Back
Poster Session B
Osteoarthritis (OA) and related disorders
Session: (0833–0849) Orthopedics, Low Back Pain, and Rehabilitation Poster
0840: Postoperative Risk of Immunosuppression in Rheumatic Disease Patients Undergoing Arthroscopy
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- JS
Jonathan Samuels, MD, RhMSUS
NYU Langone
Rye Brook, NY, United States
Abstract Poster Presenter(s)
Kinjal Vasvada, Laith Jazrawi and Jonathan Samuels, NYU Langone Health, New York, NY
Background/Purpose: Recent literature suggests that rheumatic disease patients hold most immunosuppressive (IS) medications before and after joint replacement surgery, to prevent infections and other complications. But there are currently no guidelines on peri-arthroscopic management of IS treatment in this population. The purpose of this study is to characterize the rheumatic disease patient population undergoing arthroscopy, compare the incidence of postoperative complications among patients who either remained on IS perioperatively, held IS perioperatively or were not on IS at baseline, and compare the incidence of postoperative complication by rheumatic disease type, medication type, and procedure.
Methods: We conducted a retrospective review of all arthroscopic sports medicine surgeries in patients with a rheumatic disease diagnosis at our institution over an 11-year period. Patients on IS at baseline were grouped into those who remained on IS perioperatively or held all IS before the date of their surgery. These two groups were compared to rheumatic disease patients who were not on IS at baseline. Incidence of postoperative complications was calculated for the three cohorts and by medication class, rheumatic disease type, and procedure risk. Analysis of variance (ANOVA), Chi-squared, and Fisher's exact tests were used to determine the statistical significance of between-group differences in postoperative complication incidence.
Results: We identified 1,316 rheumatic disease patients undergoing arthroscopy, with 214 of them taking IS medications at baseline. Overall, 8.4% (n=110) remained on IS perioperatively, 7.9% (n=104) held IS perioperatively, and 83.7% (n=1102) were not on IS at baseline. In all cohorts, 7 patients experienced postoperative complications, with 6 of the 7 due to infections. There were two cases (1.82%) of infections among patients remaining on IS perioperatively, zero cases (0%) of infection in patients who held all IS, and four cases (0.36%) of postoperative infection in patients who were not on any IS at baseline. There was no statistically significant difference in postoperative infections or complication rates among the three cohorts or further subgroups.
Conclusion: Physicians and surgeons will increasingly be faced with challenging perioperative management decisions regarding IS in their rheumatic disease patients undergoing arthroscopic surgery. The present study is the first to suggest a low and acceptable risk of postoperative infections and other complications in these patients on IS at the time of arthroscopy.
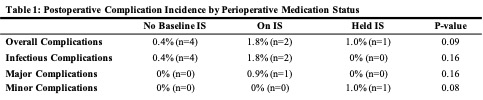 Table 1. Postoperative Complication Incidence by Perioperative Medication Status
Table 1. Postoperative Complication Incidence by Perioperative Medication Status
Disclosures: K. Vasvada, None; L. Jazrawi, Smith and nephew INC., Arthrex Sports Medicine Fellowship, Mitex Sports Medicine Fellowship; J. Samuels, None.
Background/Purpose: Recent literature suggests that rheumatic disease patients hold most immunosuppressive (IS) medications before and after joint replacement surgery, to prevent infections and other complications. But there are currently no guidelines on peri-arthroscopic management of IS treatment in this population. The purpose of this study is to characterize the rheumatic disease patient population undergoing arthroscopy, compare the incidence of postoperative complications among patients who either remained on IS perioperatively, held IS perioperatively or were not on IS at baseline, and compare the incidence of postoperative complication by rheumatic disease type, medication type, and procedure.
Methods: We conducted a retrospective review of all arthroscopic sports medicine surgeries in patients with a rheumatic disease diagnosis at our institution over an 11-year period. Patients on IS at baseline were grouped into those who remained on IS perioperatively or held all IS before the date of their surgery. These two groups were compared to rheumatic disease patients who were not on IS at baseline. Incidence of postoperative complications was calculated for the three cohorts and by medication class, rheumatic disease type, and procedure risk. Analysis of variance (ANOVA), Chi-squared, and Fisher's exact tests were used to determine the statistical significance of between-group differences in postoperative complication incidence.
Results: We identified 1,316 rheumatic disease patients undergoing arthroscopy, with 214 of them taking IS medications at baseline. Overall, 8.4% (n=110) remained on IS perioperatively, 7.9% (n=104) held IS perioperatively, and 83.7% (n=1102) were not on IS at baseline. In all cohorts, 7 patients experienced postoperative complications, with 6 of the 7 due to infections. There were two cases (1.82%) of infections among patients remaining on IS perioperatively, zero cases (0%) of infection in patients who held all IS, and four cases (0.36%) of postoperative infection in patients who were not on any IS at baseline. There was no statistically significant difference in postoperative infections or complication rates among the three cohorts or further subgroups.
Conclusion: Physicians and surgeons will increasingly be faced with challenging perioperative management decisions regarding IS in their rheumatic disease patients undergoing arthroscopic surgery. The present study is the first to suggest a low and acceptable risk of postoperative infections and other complications in these patients on IS at the time of arthroscopy.
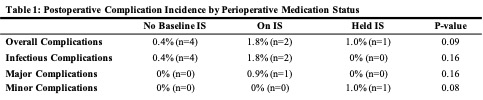 Table 1. Postoperative Complication Incidence by Perioperative Medication Status
Table 1. Postoperative Complication Incidence by Perioperative Medication StatusDisclosures: K. Vasvada, None; L. Jazrawi, Smith and nephew INC., Arthrex Sports Medicine Fellowship, Mitex Sports Medicine Fellowship; J. Samuels, None.

