Back
Poster Session D
Sjögren's syndrome
Session: (2017–2051) Sjögren's Syndrome – Basic and Clinical Science Poster
2034: What Is the Best Initial Screening for Suspected Sjögren's Disease?
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- AH
Alojzija Hocevar, MD
University Medical Center Ljubljana
LJUBLJANA, Slovenia
Abstract Poster Presenter(s)
Katja Perdan Pirkmajer, Jelka Kramarič, matija Tomšič and Alojzija Hocevar, University Medical Centre Ljubljana, Ljubljana, Slovenia
Background/Purpose: During the COVID-19 pandemic the routine diagnostic procedure in Sjögren's disease (SS) was highly hampered.
The aim of our study was to determine in a cohort of well-defined sicca patients the best screening tool for SS, obviating, when possible, the initial exposure to potentially infectious body fluids (eg. saliva, tears) and/or invasive procedures (lip biopsy) We also evaluated the performance of the newly proposed 5-item Sjögren's Syndrome Screening Questionnaire (SSSQ) derived from SICCA study data, that was shown to better differentiate SS from non-SS sicca patients compared to conventional sicca questionnaire1.
Methods: Our cohort consisted of 282 subjects (109 SS and 173 non-SS sicca patients) who completed a standardized diagnostic procedure for SS based on the ACR/EULAR 2016 classification criteria2 (standard sicca questions, Schirmer test, Rose Bengal test, unstimulated salivary flow test, immunoserological tests (anti-SSA) and lip biopsy) between Jan/2016 to Dec/2018. In addition, major salivary gland ultrasound (SGUS) was performed in each subject at the time of diagnostic procedure3. Afterwards all subjects were contacted by phone to fulfil the new SSSQ. Descriptive statistics and ROC curve analysis, calculating area under the curve (AUC) were used to analyse data.
Results: The results of standard sicca questions, SSSQ, Schirmer test, Rose Bengal test, unstimulated salivary flow test, SGUS, anti-SSA and lip biopsy were positive in 90.4%, 34.0%, 50.4%, 30.1%, 63.8%, 19.1%, 27.7% and 33.3%, respectively. The Table 1 shows the distribution of positive tests according to final diagnosis (SS vs. non-SS). The new SSSQ had a sensitivity of 41.3% and a specificity of 70.5% for SS (in comparison, the traditional sicca questions were 85.3% sensitive but only 6.4% specific for SS). Table 2 and Figure 1 show the performance of combinations of various tests that were easily available in the daily clinical practice for supporting SS diagnosis.
Conclusion: Our data suggest, that screening with a combination of anti-SSA and SGUS provides the highest AUC and specificity for SS, while a combination of SSSQ, anti-SSA and Schirmer tear test yielded the best sensitivity among the compared combinations.
References: Yu K, et al. J Clin Rheumatol 2021; doi: 10.1097/RHU.0000000000001760b
Shiboski CH, et al. Arthritis Rheumatol 2017;69:35–45. 10.1002/art.39859
H. Hocevar A, et al. Rheumatology 2005; 10.1093/rheumatology/keh588
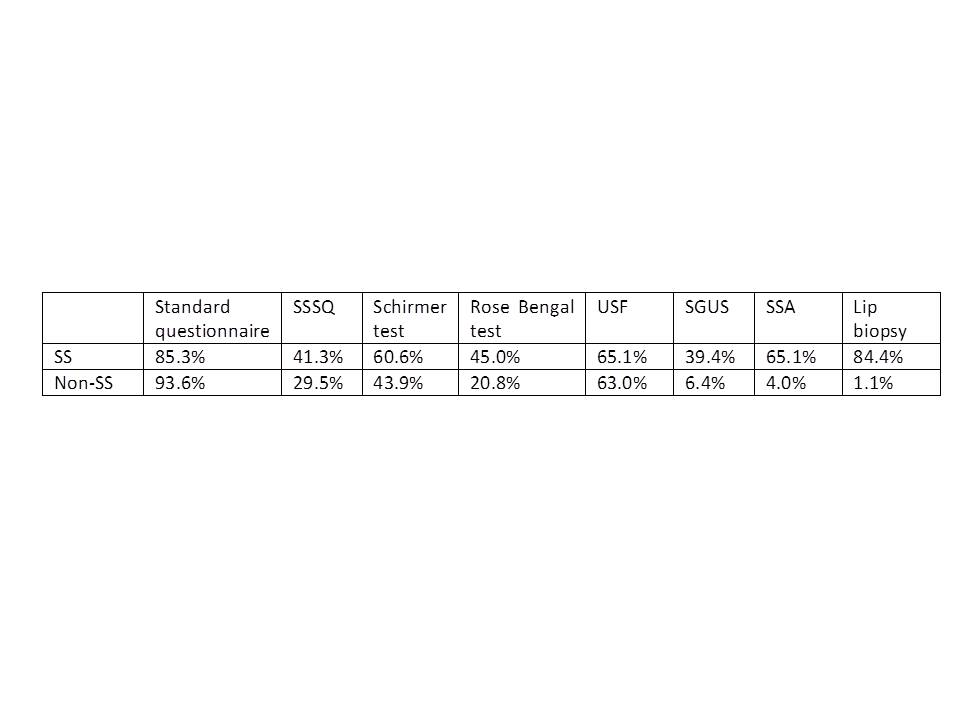 Table 1. Distribution of positive tests based on final diagnosis
Table 1. Distribution of positive tests based on final diagnosis
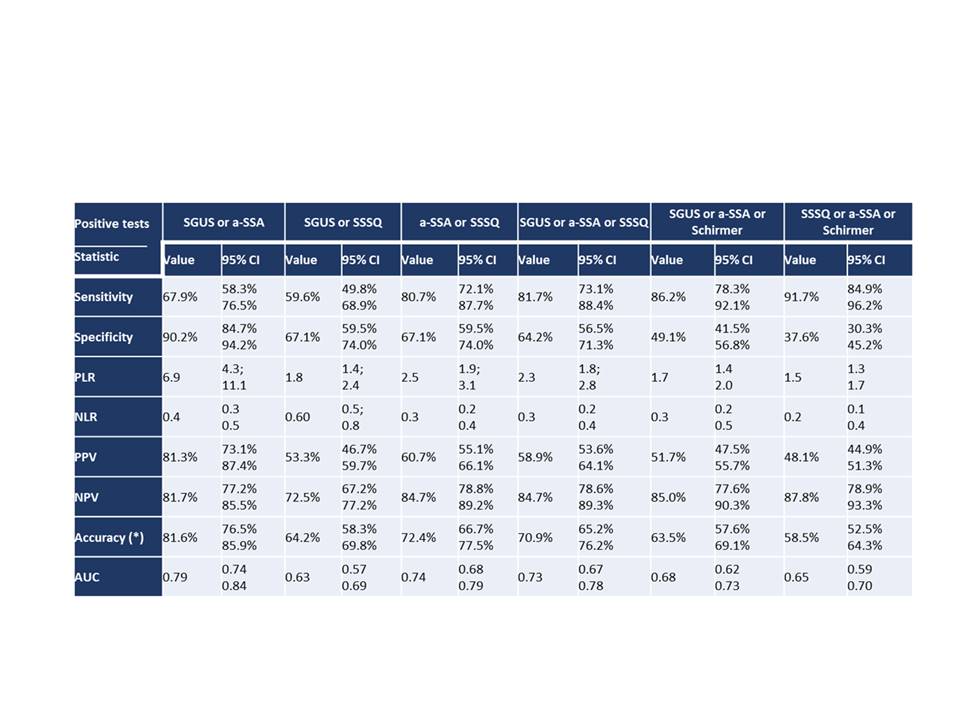 Table 2. The performance of different combinations tests in SS screening.
Table 2. The performance of different combinations tests in SS screening.
Legend: PLR Positive Likelihood Ratio; NLR Negative Likelihood Ratio; PPV Positive Predictive Value ; NPV Positive Predictive Value; AUC area under the ROC curve;
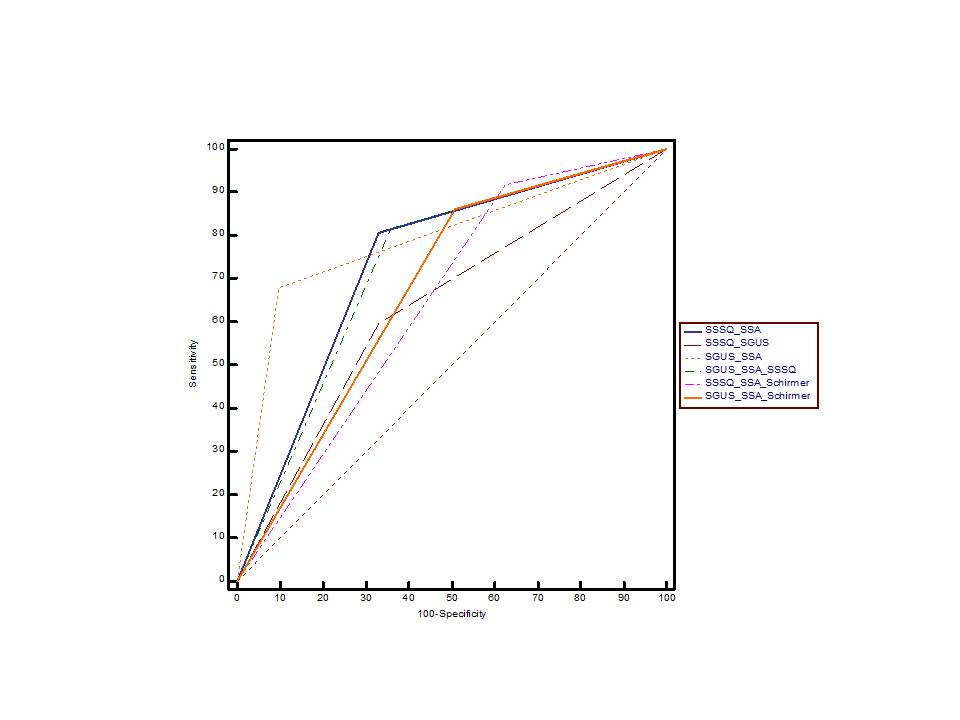 Figure 1. ROC curve analysis of different test combinations for diagnosing SS.
Figure 1. ROC curve analysis of different test combinations for diagnosing SS.
Disclosures: K. Perdan Pirkmajer, None; J. Kramarič, None; m. Tomšič, None; A. Hocevar, None.
Background/Purpose: During the COVID-19 pandemic the routine diagnostic procedure in Sjögren's disease (SS) was highly hampered.
The aim of our study was to determine in a cohort of well-defined sicca patients the best screening tool for SS, obviating, when possible, the initial exposure to potentially infectious body fluids (eg. saliva, tears) and/or invasive procedures (lip biopsy) We also evaluated the performance of the newly proposed 5-item Sjögren's Syndrome Screening Questionnaire (SSSQ) derived from SICCA study data, that was shown to better differentiate SS from non-SS sicca patients compared to conventional sicca questionnaire1.
Methods: Our cohort consisted of 282 subjects (109 SS and 173 non-SS sicca patients) who completed a standardized diagnostic procedure for SS based on the ACR/EULAR 2016 classification criteria2 (standard sicca questions, Schirmer test, Rose Bengal test, unstimulated salivary flow test, immunoserological tests (anti-SSA) and lip biopsy) between Jan/2016 to Dec/2018. In addition, major salivary gland ultrasound (SGUS) was performed in each subject at the time of diagnostic procedure3. Afterwards all subjects were contacted by phone to fulfil the new SSSQ. Descriptive statistics and ROC curve analysis, calculating area under the curve (AUC) were used to analyse data.
Results: The results of standard sicca questions, SSSQ, Schirmer test, Rose Bengal test, unstimulated salivary flow test, SGUS, anti-SSA and lip biopsy were positive in 90.4%, 34.0%, 50.4%, 30.1%, 63.8%, 19.1%, 27.7% and 33.3%, respectively. The Table 1 shows the distribution of positive tests according to final diagnosis (SS vs. non-SS). The new SSSQ had a sensitivity of 41.3% and a specificity of 70.5% for SS (in comparison, the traditional sicca questions were 85.3% sensitive but only 6.4% specific for SS). Table 2 and Figure 1 show the performance of combinations of various tests that were easily available in the daily clinical practice for supporting SS diagnosis.
Conclusion: Our data suggest, that screening with a combination of anti-SSA and SGUS provides the highest AUC and specificity for SS, while a combination of SSSQ, anti-SSA and Schirmer tear test yielded the best sensitivity among the compared combinations.
References: Yu K, et al. J Clin Rheumatol 2021; doi: 10.1097/RHU.0000000000001760b
Shiboski CH, et al. Arthritis Rheumatol 2017;69:35–45. 10.1002/art.39859
H. Hocevar A, et al. Rheumatology 2005; 10.1093/rheumatology/keh588
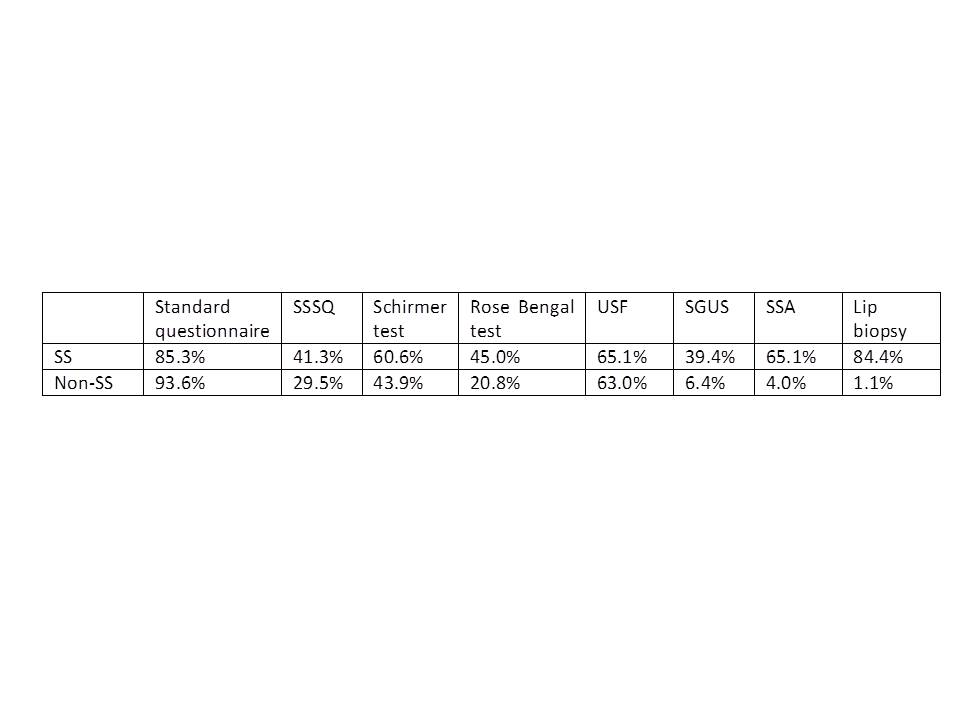 Table 1. Distribution of positive tests based on final diagnosis
Table 1. Distribution of positive tests based on final diagnosis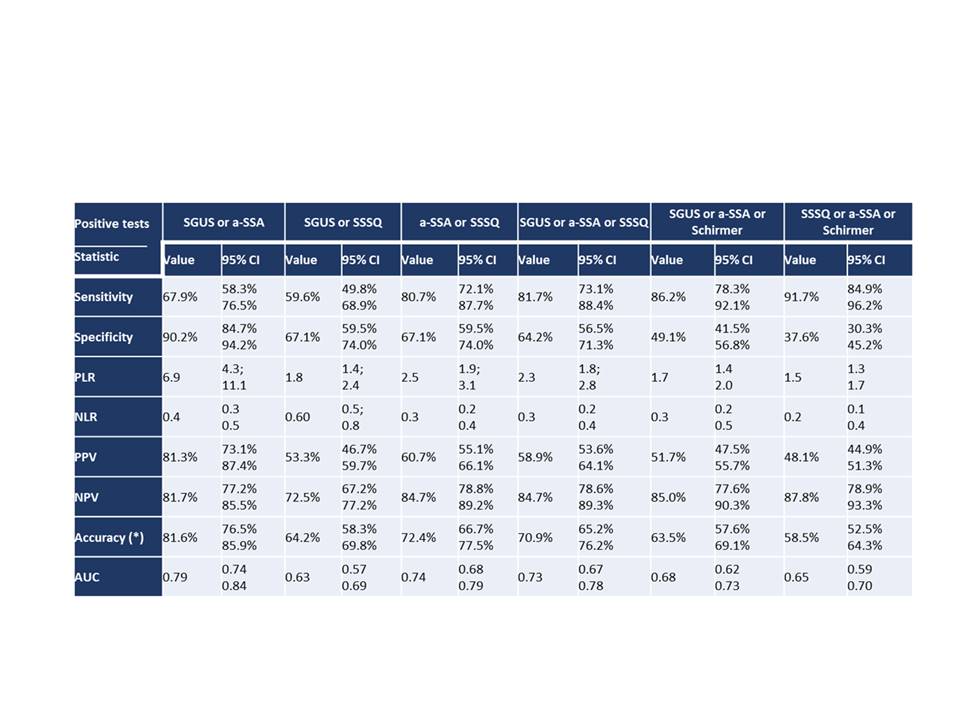 Table 2. The performance of different combinations tests in SS screening.
Table 2. The performance of different combinations tests in SS screening.Legend: PLR Positive Likelihood Ratio; NLR Negative Likelihood Ratio; PPV Positive Predictive Value ; NPV Positive Predictive Value; AUC area under the ROC curve;
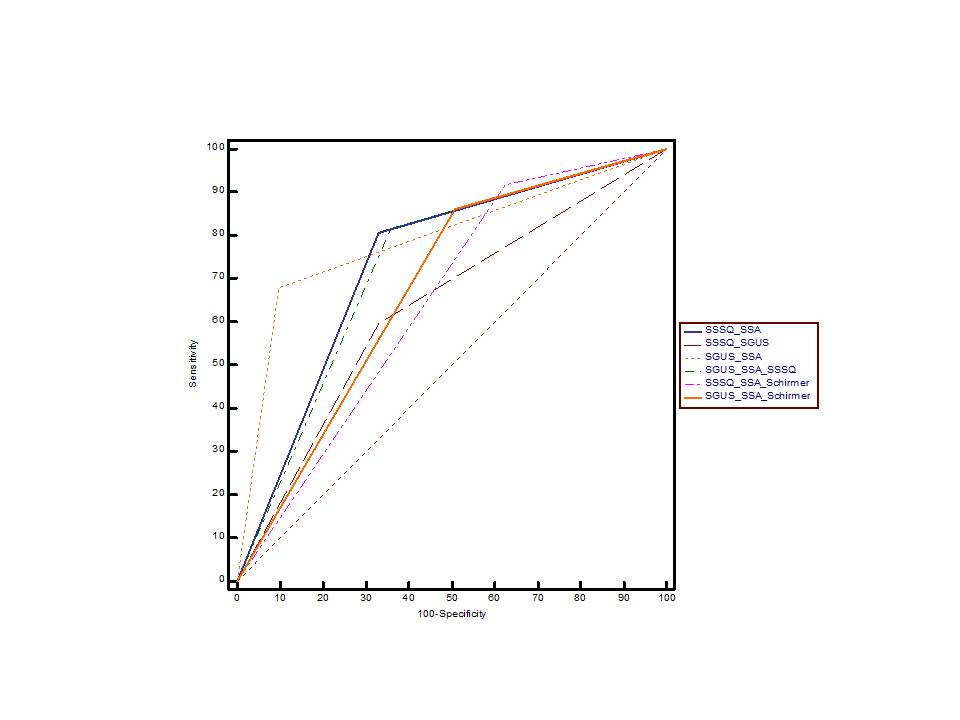 Figure 1. ROC curve analysis of different test combinations for diagnosing SS.
Figure 1. ROC curve analysis of different test combinations for diagnosing SS.Disclosures: K. Perdan Pirkmajer, None; J. Kramarič, None; m. Tomšič, None; A. Hocevar, None.

