Back
Poster Session B
Rheumatoid arthritis (RA)
Session: (0883–0912) RA – Diagnosis, Manifestations, and Outcomes Poster II
0906: Patients with Seronegative Rheumatoid Arthritis Have a Different Ultrasound-assessed Joint Disease Phenotype Than Seropositive Patients
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- NC
Natalia Carbonell-Bobadilla, MD
National Institute of Cardiology Ignacio Chávez
Ciudad de México, Federal District, Mexico
Abstract Poster Presenter(s)
Natalia Carbonell-Bobadilla1, Carina Soto-Fajardo2, Luis M Amezcua-Guerra3, Ana Beatriz Batres Marroquin4, Ana Cristina Medina5, Tania Vargas3, Adrián Hernández-Diazcouder3, Valentín Jiménez-Rojas3, Carlos Pineda5 and Luis H Silveira6, 1National Institute of Cardiology Ignacio Chávez, Ciudad de México, Mexico, 2Instituto Nacional de Rehabilitacion \"Luis Guillermo Ibarra Ibarra\", Ciudad de México, Mexico, 3Instituto Nacional de Cardiología Ignacio Chávez, Ciudad de México, Mexico, 4Instituto Nacional de Rehabilitación Luis Guillermo Ibarra Ibarra, Ciudad de México, Mexico, 5Instituto Nacional de Rehabilitacion, Ciudad de México, Mexico, 6Instituto Nacional de Cardiología, Ciudad de México, Mexico
Background/Purpose: Seronegative rheumatoid arthritis (SNRA) tends to be less severe in its presentation and evolution than seropositive rheumatoid arthritis(SPRA), but controversy exists because there have been studies that show no differences between them.
The present study was aimed to evaluate if SNRA patients show lesser clinical severity, cardiovascular risk and morphostructural abnormalities assessed by US than SPRA patients.
Methods: Patients were enrolled as SNRA or SPRA, according to their RF and ACPA status.The degree of disease activity was established by DAS28-PCR 3 elements, Clinical disease activity index(CDAI) and Simple disease activity index(SDAI) .The cardiovascular risk scores Framingham 10-years risk, Reynolds, American College of Cardiology /American Heart Heart Association (ACC/AHA), and QRISK 3 were calculated.
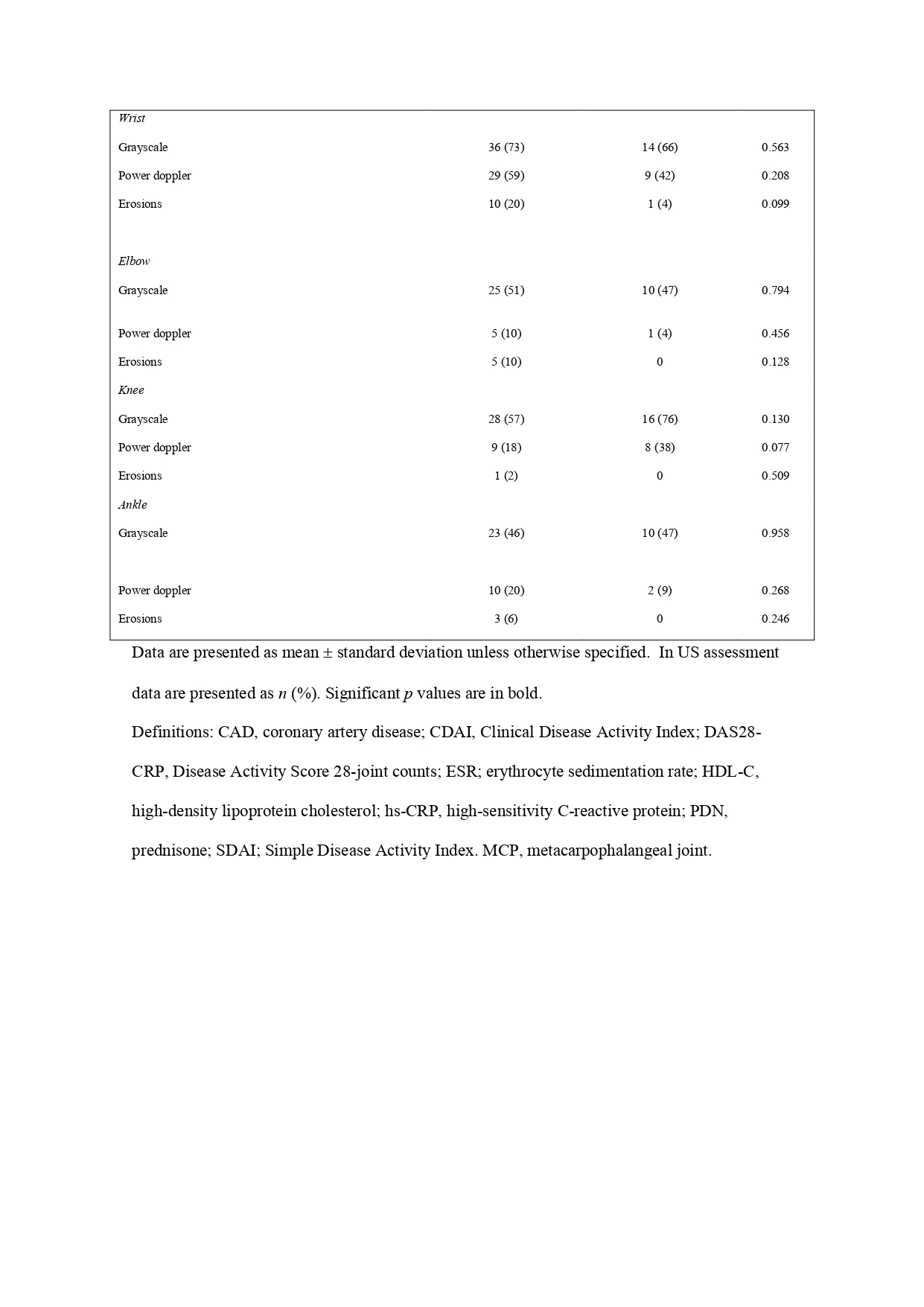
US examinations were performed using MyLab7 (Esaote Biomedica, Genoa, Italy) equipped with a 6- to 18-MHzbroadband linear transducer. The images were scored for synovitis in Grey-Scale (GS) and Power Doppler (PD) according to the EULAR-OMERACT score system.
Results: Between 2019 and 2022, 114 patients were enrolled. 92 were women (n=65 SPRA 76% and n=27 SNRA 93%; p= 0.050). The age was 54 ± 13 IQR in ARSP and 63 ± 9 IQR in SNRA; p= < 0.001. The age of disease onset was 43 ± 14 IQR in SPRA and 54 ± 11 IQR in SNRA; p= < 0.001.
The treatment between patients had significative differences in the use of SSZ, CS , and in the median of the dose used in SPRA compared with SNRA.
Patients with SPRA had a higher proportion of synovitis in the right 2MCP joint (71 vs 38% p=0.008) and in the left ankle (29 vs 5%, p=0. 026). We also find in the right knee a higher proportion of patients with SNRA with grade >2 synovitis (52 vs 23%, p=0.023). In PD we found differences in the right 2MCP joint (49 vs 9% p=0.002), left 2MCP joint (35 vs 10%, p=0.03); and right 3MCP joint (39 vs 14%, p=0.043). We also found a higher proportion of patients with SNRA with PD in the left knee (33 vs 10% p=0.019). Patients with SPRA had a higher proportion of erosions in all sites evaluated (9 vs 1%, p< 0.001).
Conclusion: We found in our study that SNRA has a different phenotype compared to SPRA. It expresses later in life, with lesser need of combination therapy and with greater glucocorticoid dosage than seropositive patients. By US assessment, SPRA patients had a higher proportion of synovitis in the right 2MCP joint and in the left ankle and higher proportion of erosions.SNRA patients had a higher proportion of synovitis in the knee. Surprisingly, we did not find differences between groups in clinical assessment and cardiovascular 10 years risk scores.
.jpg) Table 1. Clinical and laboratory features of patients with rheumatoid arthritis.
Table 1. Clinical and laboratory features of patients with rheumatoid arthritis.
Disclosures: N. Carbonell-Bobadilla, None; C. Soto-Fajardo, None; L. Amezcua-Guerra, None; A. Batres Marroquin, None; A. Medina, None; T. Vargas, None; A. Hernández-Diazcouder, None; V. Jiménez-Rojas, None; C. Pineda, None; L. Silveira, None.
Background/Purpose: Seronegative rheumatoid arthritis (SNRA) tends to be less severe in its presentation and evolution than seropositive rheumatoid arthritis(SPRA), but controversy exists because there have been studies that show no differences between them.
The present study was aimed to evaluate if SNRA patients show lesser clinical severity, cardiovascular risk and morphostructural abnormalities assessed by US than SPRA patients.
Methods: Patients were enrolled as SNRA or SPRA, according to their RF and ACPA status.The degree of disease activity was established by DAS28-PCR 3 elements, Clinical disease activity index(CDAI) and Simple disease activity index(SDAI) .The cardiovascular risk scores Framingham 10-years risk, Reynolds, American College of Cardiology /American Heart Heart Association (ACC/AHA), and QRISK 3 were calculated.
US examinations were performed using MyLab7 (Esaote Biomedica, Genoa, Italy) equipped with a 6- to 18-MHzbroadband linear transducer. The images were scored for synovitis in Grey-Scale (GS) and Power Doppler (PD) according to the EULAR-OMERACT score system.
Results: Between 2019 and 2022, 114 patients were enrolled. 92 were women (n=65 SPRA 76% and n=27 SNRA 93%; p= 0.050). The age was 54 ± 13 IQR in ARSP and 63 ± 9 IQR in SNRA; p= < 0.001. The age of disease onset was 43 ± 14 IQR in SPRA and 54 ± 11 IQR in SNRA; p= < 0.001.
The treatment between patients had significative differences in the use of SSZ, CS , and in the median of the dose used in SPRA compared with SNRA.
Patients with SPRA had a higher proportion of synovitis in the right 2MCP joint (71 vs 38% p=0.008) and in the left ankle (29 vs 5%, p=0. 026). We also find in the right knee a higher proportion of patients with SNRA with grade >2 synovitis (52 vs 23%, p=0.023). In PD we found differences in the right 2MCP joint (49 vs 9% p=0.002), left 2MCP joint (35 vs 10%, p=0.03); and right 3MCP joint (39 vs 14%, p=0.043). We also found a higher proportion of patients with SNRA with PD in the left knee (33 vs 10% p=0.019). Patients with SPRA had a higher proportion of erosions in all sites evaluated (9 vs 1%, p< 0.001).
Conclusion: We found in our study that SNRA has a different phenotype compared to SPRA. It expresses later in life, with lesser need of combination therapy and with greater glucocorticoid dosage than seropositive patients. By US assessment, SPRA patients had a higher proportion of synovitis in the right 2MCP joint and in the left ankle and higher proportion of erosions.SNRA patients had a higher proportion of synovitis in the knee. Surprisingly, we did not find differences between groups in clinical assessment and cardiovascular 10 years risk scores.
.jpg) Table 1. Clinical and laboratory features of patients with rheumatoid arthritis.
Table 1. Clinical and laboratory features of patients with rheumatoid arthritis.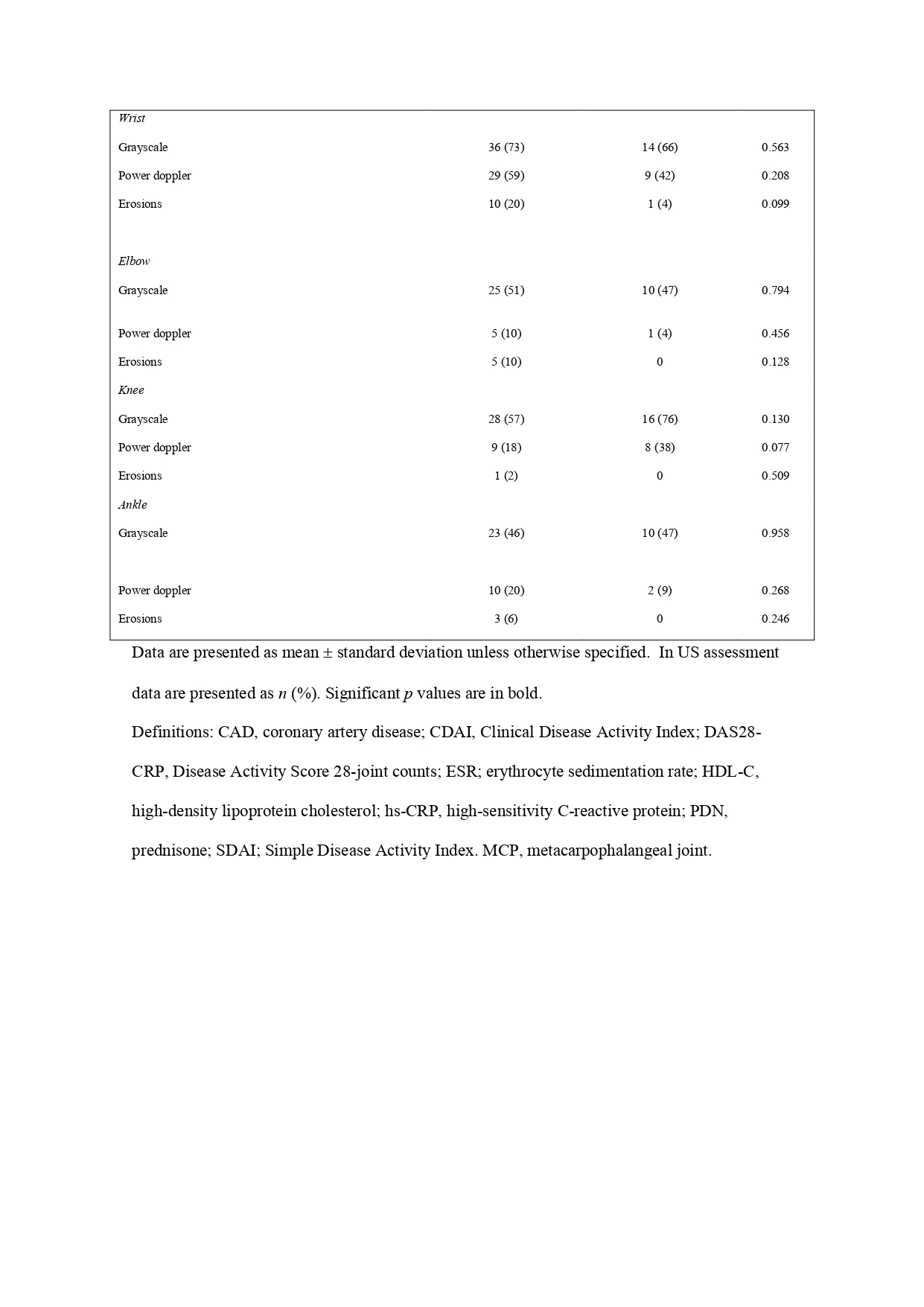
Disclosures: N. Carbonell-Bobadilla, None; C. Soto-Fajardo, None; L. Amezcua-Guerra, None; A. Batres Marroquin, None; A. Medina, None; T. Vargas, None; A. Hernández-Diazcouder, None; V. Jiménez-Rojas, None; C. Pineda, None; L. Silveira, None.

