Back
Abstract Session
Session: Abstracts: Cognition and Behavior in RA and Systemic Sclerosis (2187–2190)
2190: Characterizing Compensatory Cognitive Strategy Use in People with Systemic Sclerosis
Monday, November 14, 2022
3:45 PM – 3:55 PM Eastern Time
Location: Ballroom AB

Yen Chen, PhD
University of Michigan
Ann Arbor, MI, United States
Presenting Author(s)
Yen Chen1, Alain Lescoat2, Dinesh Khanna3 and Susan Murphy4, 1University of Michigan, Ann Arbor, MI, 2CHU Rennes - University Rennes 1, Rennes, France, 3Division of Rheumatology, Department of Internal Medicine, Scleroderma Program, University of Michigan, Ann Arbor, MI, 4University of Michigan, Grosse Ile, MI
Background/Purpose: Individuals with systemic sclerosis (SSc) report cognitive problems that worsen symptoms and daily activity performance. Compensatory cognitive strategies (CCS) are commonly taught to help people with chronic conditions manage cognitive problems. Evidence demonstrates CCS use improves symptoms and quality of life. However, current self-management programs do not include CCS. Little is known about CCS use in the SSc population. The purposes of this study are: 1) to characterize CCS use, 2) to examine if CCS use differs by demographics and SSc characteristics, and 3) to investigate associations between self-reported cognitive function and symptoms with CCS.
Methods: A cross-sectional survey was conducted. The CCS, a 24-item questionnaire, was used to assess how frequently participants use ways to decrease distractions, organize activities, avoid mistakes, and to use technologies to compensate their cognitive problems in everyday lives. The response to each item is rated on a 5-point Liker scale: 0 (never); 1 (rarely); 2 (sometimes); 3 (often); and 4 (all the time). Perceived cognitive function and symptoms (fatigue, pain, sleep disturbance, anxiety, depressed mood) were assessed with PROMIS measures. Independent t-test and one-way analysis of variance were conducted to examine whether CCS use differs by demographics and SSc characteristics. Multiple regression was conducted to examine independent associations of cognitive function and symptoms with CCS.
Results: Of 106 participants (Mean age 55.2 ± 11.5 years), most were female (84%) and White (82%). More than half (58%) had the diffuse cutaneous SSc subtype (Table 1). The most frequently used types of CCS (have the median value of 2 or higher) were organizational strategies, technology, attention strategies, lifestyle strategies, and review and confirm work to avoid mistakes (see Figure 1). The three most frequently used CCS were establishing a routine (86%), using a reminder on an electronic device (82%), and prioritizing a "to do" list (81%) (Table 2). Participants with some college or associate's degree reported significantly more CCS use compared to people with a high school degree. Participants on work disability reported more CCS use compared to homemakers and full-time employed individuals. Age, sex, race, SSc subtype, and disease duration were not significant associated with CCS. Worse cognitive function (β = -0.26, p < .05) and pain (β = 0.28, p < .05) were significantly independently associated with more CCS use. There were no significant associations of fatigue, sleep disturbance, anxiety, and depressed mood with CCS.
Conclusion: Up to 86% of participants used at least one CCS. Less educated individuals were least likely to report CCS use. Worse cognitive function and pain were associated with CCS, suggesting that it may be important to integrate CCS education in self-management programs. Future longitudinal research should investigate the effectiveness of CCS in people with SSc.
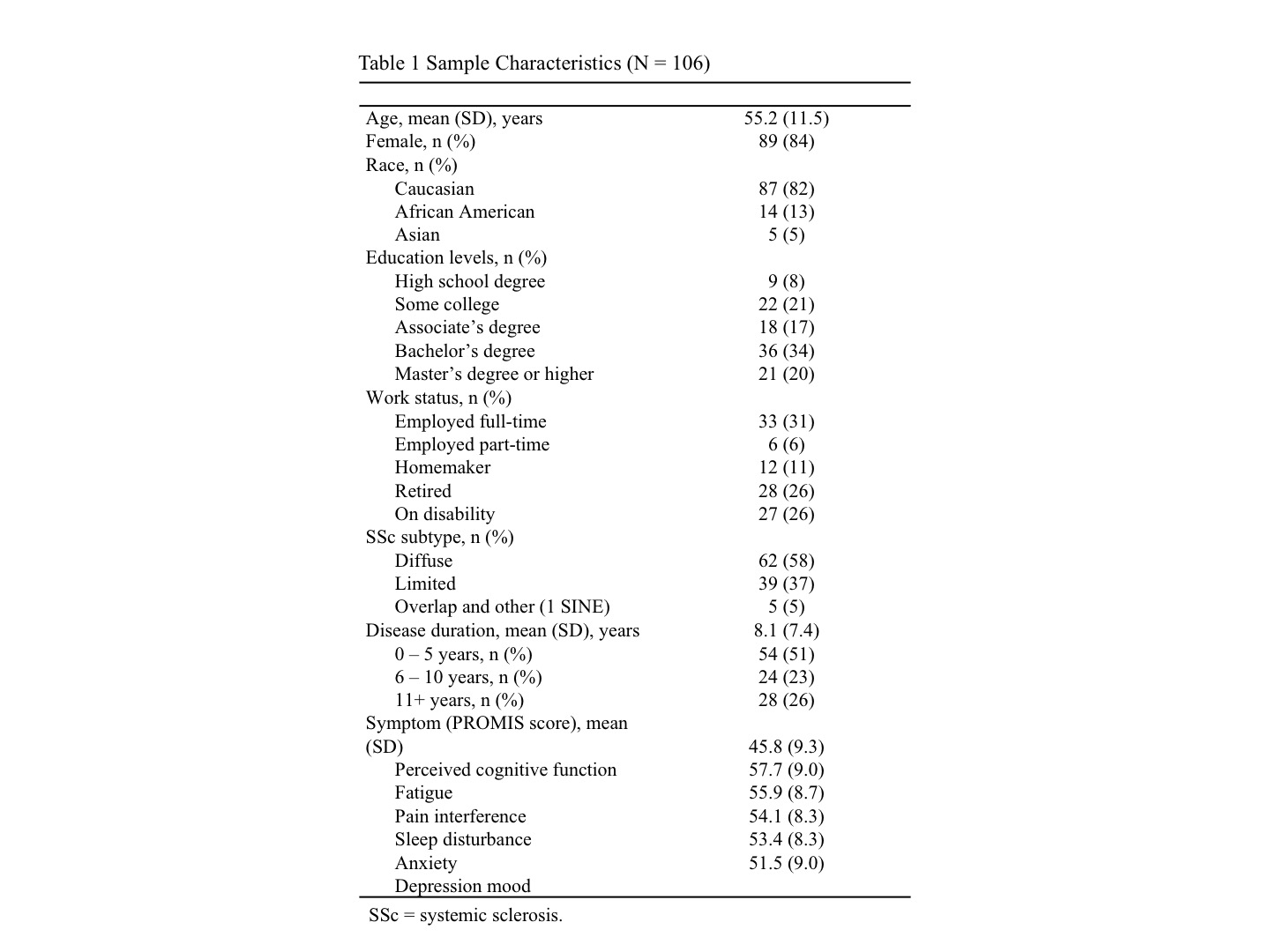 Table 1 Sample Characteristics (N = 106)
Table 1 Sample Characteristics (N = 106)
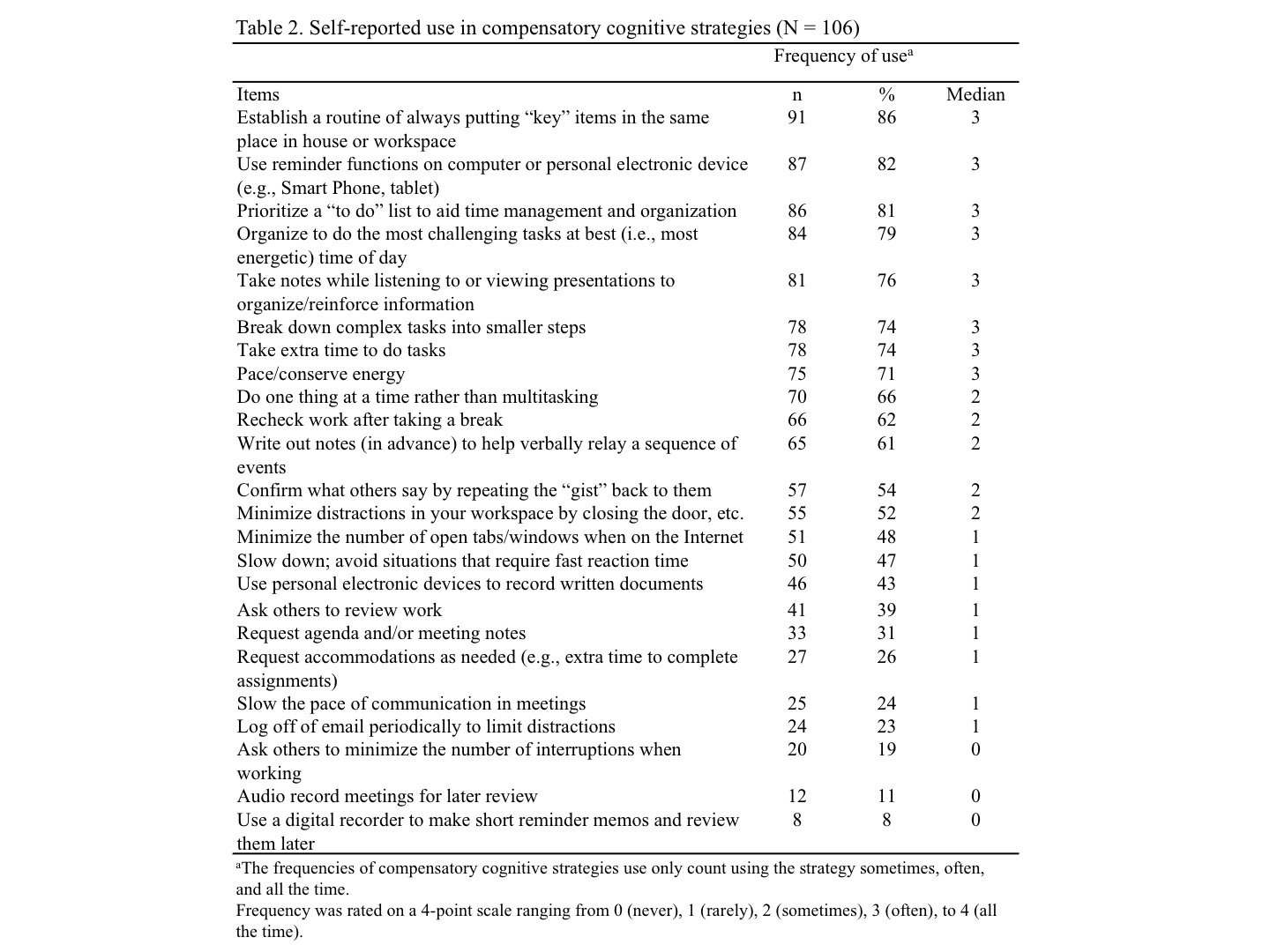 Table 2. Self-reported use in compensatory cognitive strategies (N = 106)
Table 2. Self-reported use in compensatory cognitive strategies (N = 106)
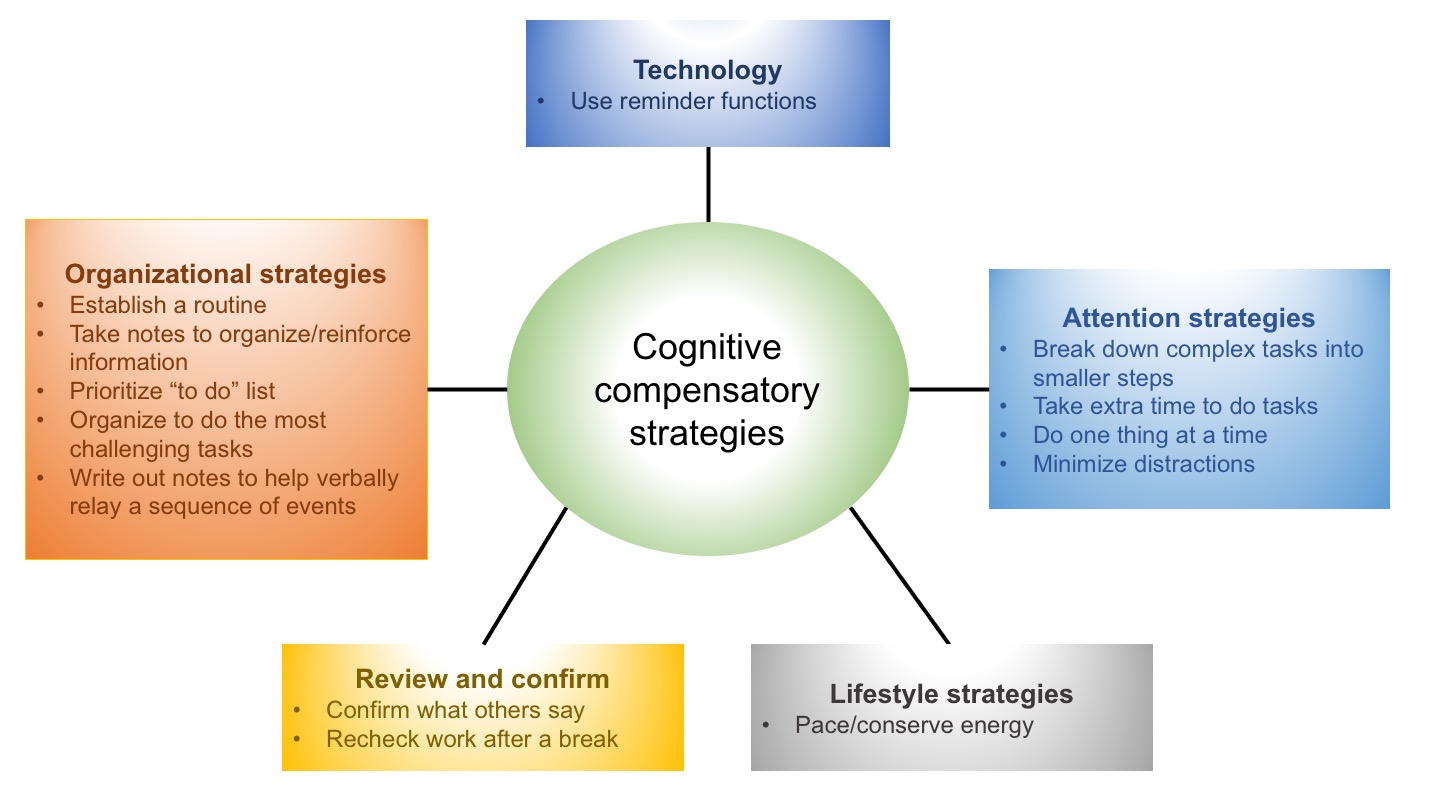 Figure 1. Cognitive compensatory strategies diagram showing different types of strategies use in patients with SSc. This diagram only presents strategies that have the median value of 2 or higher. Frequency was rated on a 4-point scale ranging from 0 (never), 1 (rarely), 2 (sometimes), 3 (often), to 4 (all the time).
Figure 1. Cognitive compensatory strategies diagram showing different types of strategies use in patients with SSc. This diagram only presents strategies that have the median value of 2 or higher. Frequency was rated on a 4-point scale ranging from 0 (never), 1 (rarely), 2 (sometimes), 3 (often), to 4 (all the time).
Disclosures: Y. Chen, None; A. Lescoat, None; D. Khanna, Boehringer Ingelheim, Genentech, Prometheus, Horizon, Chemomab, Talaris, Gesynta, Amgen, Acceleron, Actelion, Bayer, CSL Behring, Paracrine Cell Therapy, Mitsubishi Tanabe, Theraly, Eicos Sciences; S. Murphy, None.
Background/Purpose: Individuals with systemic sclerosis (SSc) report cognitive problems that worsen symptoms and daily activity performance. Compensatory cognitive strategies (CCS) are commonly taught to help people with chronic conditions manage cognitive problems. Evidence demonstrates CCS use improves symptoms and quality of life. However, current self-management programs do not include CCS. Little is known about CCS use in the SSc population. The purposes of this study are: 1) to characterize CCS use, 2) to examine if CCS use differs by demographics and SSc characteristics, and 3) to investigate associations between self-reported cognitive function and symptoms with CCS.
Methods: A cross-sectional survey was conducted. The CCS, a 24-item questionnaire, was used to assess how frequently participants use ways to decrease distractions, organize activities, avoid mistakes, and to use technologies to compensate their cognitive problems in everyday lives. The response to each item is rated on a 5-point Liker scale: 0 (never); 1 (rarely); 2 (sometimes); 3 (often); and 4 (all the time). Perceived cognitive function and symptoms (fatigue, pain, sleep disturbance, anxiety, depressed mood) were assessed with PROMIS measures. Independent t-test and one-way analysis of variance were conducted to examine whether CCS use differs by demographics and SSc characteristics. Multiple regression was conducted to examine independent associations of cognitive function and symptoms with CCS.
Results: Of 106 participants (Mean age 55.2 ± 11.5 years), most were female (84%) and White (82%). More than half (58%) had the diffuse cutaneous SSc subtype (Table 1). The most frequently used types of CCS (have the median value of 2 or higher) were organizational strategies, technology, attention strategies, lifestyle strategies, and review and confirm work to avoid mistakes (see Figure 1). The three most frequently used CCS were establishing a routine (86%), using a reminder on an electronic device (82%), and prioritizing a "to do" list (81%) (Table 2). Participants with some college or associate's degree reported significantly more CCS use compared to people with a high school degree. Participants on work disability reported more CCS use compared to homemakers and full-time employed individuals. Age, sex, race, SSc subtype, and disease duration were not significant associated with CCS. Worse cognitive function (β = -0.26, p < .05) and pain (β = 0.28, p < .05) were significantly independently associated with more CCS use. There were no significant associations of fatigue, sleep disturbance, anxiety, and depressed mood with CCS.
Conclusion: Up to 86% of participants used at least one CCS. Less educated individuals were least likely to report CCS use. Worse cognitive function and pain were associated with CCS, suggesting that it may be important to integrate CCS education in self-management programs. Future longitudinal research should investigate the effectiveness of CCS in people with SSc.
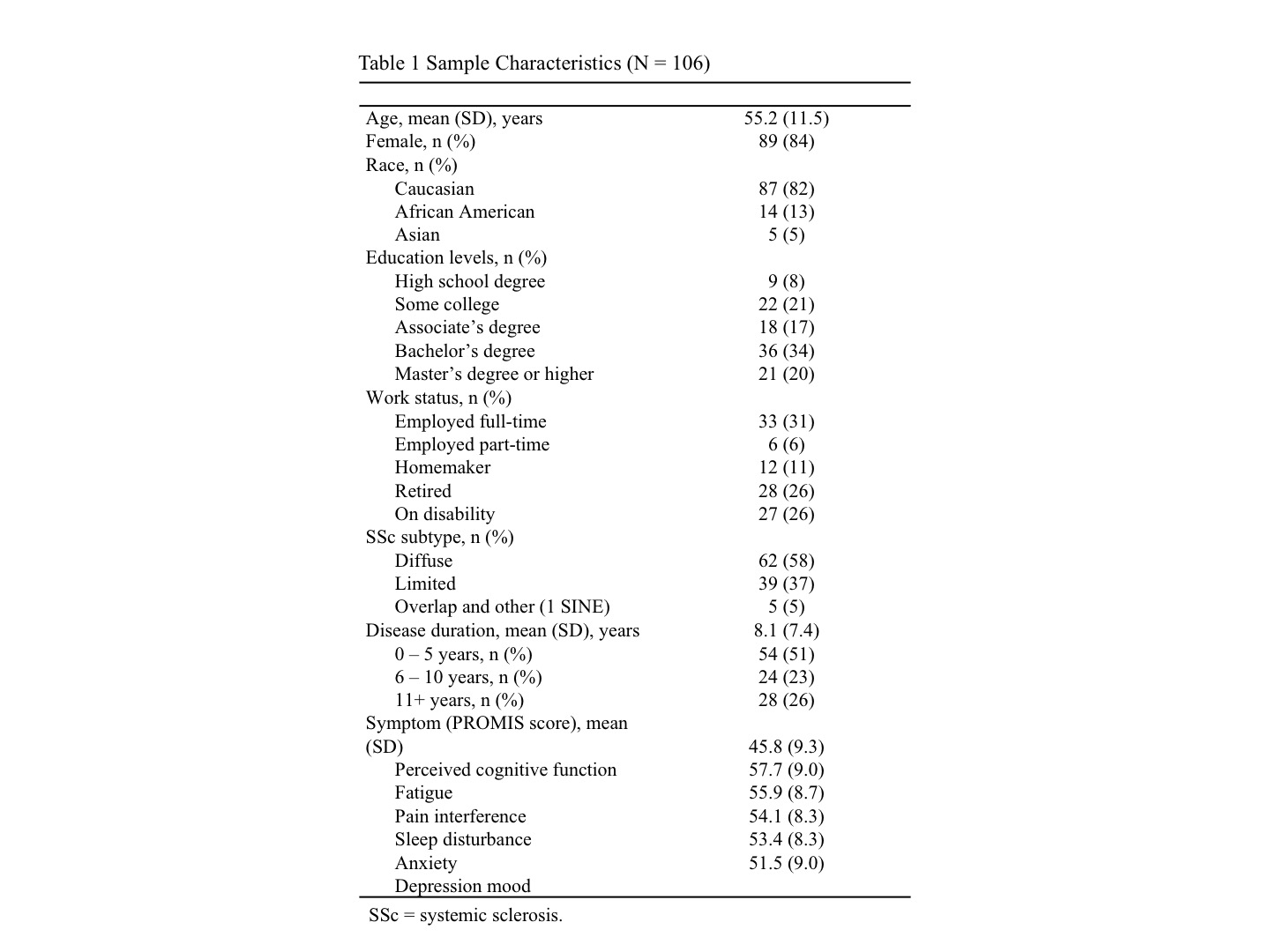 Table 1 Sample Characteristics (N = 106)
Table 1 Sample Characteristics (N = 106)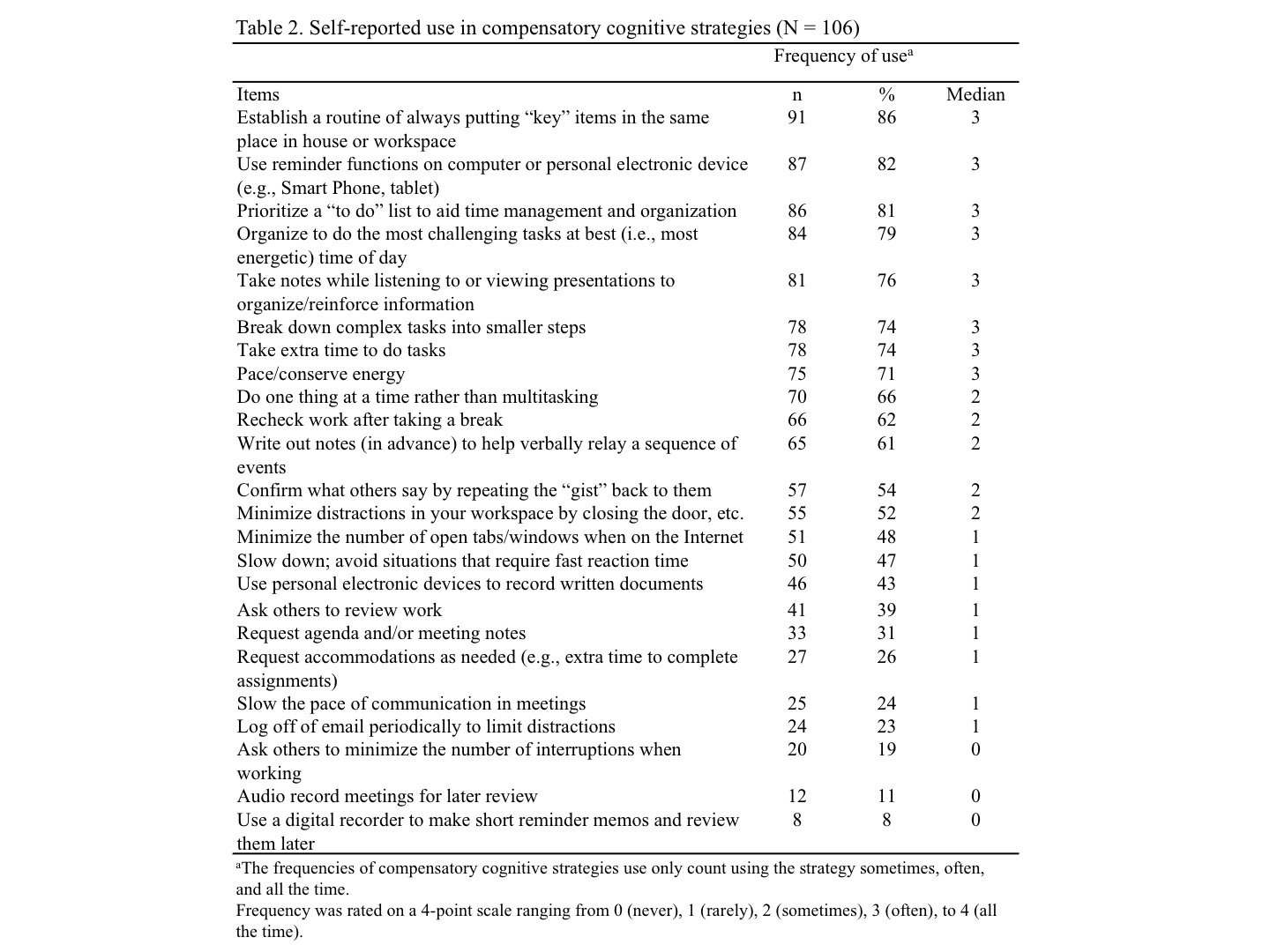 Table 2. Self-reported use in compensatory cognitive strategies (N = 106)
Table 2. Self-reported use in compensatory cognitive strategies (N = 106)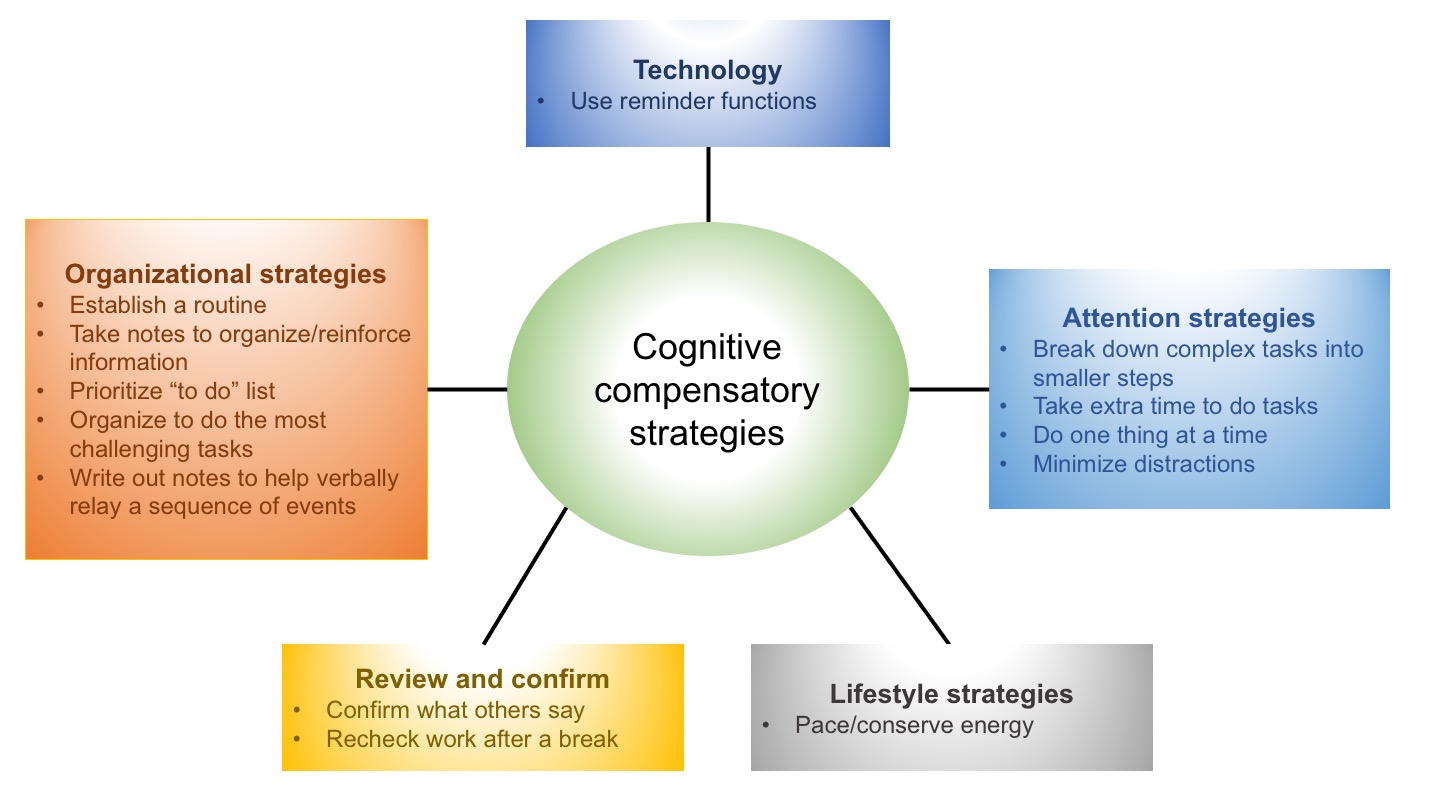 Figure 1. Cognitive compensatory strategies diagram showing different types of strategies use in patients with SSc. This diagram only presents strategies that have the median value of 2 or higher. Frequency was rated on a 4-point scale ranging from 0 (never), 1 (rarely), 2 (sometimes), 3 (often), to 4 (all the time).
Figure 1. Cognitive compensatory strategies diagram showing different types of strategies use in patients with SSc. This diagram only presents strategies that have the median value of 2 or higher. Frequency was rated on a 4-point scale ranging from 0 (never), 1 (rarely), 2 (sometimes), 3 (often), to 4 (all the time).Disclosures: Y. Chen, None; A. Lescoat, None; D. Khanna, Boehringer Ingelheim, Genentech, Prometheus, Horizon, Chemomab, Talaris, Gesynta, Amgen, Acceleron, Actelion, Bayer, CSL Behring, Paracrine Cell Therapy, Mitsubishi Tanabe, Theraly, Eicos Sciences; S. Murphy, None.

