Back
Poster Session B
Rheumatoid arthritis (RA)
Session: (0913–0938) RA – Treatment Poster II
0934: Impact of Tapering Targeted Therapy on Disease Activity Is Different Based on Concomitant Methotrexate Use in Patients with Rheumatoid Arthritis: A Nationwide Cohort Study
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- JP
Jun Won Park, MD
Seoul National University Hospital
Seoul, South Korea
Abstract Poster Presenter(s)
Jun Won Park1, Min Jung Kim2, Hyoun-Ah Kim3, Jinhyun Kim4, Eun Bong Lee1 and Kichul Shin5, 1Seoul National University Hospital, Seoul, Republic of Korea, 2Seoul Metropolitan Government Boramae Medical center, Dongjak-gu, Seoul, Republic of Korea, 3Ajou University School of Medicine, Suwon, Republic of Korea, 4Chungnam National University Hospital, Jung-gu, Daejeon, South Korea, 5Seoul Metropolitan Government- Seoul National University Boramae Medical Center, Seoul, Republic of Korea
Background/Purpose: The American College of Rheumatology and the European League Against Rheumatism recommend using methotrexate (MTX) with targeted therapy. Previous studies have shown that tapering targeted therapy (including biologic DMARDs and targeted synthetic DMARDs) is feasible for selected patients with rheumatoid arthritis (RA), yet there has been no consensus of the detailed strategy. Moreover, the impact of MTX on disease activity during tapering targeted therapy is still inconclusive. We aimed to investigate the interaction between the effect of tapering targeted therapy and concurrent MTX use on disease activity in patients with RA in real-world clinical practice.
Methods: This study used data from the Korean College of Rheumatology Biologics and Targeted therapy Registry (KOBIO-RA), a nationwide cohort of patients with RA receiving targeted therapy in outpatient clinics (NCT01965132). Patients were enrolled when they initiated a new targeted therapy and were followed-up annually thereafter. This study included 1-year follow-up intervals from patients treated with concomitant MTX treatment (defined as ≥ 7.5mg/week of MTX with targeted therapy) at baseline visit. As the decision on tapering is influenced by time-varying factors such as disease activity measured at the follow-up interval of last year, we used the marginal structural model in which inverse probability of treatment weights (IPTWs) for each interval was applied to control time-varying confounders. The primary outcome in this study was clinical remission based on DAS28-ESR in each follow-up interval. The effect of tapering targeted therapy, concomitant MTX treatment, and their interactions with the outcome were estimated using generalized estimating equation.
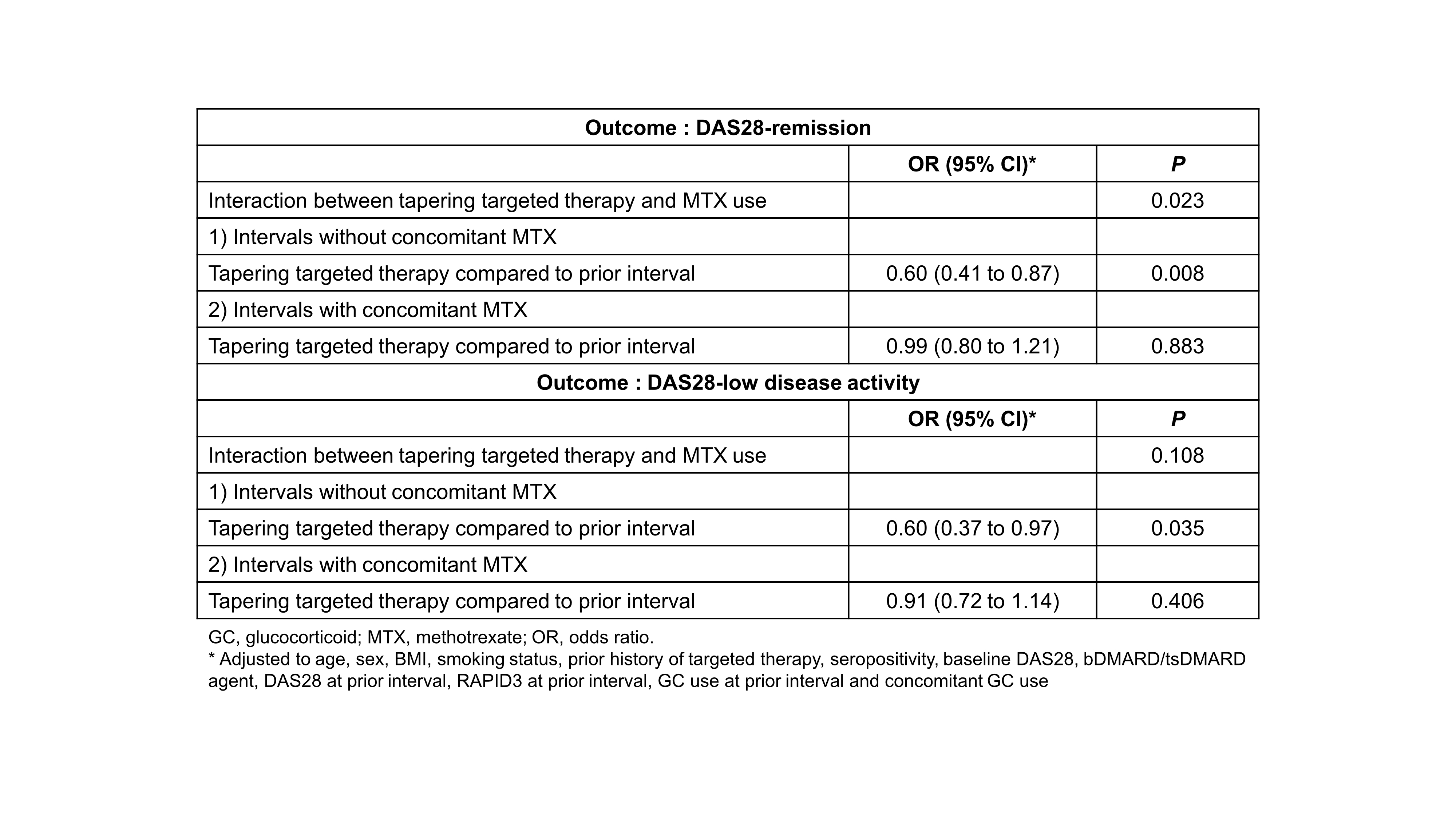
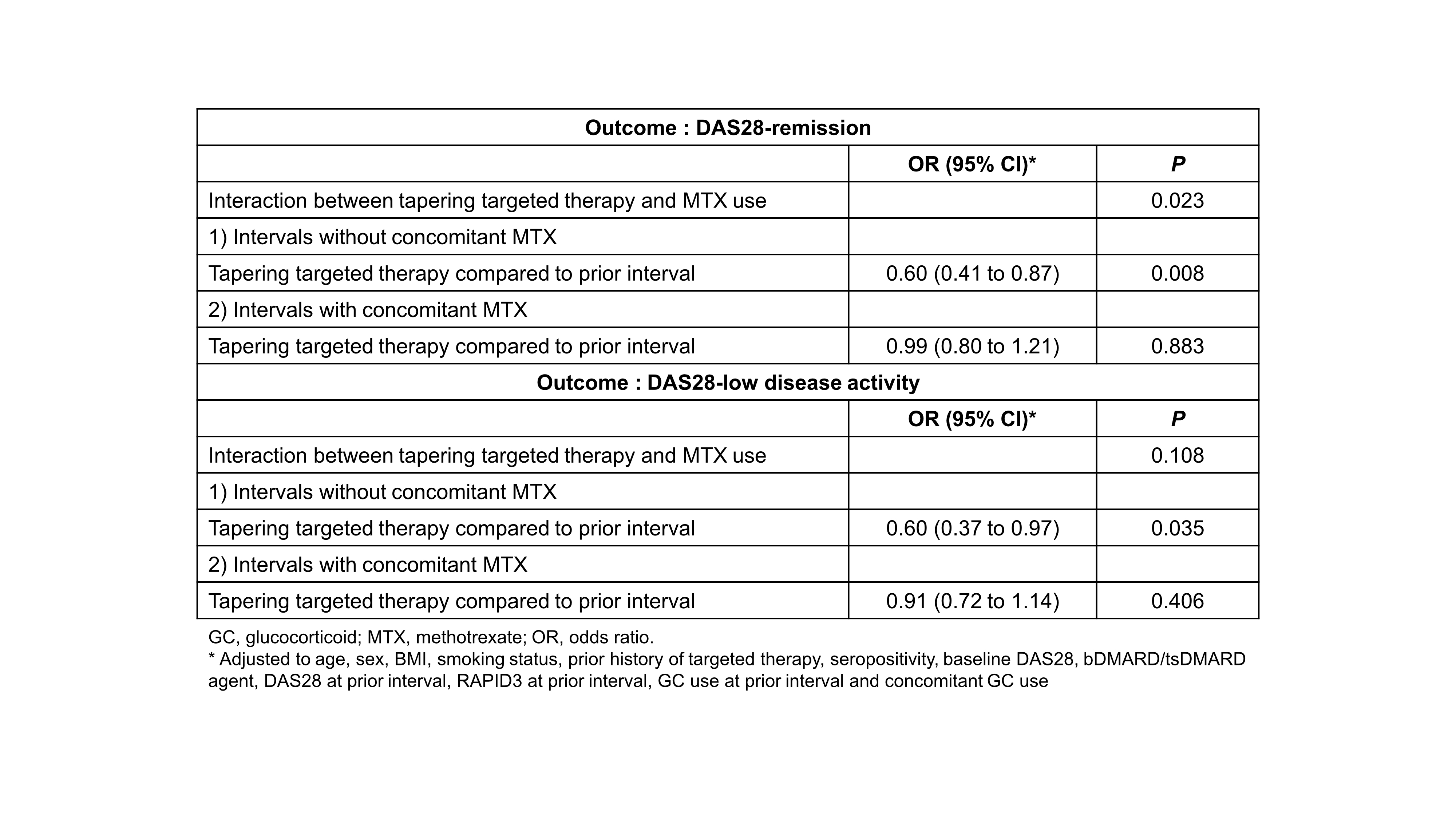
Results: A total of 3816 follow-up intervals from 1487 patients were analyzed. Tapering targeted therapy compared with previous follow-ups occurred in 816 intervals (tapering group vs. non-tapering group). Baseline clinical factors such as disease activity, dose of MTX, and concomitant glucocorticoid use were also comparable but mean (SD) DAS28-ESR (3.89 [1.8] vs. 3.3 [1.7], P < 0.001) and proportion of patients with glucocorticoid (71.2% vs. 65.4%, P = 0.002) in the previous interval was significantly lower in the tapering group. These time-varying factors were all balanced after IPTWs were applied (Table 1). The effect of tapering targeted therapy was significantly different based on whether a patients received concomitant MTX. In the subgroup of intervals with concomitant MTX, tapering targeted therapy did not affect the likelihood of achieving DAS28-remission (adjusted OR 0.99 [95% CI 0.80-1.21]). However, without concomitant MTX treatment, tapering targeted therapy was significantly associated with a lower likelihood of DAS28-remission (0.60 [0.41-0.87]) (P-value for interaction = 0.023). The result was comparable when the outcome was DAS28-low disease activity (LDA) (Table 2).
Conclusion: Tapering targeted therapy without concomitant MTX would likely result in failure to reach DAS28 remission or LDA in patients with RA.
.jpg)
Disclosures: J. Park, None; M. Kim, None; H. Kim, None; J. Kim, None; E. Lee, None; K. Shin, None.
Background/Purpose: The American College of Rheumatology and the European League Against Rheumatism recommend using methotrexate (MTX) with targeted therapy. Previous studies have shown that tapering targeted therapy (including biologic DMARDs and targeted synthetic DMARDs) is feasible for selected patients with rheumatoid arthritis (RA), yet there has been no consensus of the detailed strategy. Moreover, the impact of MTX on disease activity during tapering targeted therapy is still inconclusive. We aimed to investigate the interaction between the effect of tapering targeted therapy and concurrent MTX use on disease activity in patients with RA in real-world clinical practice.
Methods: This study used data from the Korean College of Rheumatology Biologics and Targeted therapy Registry (KOBIO-RA), a nationwide cohort of patients with RA receiving targeted therapy in outpatient clinics (NCT01965132). Patients were enrolled when they initiated a new targeted therapy and were followed-up annually thereafter. This study included 1-year follow-up intervals from patients treated with concomitant MTX treatment (defined as ≥ 7.5mg/week of MTX with targeted therapy) at baseline visit. As the decision on tapering is influenced by time-varying factors such as disease activity measured at the follow-up interval of last year, we used the marginal structural model in which inverse probability of treatment weights (IPTWs) for each interval was applied to control time-varying confounders. The primary outcome in this study was clinical remission based on DAS28-ESR in each follow-up interval. The effect of tapering targeted therapy, concomitant MTX treatment, and their interactions with the outcome were estimated using generalized estimating equation.
Results: A total of 3816 follow-up intervals from 1487 patients were analyzed. Tapering targeted therapy compared with previous follow-ups occurred in 816 intervals (tapering group vs. non-tapering group). Baseline clinical factors such as disease activity, dose of MTX, and concomitant glucocorticoid use were also comparable but mean (SD) DAS28-ESR (3.89 [1.8] vs. 3.3 [1.7], P < 0.001) and proportion of patients with glucocorticoid (71.2% vs. 65.4%, P = 0.002) in the previous interval was significantly lower in the tapering group. These time-varying factors were all balanced after IPTWs were applied (Table 1). The effect of tapering targeted therapy was significantly different based on whether a patients received concomitant MTX. In the subgroup of intervals with concomitant MTX, tapering targeted therapy did not affect the likelihood of achieving DAS28-remission (adjusted OR 0.99 [95% CI 0.80-1.21]). However, without concomitant MTX treatment, tapering targeted therapy was significantly associated with a lower likelihood of DAS28-remission (0.60 [0.41-0.87]) (P-value for interaction = 0.023). The result was comparable when the outcome was DAS28-low disease activity (LDA) (Table 2).
Conclusion: Tapering targeted therapy without concomitant MTX would likely result in failure to reach DAS28 remission or LDA in patients with RA.
.jpg)
Disclosures: J. Park, None; M. Kim, None; H. Kim, None; J. Kim, None; E. Lee, None; K. Shin, None.

