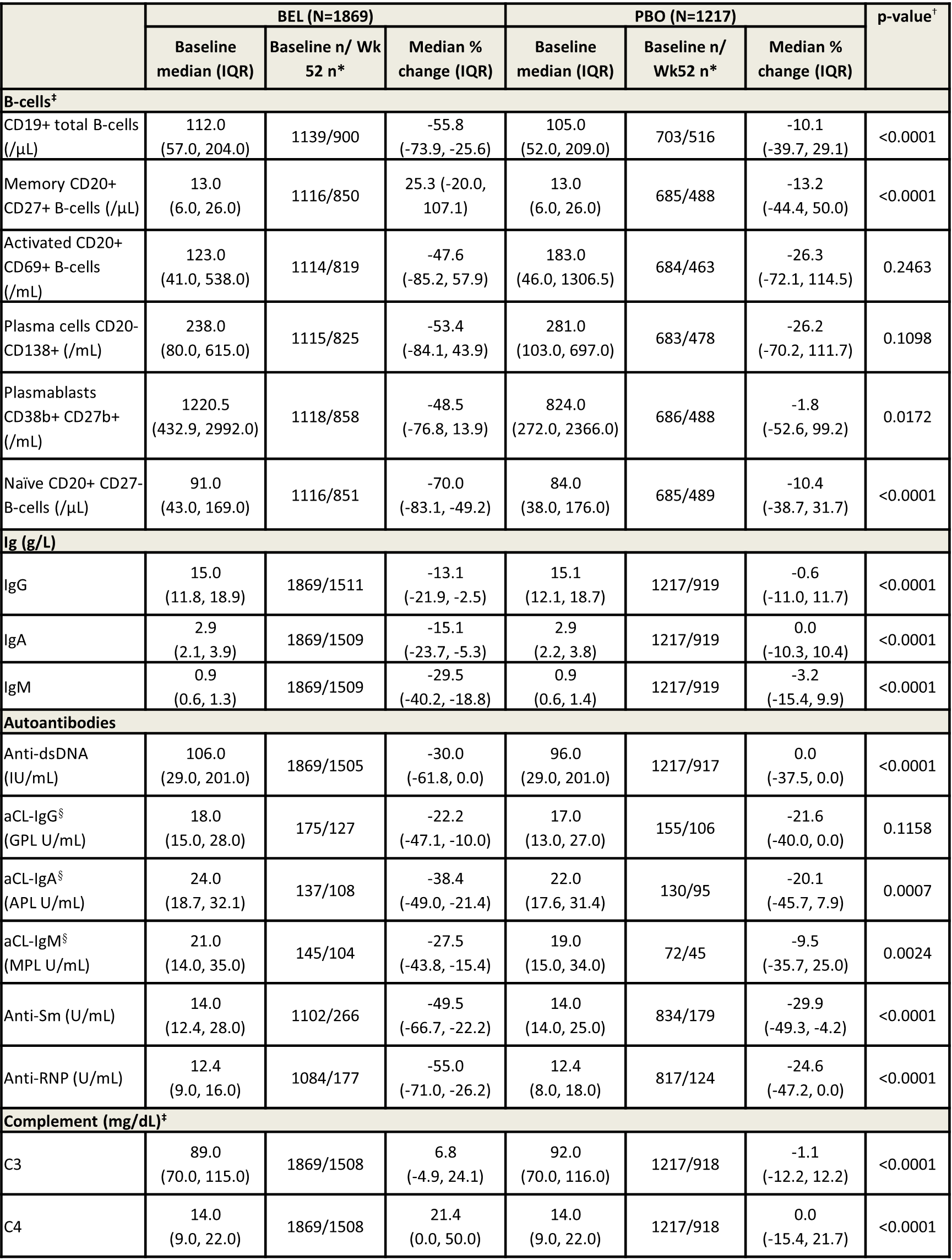 Table. B-cell and serological biomarker levels, median percent change from baseline at Wk 52 (mITT population).
Table. B-cell and serological biomarker levels, median percent change from baseline at Wk 52 (mITT population). *Patients with a baseline value of zero were excluded from analysis at Wk 52; †a p-value of < 0.05 was considered significant; ‡covariates for the ANCOVA were treatment group, study, baseline B-cell value or baseline complement value, and baseline SELENA-SLEDAI score; §among patients who were positive at baseline.
ANCOVA, analysis of covariance; mITT, modified intent-to-treat; SELENA, Safety of Estrogens in Systemic Lupus Erythematosus National Assessment
Disclosures: J. Knight, Jazz Pharmaceuticals, Bristol Myers Squibb; W. Chatham, GlaxoSmithKline; C. Henning, GlaxoSmithKline; J. Harris, GlaxoSmithKline; A. Van Maurik, GlaxoSmithKline, GlaxoSmithKlein(GSK); R. Levy, GlaxoSmithKline (GSK); D. Pisetsky, DILI-Sym Immunovant BMS, Exagen, Immunovant.

