Back
Poster Session B
Juvenile idiopathic arthritis (JIA) and pediatric joint disorders
Session: (0850–0880) Pediatric Rheumatology – Clinical Poster I: JIA
0858: Predicting the Occurrence of Drug-Free Inactive Disease Two Years After Diagnosis of Non-Systemic Juvenile Idiopathic Arthritis
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- MM
Melissa Mannion, MD
University of Alabama at Birmingham
Birmingham, AL, United States
Abstract Poster Presenter(s)
Melissa Mannion1, Chen Chen2, Olha Halyabar3, Susan Paetkau4, Tingting Qiu5 and Bin Huang6, 1University of Alabama at Birmingham, Birmingham, AL, 2Cincinnati Children's Hospital Medical Center, Taipei, Taiwan, 3Children's Hospital/Boston Medical Center, Boston, MA, 4The Hospital for Sick Children, Toronto, ON, Canada, 5Cincinnati Children's Hospital Medical Center, Cincinnati, OH, 6Cincinnati Children's Hospital Medical Center, Cinciannati, OH
Background/Purpose: The goal of treatment for juvenile idiopathic arthritis (JIA) is inactive disease (ID), but the optimal treatment for each patient to maximize ID and minimize overtreatment is unknown. The objective of this study was to assess if clinical measures could predict the onset of ID or drug-free inactive disease (DFID) within 2 years of diagnosis of non-systemic JIA.
Methods: Using an inception cohort from a large pediatric rheumatology clinic in the US from 2009 to 2020, we identified patients with non-systemic JIA in the electronic health record (EHR) with ≥2 clinical visits and ≥2 years of follow up following diagnosis. JIA category at baseline is reported; oligoarticular (oligo), rheumatoid factor (RF) - polyarticular (poly), RF+ poly, and all other non-systemic. A published model was used to calculate probability of severe disease course (1). Medications were classified into systemic corticosteroids, non-biologic (nb) disease modifying anti-rheumatic drug (DMARD), biologic (b) DMARD, and intra-articular corticosteroid injections. ID was defined as no active joint count (AJC), no enthesitis, no active uveitis, and physician global (PGA) < 1. Relative change in disease activity in the 3 months following diagnosis was reported by the treating physician. Descriptive statistics and Kaplan-Meier curves for time to ID and DFID were calculated based on baseline characteristics. Cox Proportional hazard (CoxPH) modeling was used to evaluate the effect of baseline characteristics and initial medication use (1st year) on onset of ID and DFID. The bivariate relationship between time to ID and covariates were plotted by individual patient in a heatmap.
Results: 605 patients with JIA were included (Table 1). By 1(2) years post diagnosis, 52(73)% and 28(42)% achieved ID and DFID respectively. Time to 1st ID or DFID is significantly different (Log-rank test P=0.001 for ID; P< .0001 for DFID) by category; median (95% CI) time to ID and DFID in oligo 0.76 years (0.63, 0.90), 1.65 (1.08, 2.24), RF- poly 1.23 (1.01, 1.49), 5.04 (3.21, 7.83), RF+ poly 1.36 (0.63, 2.79), >2.22, and other types 0.90 (0.73, 1.17), 2.88 (1.99, 4.68). Of 30 RF+ poly patients only 10 achieved DFID, the median time to DFID could not be estimated. JIA category was not significant in multivariable CoxPH analyses, but lower cJADAS, shorter time from symptoms to diagnosis, improvement at the second visit, and private insurance were significantly associated with sooner time to ID (Table 2). Less DMARD use (b and nb) was associated with sooner DFID, but more bDMARD use was associated with sooner ID.
Conclusion: In the two years after diagnosis, 73% of JIA patients achieved ID and 42% achieved DFID. There are disease characteristics associated with sooner time to ID and DFID, but further research is needed to predict medication needs for patients with JIA.
1. Guzman J, Henrey A, Loughin T, Berard RA, Shiff NJ, Jurencak R, et al. Predicting Which Children with Juvenile Idiopathic Arthritis Will Not Attain Early Remission with Conventional Treatment: Results from the ReACCh-Out Cohort. J Rheumatol. 2019;46(6):628-35.
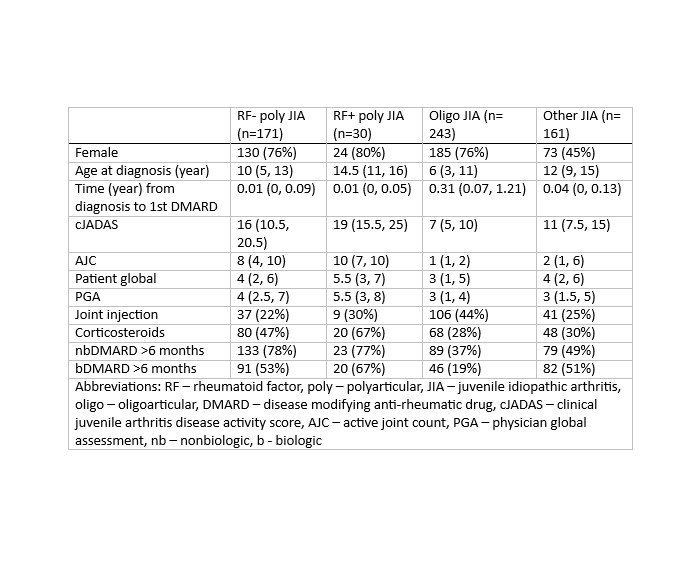 Table 1: Patient and disease characteristics at the time of diagnosis and medication use in the 12 months following diagnosis stratified by JIA category. Values are median (IQR) or n (%). All p-values < 0.0001
Table 1: Patient and disease characteristics at the time of diagnosis and medication use in the 12 months following diagnosis stratified by JIA category. Values are median (IQR) or n (%). All p-values < 0.0001
<img src=https://www.abstractscorecard.com/uploads/Tasks/upload/17574/QHOPTGBB-1291886-2-ANY.jpg width=440 height=542.978723404255 border=0 style=border-style: none;>
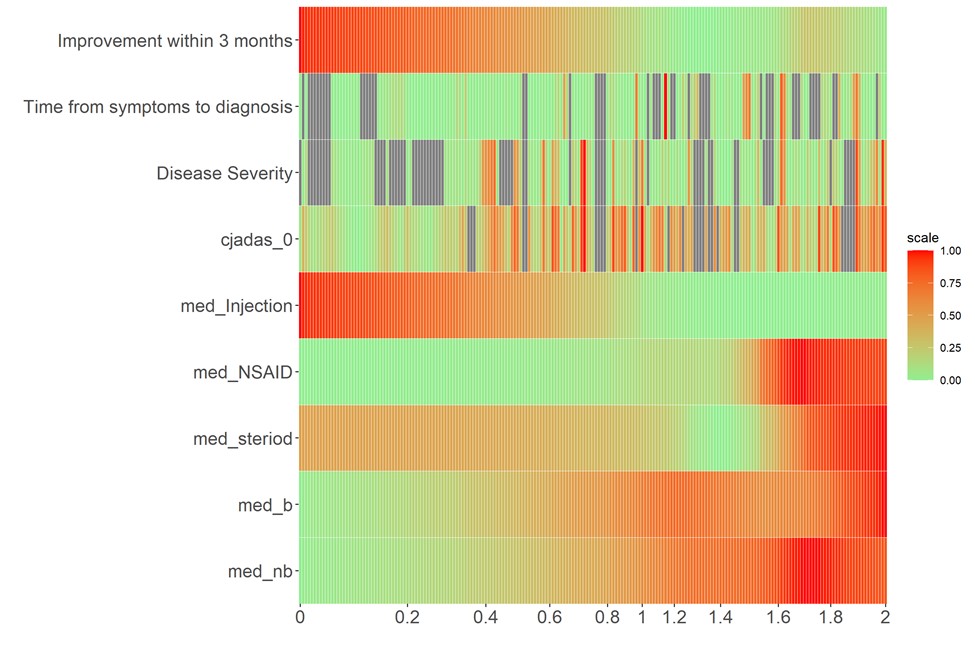 Figure 1: Heatmap of bivariate relationship between time to ID and physician impression of clinical improvement in initial 3 months following diagnosis, time from symptoms to diagnosis, probability of severe disease, initial cJADAS, and medication use in the 12 months following diagnosis.
Figure 1: Heatmap of bivariate relationship between time to ID and physician impression of clinical improvement in initial 3 months following diagnosis, time from symptoms to diagnosis, probability of severe disease, initial cJADAS, and medication use in the 12 months following diagnosis.
Disclosures: M. Mannion, None; C. Chen, None; O. Halyabar, None; S. Paetkau, None; T. Qiu, None; B. Huang, None.
Background/Purpose: The goal of treatment for juvenile idiopathic arthritis (JIA) is inactive disease (ID), but the optimal treatment for each patient to maximize ID and minimize overtreatment is unknown. The objective of this study was to assess if clinical measures could predict the onset of ID or drug-free inactive disease (DFID) within 2 years of diagnosis of non-systemic JIA.
Methods: Using an inception cohort from a large pediatric rheumatology clinic in the US from 2009 to 2020, we identified patients with non-systemic JIA in the electronic health record (EHR) with ≥2 clinical visits and ≥2 years of follow up following diagnosis. JIA category at baseline is reported; oligoarticular (oligo), rheumatoid factor (RF) - polyarticular (poly), RF+ poly, and all other non-systemic. A published model was used to calculate probability of severe disease course (1). Medications were classified into systemic corticosteroids, non-biologic (nb) disease modifying anti-rheumatic drug (DMARD), biologic (b) DMARD, and intra-articular corticosteroid injections. ID was defined as no active joint count (AJC), no enthesitis, no active uveitis, and physician global (PGA) < 1. Relative change in disease activity in the 3 months following diagnosis was reported by the treating physician. Descriptive statistics and Kaplan-Meier curves for time to ID and DFID were calculated based on baseline characteristics. Cox Proportional hazard (CoxPH) modeling was used to evaluate the effect of baseline characteristics and initial medication use (1st year) on onset of ID and DFID. The bivariate relationship between time to ID and covariates were plotted by individual patient in a heatmap.
Results: 605 patients with JIA were included (Table 1). By 1(2) years post diagnosis, 52(73)% and 28(42)% achieved ID and DFID respectively. Time to 1st ID or DFID is significantly different (Log-rank test P=0.001 for ID; P< .0001 for DFID) by category; median (95% CI) time to ID and DFID in oligo 0.76 years (0.63, 0.90), 1.65 (1.08, 2.24), RF- poly 1.23 (1.01, 1.49), 5.04 (3.21, 7.83), RF+ poly 1.36 (0.63, 2.79), >2.22, and other types 0.90 (0.73, 1.17), 2.88 (1.99, 4.68). Of 30 RF+ poly patients only 10 achieved DFID, the median time to DFID could not be estimated. JIA category was not significant in multivariable CoxPH analyses, but lower cJADAS, shorter time from symptoms to diagnosis, improvement at the second visit, and private insurance were significantly associated with sooner time to ID (Table 2). Less DMARD use (b and nb) was associated with sooner DFID, but more bDMARD use was associated with sooner ID.
Conclusion: In the two years after diagnosis, 73% of JIA patients achieved ID and 42% achieved DFID. There are disease characteristics associated with sooner time to ID and DFID, but further research is needed to predict medication needs for patients with JIA.
1. Guzman J, Henrey A, Loughin T, Berard RA, Shiff NJ, Jurencak R, et al. Predicting Which Children with Juvenile Idiopathic Arthritis Will Not Attain Early Remission with Conventional Treatment: Results from the ReACCh-Out Cohort. J Rheumatol. 2019;46(6):628-35.
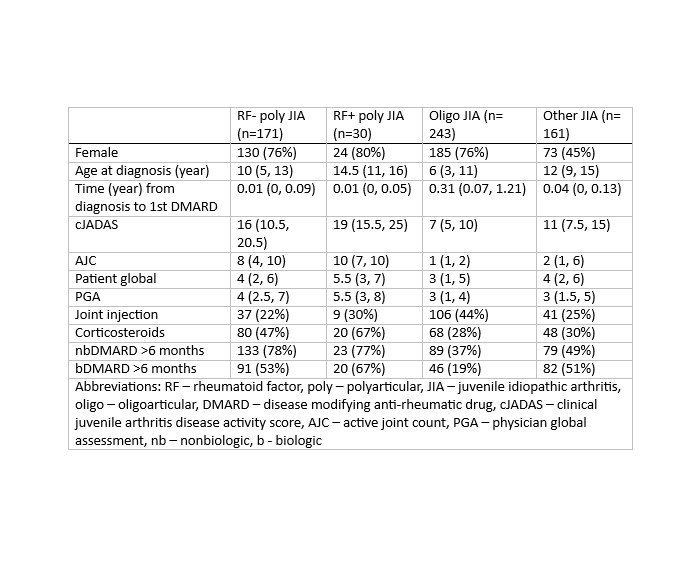 Table 1: Patient and disease characteristics at the time of diagnosis and medication use in the 12 months following diagnosis stratified by JIA category. Values are median (IQR) or n (%). All p-values < 0.0001
Table 1: Patient and disease characteristics at the time of diagnosis and medication use in the 12 months following diagnosis stratified by JIA category. Values are median (IQR) or n (%). All p-values < 0.0001<img src=https://www.abstractscorecard.com/uploads/Tasks/upload/17574/QHOPTGBB-1291886-2-ANY.jpg width=440 height=542.978723404255 border=0 style=border-style: none;>
Table 2: Adjusted hazards ratios (HR) for the effect of baseline characteristics and medication use in the 12 months following diagnosis on time to ID or DFID. Medication use was >50% in the first year.
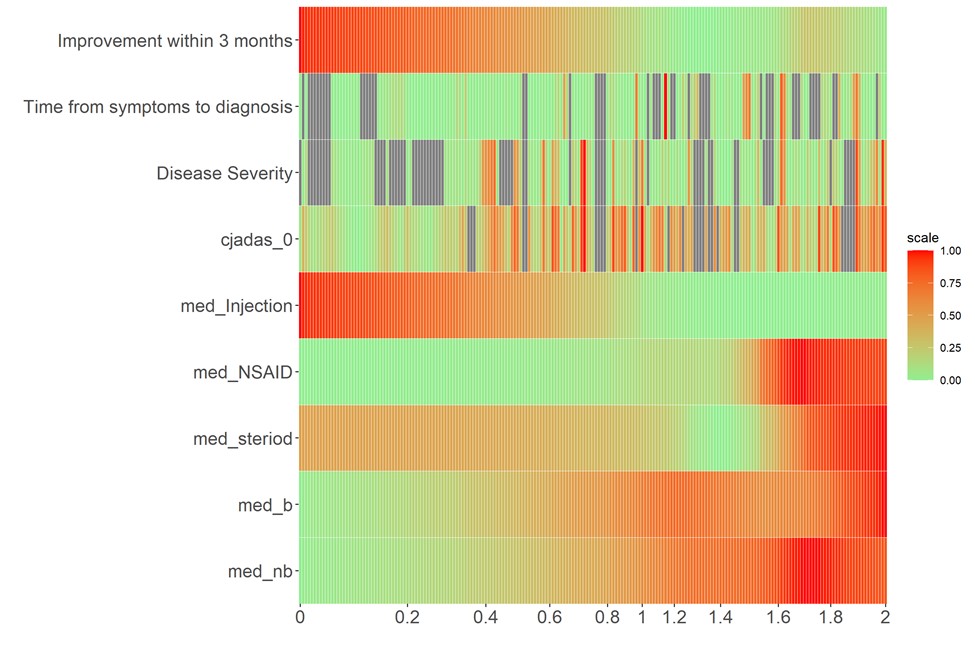 Figure 1: Heatmap of bivariate relationship between time to ID and physician impression of clinical improvement in initial 3 months following diagnosis, time from symptoms to diagnosis, probability of severe disease, initial cJADAS, and medication use in the 12 months following diagnosis.
Figure 1: Heatmap of bivariate relationship between time to ID and physician impression of clinical improvement in initial 3 months following diagnosis, time from symptoms to diagnosis, probability of severe disease, initial cJADAS, and medication use in the 12 months following diagnosis. Disclosures: M. Mannion, None; C. Chen, None; O. Halyabar, None; S. Paetkau, None; T. Qiu, None; B. Huang, None.

