Back
Poster Session B
Juvenile idiopathic arthritis (JIA) and pediatric joint disorders
Session: (0850–0880) Pediatric Rheumatology – Clinical Poster I: JIA
0877: Neutrophils Extracellular Traps Formation May Serve as a Biomarker for Disease Activity in Oligoarticular Juvenile Idiopathic Arthritis
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- MH
Merav Heshin Bekenstein, MD
Tel Aviv Medical Center Israel
Binyamina, Israel
Abstract Poster Presenter(s)
Merav Heshin-Bekenstein1, Szilvia Baron2, Grant Schulert3, Anna Shusterman4, Rachel Shukrun4, Yoav Binenbaum4 and Ronit Elhasid5, 1Dana Dwek Children's Hospital, Tel Aviv Medical Center Israel, Binyamina, Israel, 2Pediatric Hemato-Oncology Research Laboratory, Tel Aviv Medical Center, Tel Aviv, Israel, 3Cincinnati Children's Hospital Medical Center, Cincinnati, OH, 4Tel Aviv Medical Center, Tel Aviv, Israel, 5Dana Children's Hospital, Tel Aviv Medical Center, Tel Aviv, Israel
Background/Purpose: Juvenile idiopathic arthritis (JIA) is the most common chronic rheumatic disease in children, causing significant morbidity. Despite the dramatic improvement in treatment, many patients do not achieve complete remission, and biomarkers for subclinical disease, flares, and response to treatment are lacking. Neutrophils and neutrophil extracellular traps (NETs) were revealed to partake in the pathogenesis of autoimmune and inflammatory conditions, but their role in JIA pathogenesis and as biomarkers for JIA disease activity are largely unexplored. In this study, we aimed to characterize the neutrophil enzymatic activity and NETs in oligoarticular and polyarticular JIA and explored its association with disease activity.
Methods: Neutrophils from 7 patients with oligoarticular and RF negative polyarticular JIA were isolated at the time of diagnosis and after glucocorticoid intraarticular injection with or without DMARD treatment. Enzymatic activity of neutrophil granular enzymes was monitored by colorimetry, while NET formation was assessed using a confocal fluorescence microscope.
Results: In oligoarticular JIA patients (n=4), all disease activity parameters and neutrophil function-related parameters decreased following intraarticular steroid injection. However, only three parameters exhibited statistically significant decline, including Physician Global Assessment (PhGA), Juvenile Activity Disease Activity Score-10 (JADAS-10), and clinical JADAS-10 (cJADAS-10). Importantly, NET formation was strongly positively correlated with the cJADAS-10 at all time points (R=0.93, p=0.007). In polyarticular JIA patients (n=3), neither clinical disease activity parameters, the CRP, or the neutrophil function-related parameters showed consistent and significant decreases after steroid injections. Similarly, there no significant correlation was found between NETs formation and cJADAS-10 in polyarticular JIA patients.
Conclusion: This is the first study exploring the link between NETs formation and JIA activity. In this pilot study, we demonstrated a statistically significant linear correlation between cJADAS-10 and NETs formation in oligoarticular but not in polyarticular JIA patients. Hence, we suggest that NETs might play a role in JIA activity and may serve as a putative biomarker for treatment response. Further work is needed to validate these initial results and determine dynamics of NETosis in JIA.
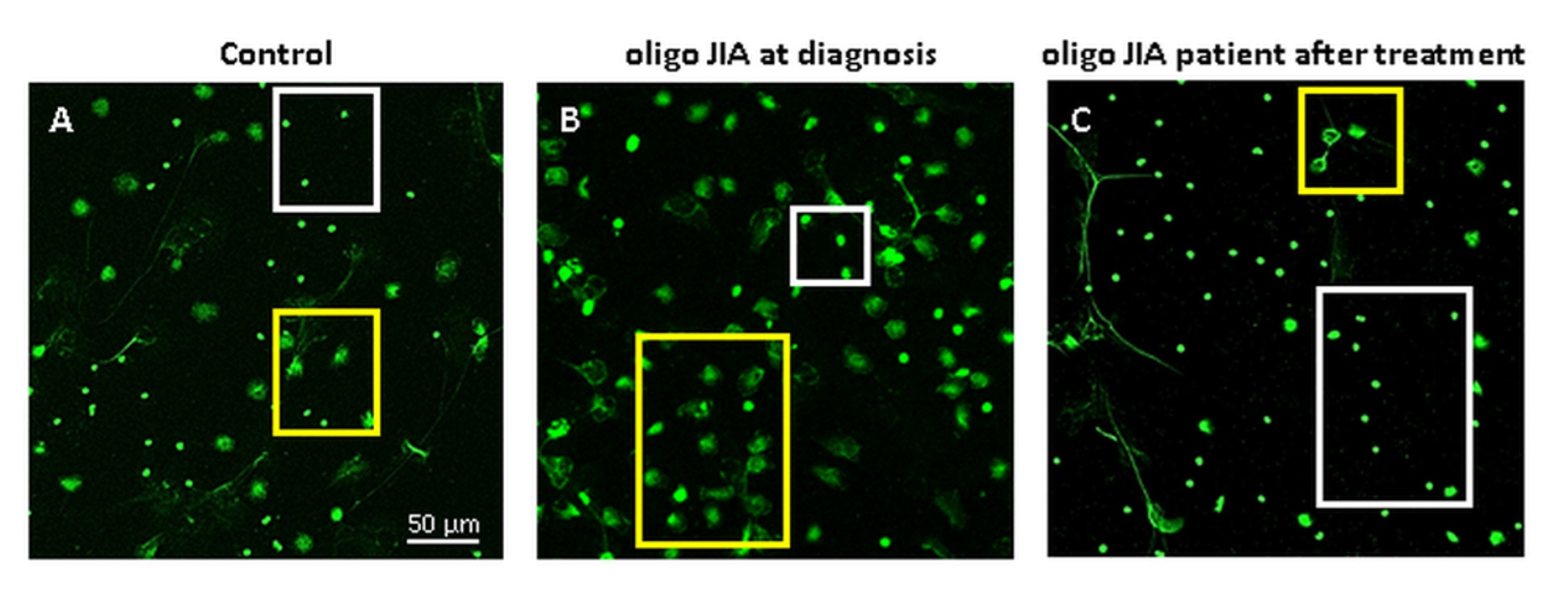 Anti-inflammatory treatment results in NETs formation inhibition. Immunofluorescent staining demonstrating NETs formation in 3 samples: (A) control; (B) an oligo JIA patient at diagnosis; (C) an oligo JIA patient after anti-inflamatory treatment. Images demonstrate a significant increase in NETs formation among JIA patient at diagnosis in comparison to control. In addition, inhibition of NET formation following treatment initiation is shown. White rectangles represent non-NETing neutrophils, while yellow rectangles contain NETing neutrophils
Anti-inflammatory treatment results in NETs formation inhibition. Immunofluorescent staining demonstrating NETs formation in 3 samples: (A) control; (B) an oligo JIA patient at diagnosis; (C) an oligo JIA patient after anti-inflamatory treatment. Images demonstrate a significant increase in NETs formation among JIA patient at diagnosis in comparison to control. In addition, inhibition of NET formation following treatment initiation is shown. White rectangles represent non-NETing neutrophils, while yellow rectangles contain NETing neutrophils
Disclosures: M. Heshin-Bekenstein, None; S. Baron, None; G. Schulert, Novartis, SOBI; A. Shusterman, None; R. Shukrun, None; Y. Binenbaum, None; R. Elhasid, None.
Background/Purpose: Juvenile idiopathic arthritis (JIA) is the most common chronic rheumatic disease in children, causing significant morbidity. Despite the dramatic improvement in treatment, many patients do not achieve complete remission, and biomarkers for subclinical disease, flares, and response to treatment are lacking. Neutrophils and neutrophil extracellular traps (NETs) were revealed to partake in the pathogenesis of autoimmune and inflammatory conditions, but their role in JIA pathogenesis and as biomarkers for JIA disease activity are largely unexplored. In this study, we aimed to characterize the neutrophil enzymatic activity and NETs in oligoarticular and polyarticular JIA and explored its association with disease activity.
Methods: Neutrophils from 7 patients with oligoarticular and RF negative polyarticular JIA were isolated at the time of diagnosis and after glucocorticoid intraarticular injection with or without DMARD treatment. Enzymatic activity of neutrophil granular enzymes was monitored by colorimetry, while NET formation was assessed using a confocal fluorescence microscope.
Results: In oligoarticular JIA patients (n=4), all disease activity parameters and neutrophil function-related parameters decreased following intraarticular steroid injection. However, only three parameters exhibited statistically significant decline, including Physician Global Assessment (PhGA), Juvenile Activity Disease Activity Score-10 (JADAS-10), and clinical JADAS-10 (cJADAS-10). Importantly, NET formation was strongly positively correlated with the cJADAS-10 at all time points (R=0.93, p=0.007). In polyarticular JIA patients (n=3), neither clinical disease activity parameters, the CRP, or the neutrophil function-related parameters showed consistent and significant decreases after steroid injections. Similarly, there no significant correlation was found between NETs formation and cJADAS-10 in polyarticular JIA patients.
Conclusion: This is the first study exploring the link between NETs formation and JIA activity. In this pilot study, we demonstrated a statistically significant linear correlation between cJADAS-10 and NETs formation in oligoarticular but not in polyarticular JIA patients. Hence, we suggest that NETs might play a role in JIA activity and may serve as a putative biomarker for treatment response. Further work is needed to validate these initial results and determine dynamics of NETosis in JIA.
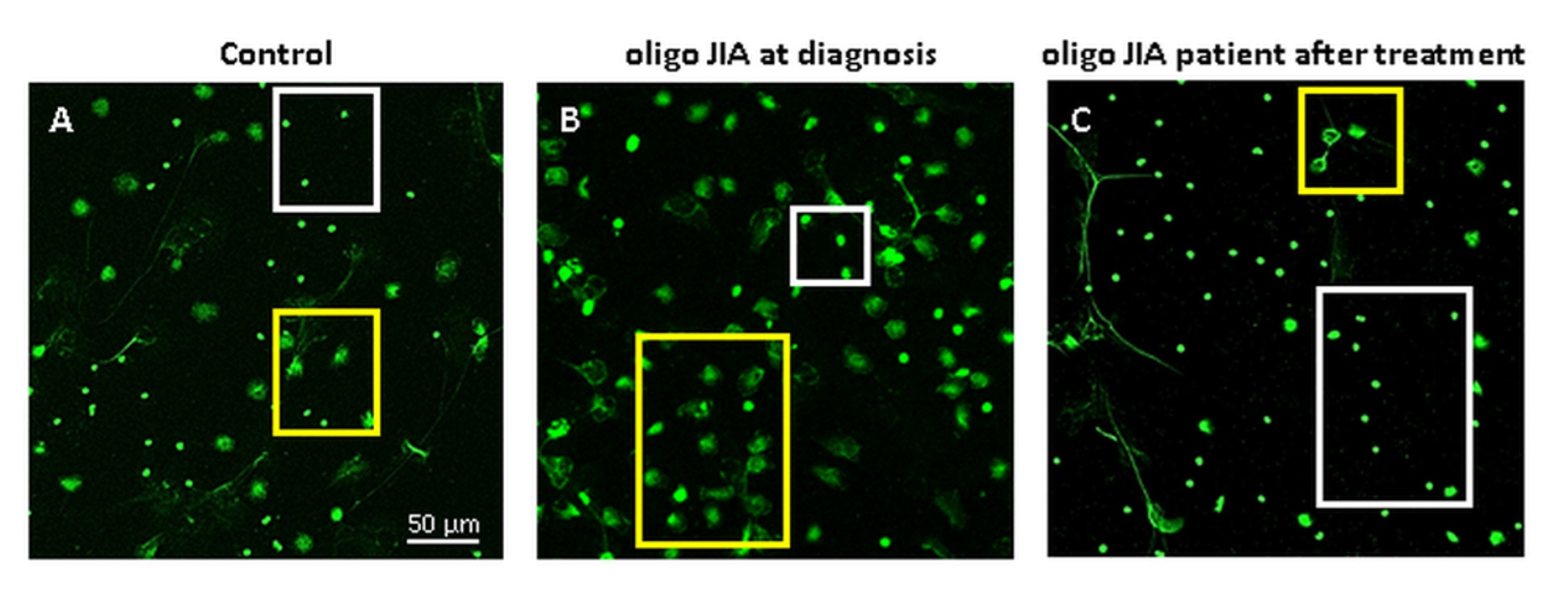 Anti-inflammatory treatment results in NETs formation inhibition. Immunofluorescent staining demonstrating NETs formation in 3 samples: (A) control; (B) an oligo JIA patient at diagnosis; (C) an oligo JIA patient after anti-inflamatory treatment. Images demonstrate a significant increase in NETs formation among JIA patient at diagnosis in comparison to control. In addition, inhibition of NET formation following treatment initiation is shown. White rectangles represent non-NETing neutrophils, while yellow rectangles contain NETing neutrophils
Anti-inflammatory treatment results in NETs formation inhibition. Immunofluorescent staining demonstrating NETs formation in 3 samples: (A) control; (B) an oligo JIA patient at diagnosis; (C) an oligo JIA patient after anti-inflamatory treatment. Images demonstrate a significant increase in NETs formation among JIA patient at diagnosis in comparison to control. In addition, inhibition of NET formation following treatment initiation is shown. White rectangles represent non-NETing neutrophils, while yellow rectangles contain NETing neutrophilsDisclosures: M. Heshin-Bekenstein, None; S. Baron, None; G. Schulert, Novartis, SOBI; A. Shusterman, None; R. Shukrun, None; Y. Binenbaum, None; R. Elhasid, None.

