Back
Poster Session B
Epidemiology, health policy and outcomes
Session: (0724–0751) Health Services Research Poster II
0730: Improving Mental Health Services in Children and Adolescents with Systemic Lupus Erythematosus by Establishing a Mental Health Care Navigator
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- CC
Colleen Correll, MD, MPH
University of Minnesota
Minneapolis, MN, United States
Abstract Poster Presenter(s)
Colleen Correll, Erika Vaughn, Amanda Schlesinger and Danielle Bullock, University of Minnesota, Minneapolis, MN
Background/Purpose: Anxiety and depression are three times more common in children with childhood onset-systemic lupus erythematosus (cSLE) compared to their peers, and both are associated with increased healthcare utilization, poor medication adherence and school performance, worse outcomes and quality of life, and difficulty with transition to adult care. Lack of sufficient services for mental health (MH) care in cSLE is well-recognized in pediatric rheumatology. Lack of adequate resources is the most commonly reported barrier to screening for MH diseases and accessing care. We received grant funding to create a new position called a Mental Health Care Navigator (MHCN) to improve our MH screenings, referrals, and treatment for patients with cSLE who are seen at our Pediatric Rheumatology Clinic. Here, we present our new program and preliminary findings.
Methods: We hired an experienced clinical social worker for the MHCN role. Patients with cSLE are screened for depression and anxiety. Patients 12+ complete the Patient Health Questionnaire for Adolescents (PHQ-A) and the General Anxiety Disorder-7 (GAD-7); patients ages 8-11 complete the Center for Epidemiological Studies Depression Scale for Children (CES-DC) and Screen for Child Anxiety Related Disorders (SCARED) every 6 months at their routine rheumatology appointment. Depending on screening results, the MHCN facilities referrals to community MH providers or specialists at the University if needed (Figure 1). We are collecting outcome metrics including rates of MH screening, meeting with the MHCN, referrals and no-shows. Next steps include collecting hospitalization rates, medication adherence, and patient/family and provider perception of the MHCN program. We are also conducting four MH Training Sessions for pediatric rheumatology clinic staff.
Results: Since the initiation of the program 6 months ago, the MHCN has met with 42/61 (69%) patients with cSLE in 83 encounters. We have screened 29/61 (48%) for depression and anxiety, and we have referred 7/29 (24%) to MH services after screening; 11/29 (38%) had MH services prior to screening. The MHCN is also developing culturally competent patient educational materials, coordinating community support groups, and helping patients gain access to advocacy foundations. We have completed 1 of 4 MH training sessions for pediatric rheumatology providers.
Conclusion: cSLE is a complex disease and is associated with high rates of MH diagnoses . Despite this, patients face many barriers to accessing MH services. We created a new program using a MHCN to help patients overcome these barriers and to educate rheumatology providers. In the short time since the start of the program, the MCHN has met with the majority of our patients with cSLE, created a standardized MH screening program, and is developing a variety of resources for patients and families. We anticipate that our outcome metrics will demonstrate that this model is effective. This preliminary program can provide a model for other centers seeking to improve MH service utilization. With additional funding, we plan to expand the program to assist other pediatric rheumatology patients with complex disease and MH care needs.
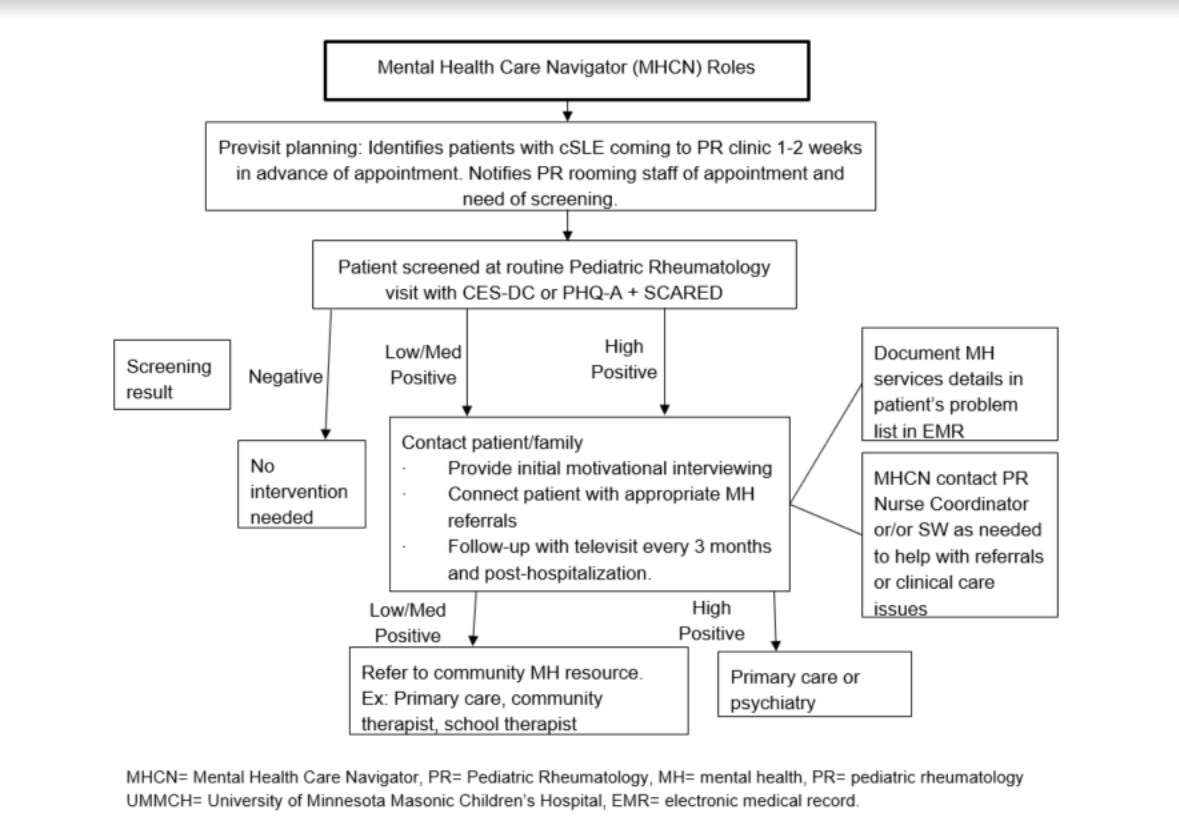 Figure 1. Process for mental health screening and referrals.
Figure 1. Process for mental health screening and referrals.
Disclosures: C. Correll, None; E. Vaughn, None; A. Schlesinger, None; D. Bullock, None.
Background/Purpose: Anxiety and depression are three times more common in children with childhood onset-systemic lupus erythematosus (cSLE) compared to their peers, and both are associated with increased healthcare utilization, poor medication adherence and school performance, worse outcomes and quality of life, and difficulty with transition to adult care. Lack of sufficient services for mental health (MH) care in cSLE is well-recognized in pediatric rheumatology. Lack of adequate resources is the most commonly reported barrier to screening for MH diseases and accessing care. We received grant funding to create a new position called a Mental Health Care Navigator (MHCN) to improve our MH screenings, referrals, and treatment for patients with cSLE who are seen at our Pediatric Rheumatology Clinic. Here, we present our new program and preliminary findings.
Methods: We hired an experienced clinical social worker for the MHCN role. Patients with cSLE are screened for depression and anxiety. Patients 12+ complete the Patient Health Questionnaire for Adolescents (PHQ-A) and the General Anxiety Disorder-7 (GAD-7); patients ages 8-11 complete the Center for Epidemiological Studies Depression Scale for Children (CES-DC) and Screen for Child Anxiety Related Disorders (SCARED) every 6 months at their routine rheumatology appointment. Depending on screening results, the MHCN facilities referrals to community MH providers or specialists at the University if needed (Figure 1). We are collecting outcome metrics including rates of MH screening, meeting with the MHCN, referrals and no-shows. Next steps include collecting hospitalization rates, medication adherence, and patient/family and provider perception of the MHCN program. We are also conducting four MH Training Sessions for pediatric rheumatology clinic staff.
Results: Since the initiation of the program 6 months ago, the MHCN has met with 42/61 (69%) patients with cSLE in 83 encounters. We have screened 29/61 (48%) for depression and anxiety, and we have referred 7/29 (24%) to MH services after screening; 11/29 (38%) had MH services prior to screening. The MHCN is also developing culturally competent patient educational materials, coordinating community support groups, and helping patients gain access to advocacy foundations. We have completed 1 of 4 MH training sessions for pediatric rheumatology providers.
Conclusion: cSLE is a complex disease and is associated with high rates of MH diagnoses . Despite this, patients face many barriers to accessing MH services. We created a new program using a MHCN to help patients overcome these barriers and to educate rheumatology providers. In the short time since the start of the program, the MCHN has met with the majority of our patients with cSLE, created a standardized MH screening program, and is developing a variety of resources for patients and families. We anticipate that our outcome metrics will demonstrate that this model is effective. This preliminary program can provide a model for other centers seeking to improve MH service utilization. With additional funding, we plan to expand the program to assist other pediatric rheumatology patients with complex disease and MH care needs.
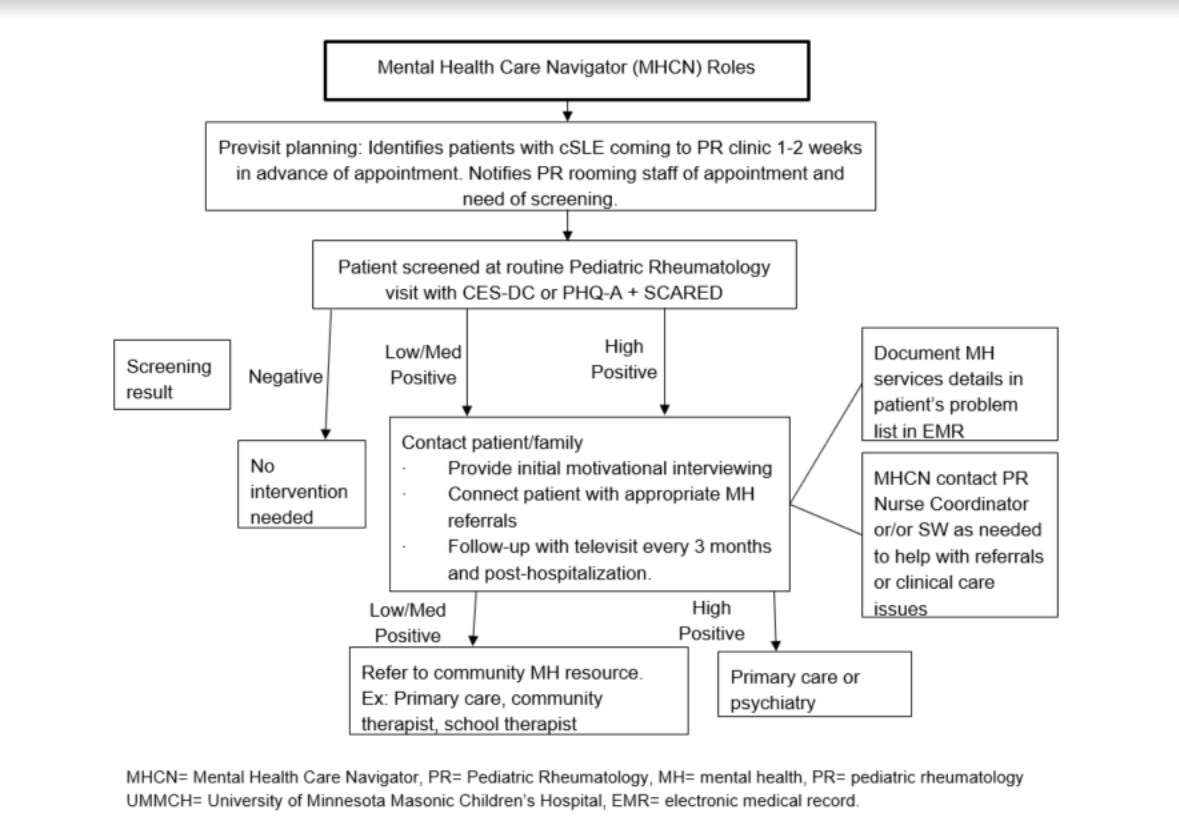 Figure 1. Process for mental health screening and referrals.
Figure 1. Process for mental health screening and referrals. Disclosures: C. Correll, None; E. Vaughn, None; A. Schlesinger, None; D. Bullock, None.

