Back
Poster Session B
Vasculitis
Session: (1071–1093) Vasculitis – ANCA-Associated Poster II: Treatment Efficacy, Clinical Outcomes, Biomarkers
1082: Outcomes of Methotrexate as an Initial Induction and Maintenance Regimen for Localized Granulomatosis with Polyangiitis: A Retrospective Review
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- PB
Pratyusha Banik, MD
Oregon Health & Science University
Portland, OR, United States
Abstract Poster Presenter(s)
Pratyusha Banik1, Marcia Friedman2, Daniela Ghetie3, Dongseok Choi4 and Margaret Brophy1, 1Oregon Health & Science University, Portland, OR, 2Oregon Health and Science University, Division of Arthritis and Rheumatic Diseases, Portland, OR, 3Oregon Health & Science University, Division of Arthritis and Rheumatic Diseases, Lake Oswego, OR, 4OHSU-PSU School of Public Health, Portland, OR
Background/Purpose: While there is established data regarding the induction and maintenance treatment of systemic or organ threatening granulomatosis with polyangiitis (GPA), there is limited data regarding the outcomes of methotrexate (MTX) as an initial induction and maintenance regimen for localized GPA.
Methods: A retrospective chart review was performed of all patients at Oregon Health & Science University with a diagnosis of localized GPA (confirmed by a rheumatologist) treated initially with MTX and glucocorticoids as induction and MTX as maintenance treatment. Exclusion criteria were systemic involvement (glomerulonephritis, symptomatic pulmonary infiltrates, alveolar hemorrhage, pachymeningitis, mononeuritis multiplex, cardiac or mesenteric involvement), prior induction with rituximab (RTX) or CYC, and insufficient documentation in medical records to monitor response. Data were abstracted from charts at the initial visit when MTX was first prescribed (Table 1), and at 3, 6, and 12 month follow ups. At each visit, clinical data were collected including a Birmingham Vasculitis Activity Score (BVAS, version 3) calculated based on chart documentation, current therapy (MTX/corticosteroid doses), treatment decisions (continue or escalate therapy and reasons for doing so), and disease status (remission, persistent disease, localized organ threatening disease, or progression to systemic involvement). Remission was defined as a BVAS score of 0 on MTX and ≤5 mg prednisone daily. Persistent disease was defined as a BVAS score of greater than 0 but no new/worsening disease. Localized organ threatening disease was defined as having localized worsening symptoms placing tissues or patients at risk of permanent damage. The primary outcomes were remission rate at 12 months of MTX therapy, rate of requiring RTX or CYC, and rate of progression to systemic disease prior to 12 months.
Results: A total of 31 patients were included in the analysis (Figure 1). The most common clinical manifestation was sinusitis (Figure 2). 15/31 patients (48%) patients were in remission at one year on MTX and prednisone ≤ 5 mg/day. 12/31 patients (39%) required RTX or CYC prior to one year; 6 for organ threatening localized disease (1 each for necrotizing scleritis, progressive tracheal stenosis, retro-orbital disease, saddle nose deformity, diplopia, and 2 for hearing loss), 3 for persistently active localized disease, and 3 (9.5%) for progression to systemic disease. Of the 15 patients who achieved remission on MTX at one year, 3 patients required RTX after the 12-month mark; 1 developed glomerulonephritis, 1 developed organ threatening disease, and 1 had persistent disease requiring repeated high dose prednisone.
Conclusion: In this real-world retrospective analysis, among patients with localized GPA treated initially with MTX and glucocorticoids, 48% achieved remission at one year of therapy. 9.5% patients developed systemic disease prior to one year of therapy. MTX can be a highly effective initial therapy for some patients with localized GPA, however many patients will ultimately require escalation to rituximab or cyclophosphamide.
.jpg) Table 1
Table 1
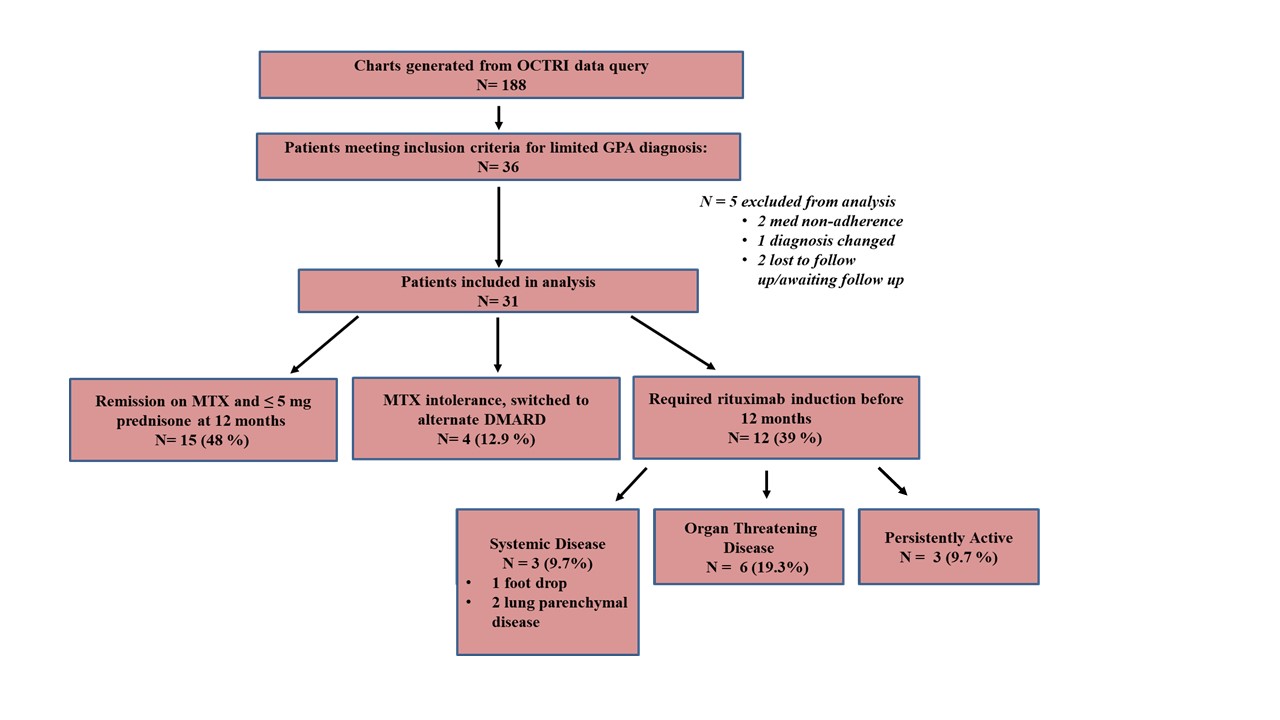 Figure 1
Figure 1
.jpg) Figure 2
Figure 2
Disclosures: P. Banik, None; M. Friedman, revolo; D. Ghetie, None; D. Choi, None; M. Brophy, None.
Background/Purpose: While there is established data regarding the induction and maintenance treatment of systemic or organ threatening granulomatosis with polyangiitis (GPA), there is limited data regarding the outcomes of methotrexate (MTX) as an initial induction and maintenance regimen for localized GPA.
Methods: A retrospective chart review was performed of all patients at Oregon Health & Science University with a diagnosis of localized GPA (confirmed by a rheumatologist) treated initially with MTX and glucocorticoids as induction and MTX as maintenance treatment. Exclusion criteria were systemic involvement (glomerulonephritis, symptomatic pulmonary infiltrates, alveolar hemorrhage, pachymeningitis, mononeuritis multiplex, cardiac or mesenteric involvement), prior induction with rituximab (RTX) or CYC, and insufficient documentation in medical records to monitor response. Data were abstracted from charts at the initial visit when MTX was first prescribed (Table 1), and at 3, 6, and 12 month follow ups. At each visit, clinical data were collected including a Birmingham Vasculitis Activity Score (BVAS, version 3) calculated based on chart documentation, current therapy (MTX/corticosteroid doses), treatment decisions (continue or escalate therapy and reasons for doing so), and disease status (remission, persistent disease, localized organ threatening disease, or progression to systemic involvement). Remission was defined as a BVAS score of 0 on MTX and ≤5 mg prednisone daily. Persistent disease was defined as a BVAS score of greater than 0 but no new/worsening disease. Localized organ threatening disease was defined as having localized worsening symptoms placing tissues or patients at risk of permanent damage. The primary outcomes were remission rate at 12 months of MTX therapy, rate of requiring RTX or CYC, and rate of progression to systemic disease prior to 12 months.
Results: A total of 31 patients were included in the analysis (Figure 1). The most common clinical manifestation was sinusitis (Figure 2). 15/31 patients (48%) patients were in remission at one year on MTX and prednisone ≤ 5 mg/day. 12/31 patients (39%) required RTX or CYC prior to one year; 6 for organ threatening localized disease (1 each for necrotizing scleritis, progressive tracheal stenosis, retro-orbital disease, saddle nose deformity, diplopia, and 2 for hearing loss), 3 for persistently active localized disease, and 3 (9.5%) for progression to systemic disease. Of the 15 patients who achieved remission on MTX at one year, 3 patients required RTX after the 12-month mark; 1 developed glomerulonephritis, 1 developed organ threatening disease, and 1 had persistent disease requiring repeated high dose prednisone.
Conclusion: In this real-world retrospective analysis, among patients with localized GPA treated initially with MTX and glucocorticoids, 48% achieved remission at one year of therapy. 9.5% patients developed systemic disease prior to one year of therapy. MTX can be a highly effective initial therapy for some patients with localized GPA, however many patients will ultimately require escalation to rituximab or cyclophosphamide.
.jpg) Table 1
Table 1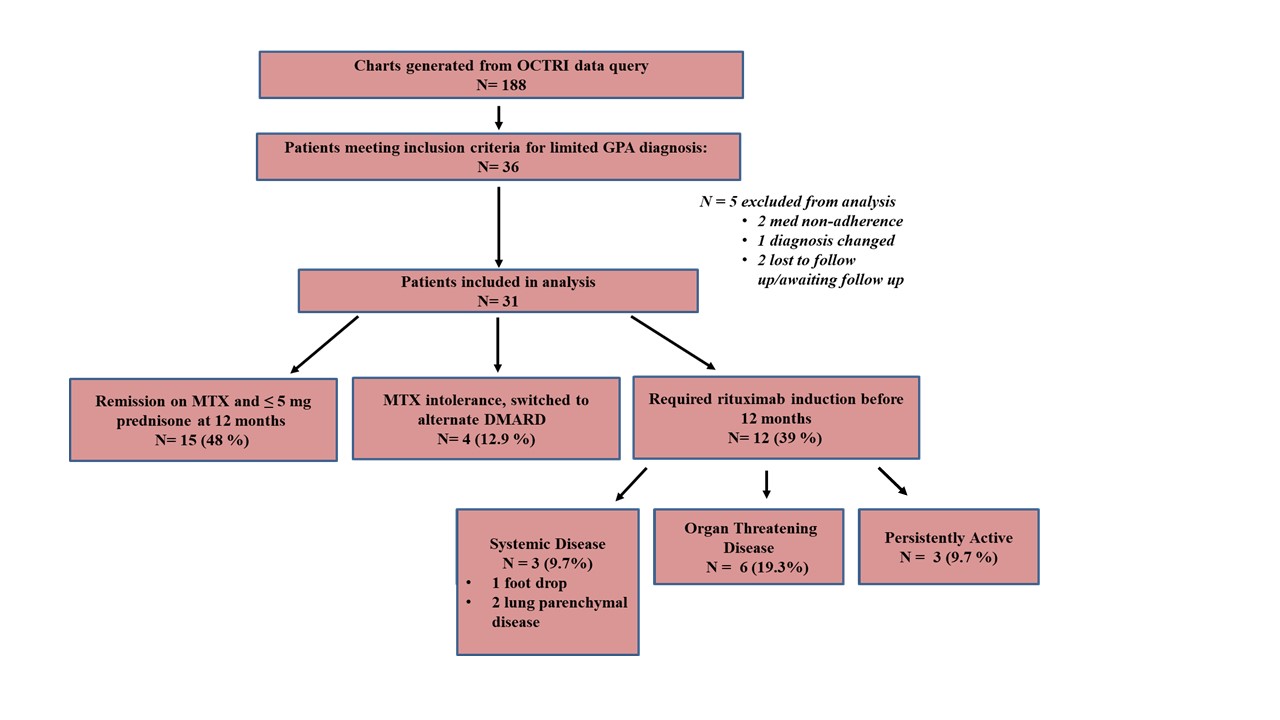 Figure 1
Figure 1.jpg) Figure 2
Figure 2Disclosures: P. Banik, None; M. Friedman, revolo; D. Ghetie, None; D. Choi, None; M. Brophy, None.

