Back
Poster Session B
Systemic lupus erythematosus (SLE)
Session: (0974–1003) SLE – Treatment Poster II
0981: QTc Prolongation in Rheumatoid Arthritis and Systemic Lupus Erythematosus Patients Treated with Hydroxychloroquine - Preliminary Results from a Single Center Study
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- TB
Tanmayee Bichile, MD
Allegheny Health Network
Gibsonia, PA, United States
Abstract Poster Presenter(s)
Tanmayee Bichile1, Susan Manzi2 and Tarun Sharma3, 1Allegheny Health Network, Gibsonia, PA, 2Allegheny Health Network, Lupus Center of Excellence, Wexford, PA, 3Allegheny Health Network, Pittsburgh, PA
Background/Purpose: The effect of hydroxychloroquine (HCQ) on QTc interval in patients with rheumatic diseases is under scrutiny since the COVID-19 pandemic, however studies have shown conflicting data.The aim of this study is to investigate the effect of HCQ on QTc prolongation in SLE and RA patients.
Methods: A retrospective cohort of adult patients with SLE and RA was constructed from December 1, 2014 to September 30, 2020 using electronic health records (EHR). RA was defined as ICD 10 codes M05 or M06 and SLE defined as ICD10 M35 by a rheumatologist during the study period. Patients were categorized as HCQ users or nonusers and had at least one EKG during the study period with reported QTc interval. The primary outcome was incidence of QTc prolongation defined as ≥450ms based on the Heart Rhythm Society guidelines. We analyzed data using Chi square test to estimate risk of QTc prolongation among HCQ users and nonusers.
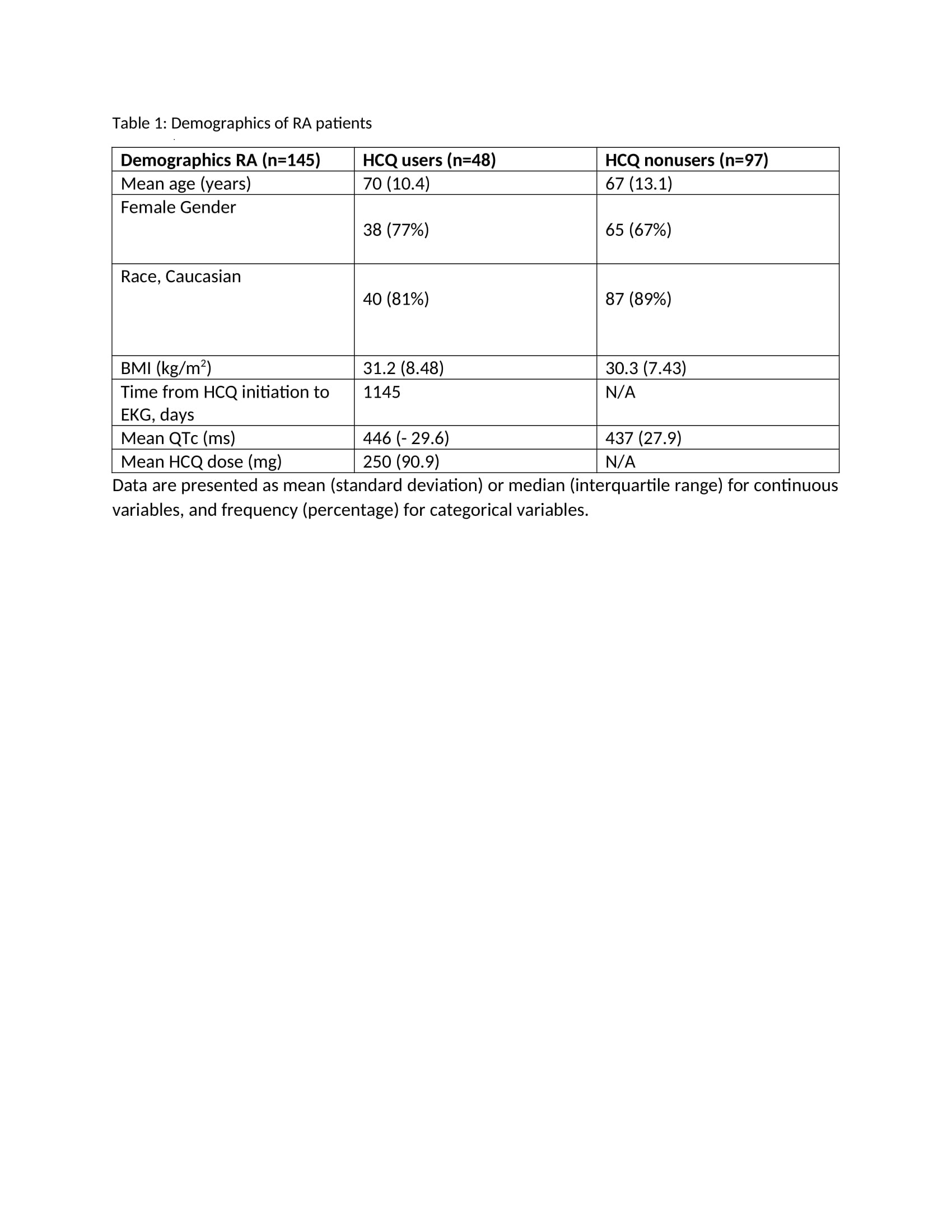
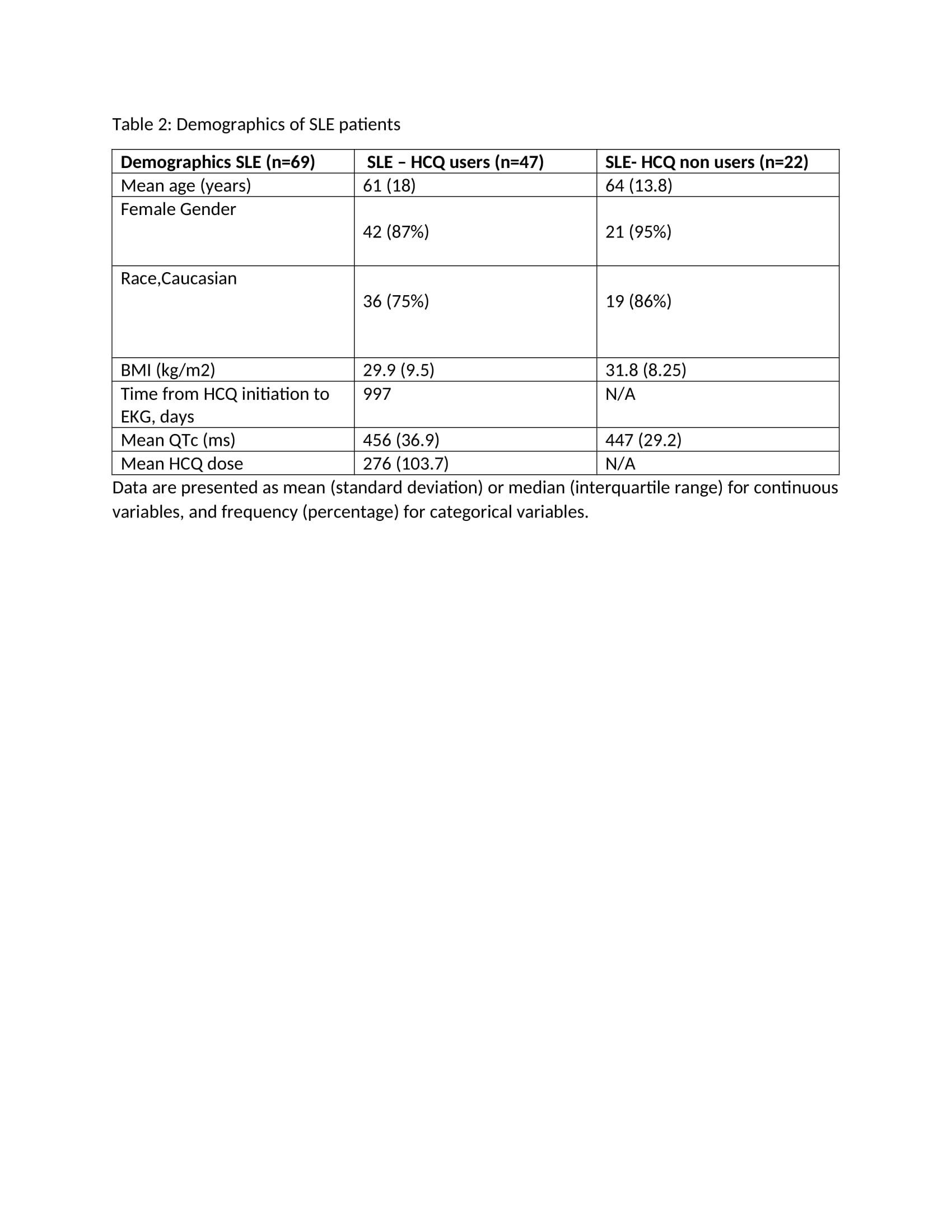
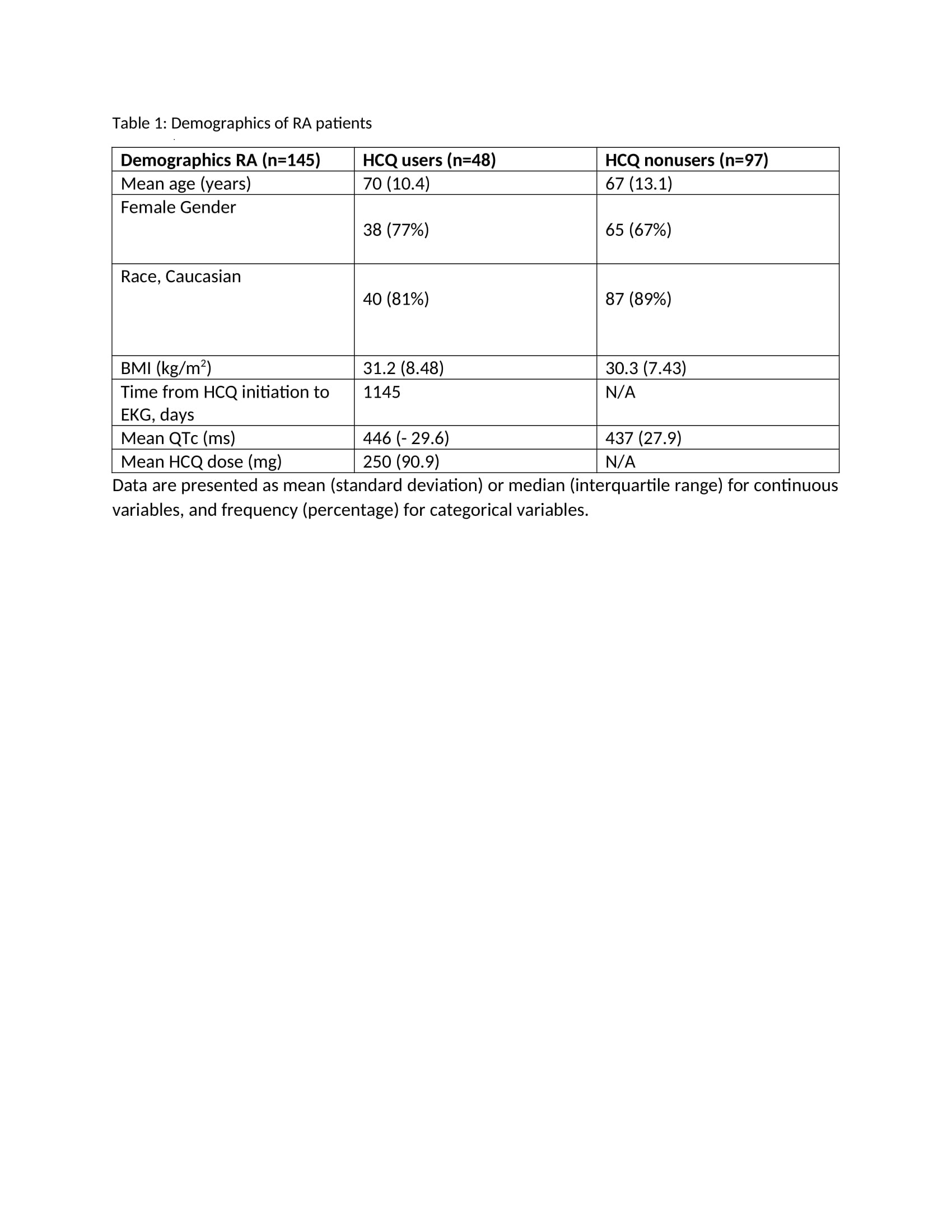
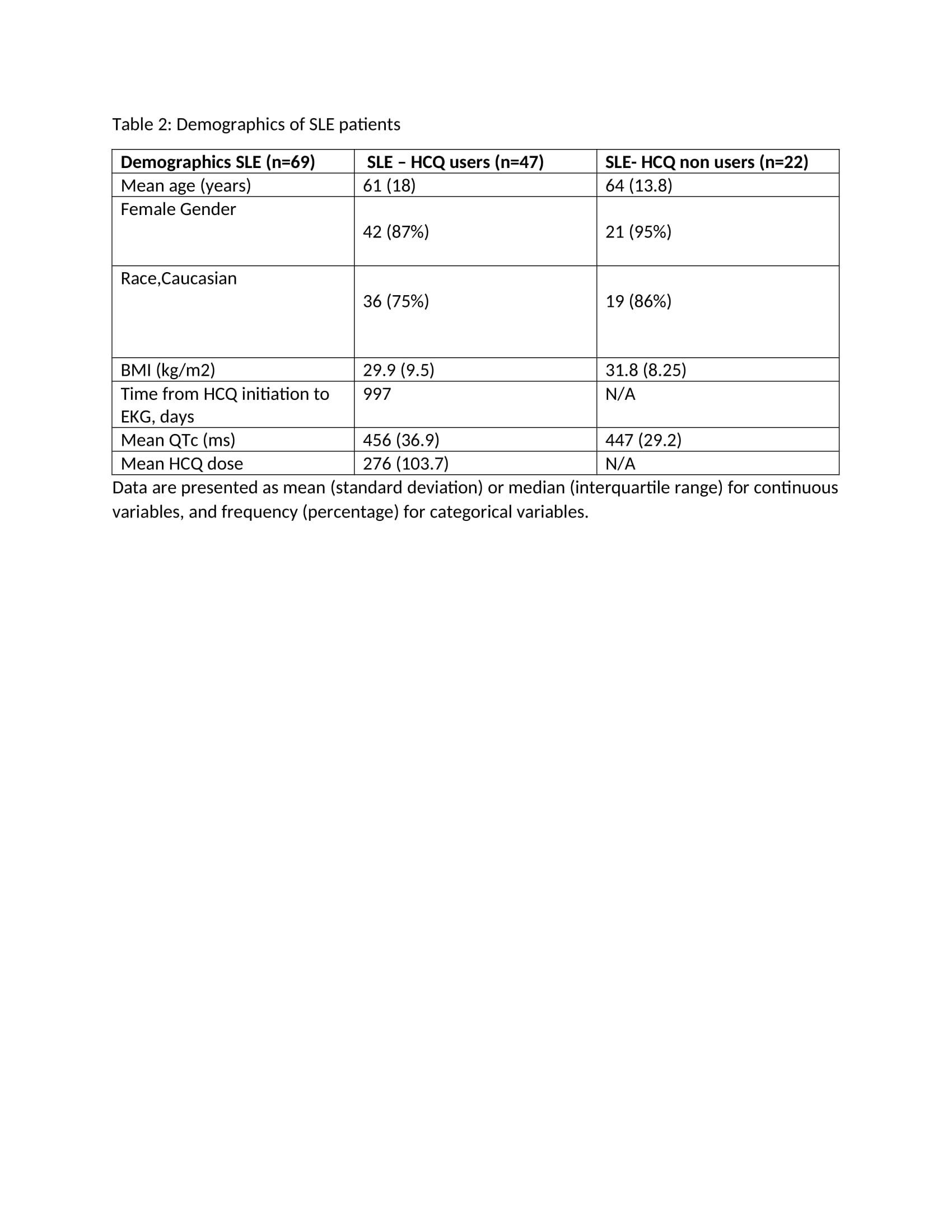
Results: The study included 145 patients with RA and QTc data, of which 48 were HCQ users (33%) and 97 were nonusers (67%). There were 69 patients with SLE and QTc data, of which 47 were HCQ users (68%) and 22 were nonusers (32%). Majority of the study population was Caucasian and female. The mean HCQ dose in users with RA was 250mg, and in users with SLE was 276mg. The mean QTc in RA users was 446ms as compared to 437ms in nonusers. The mean QTc in SLE users was 456ms as compared to 447ms in nonusers. Table 1 and 2 highlight the demographics of our study population.
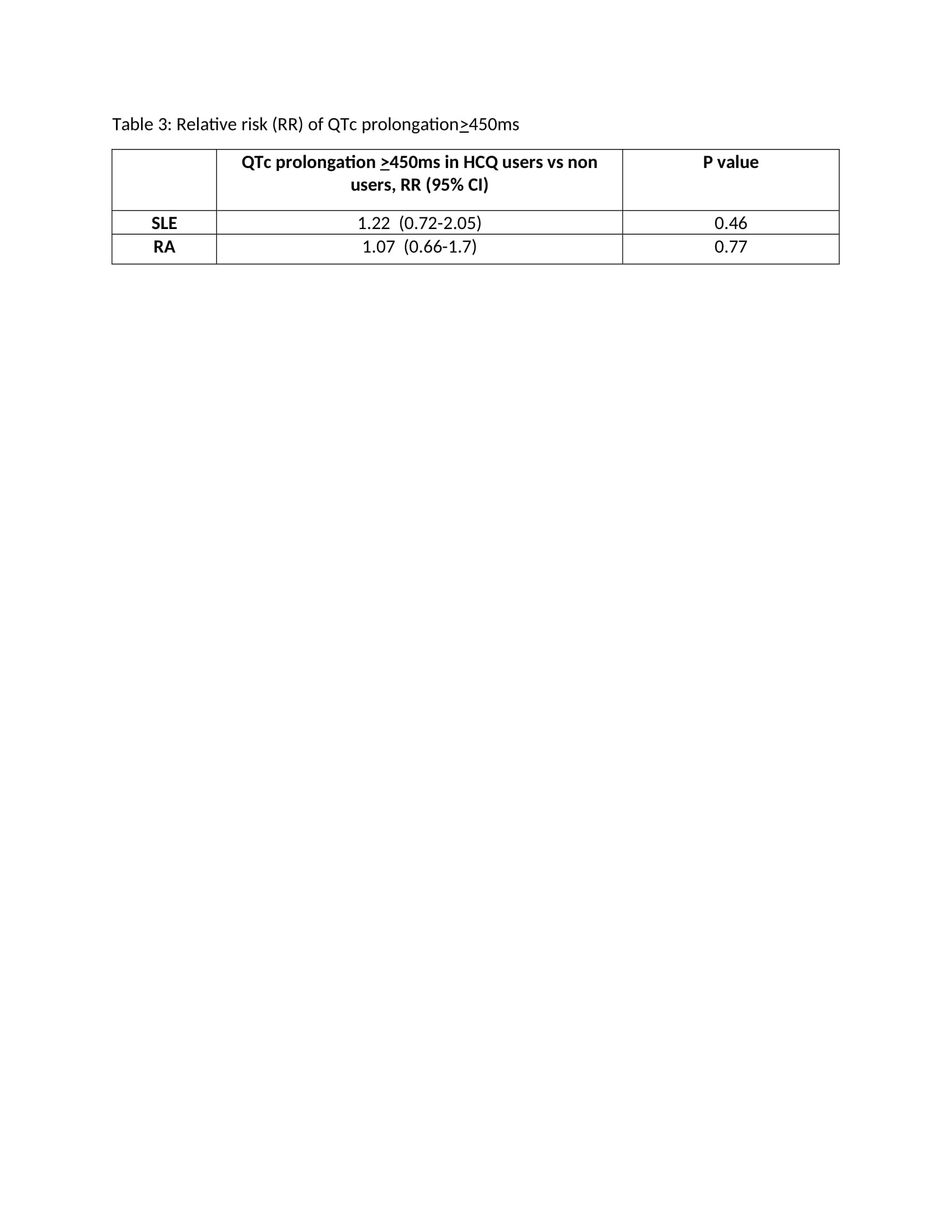
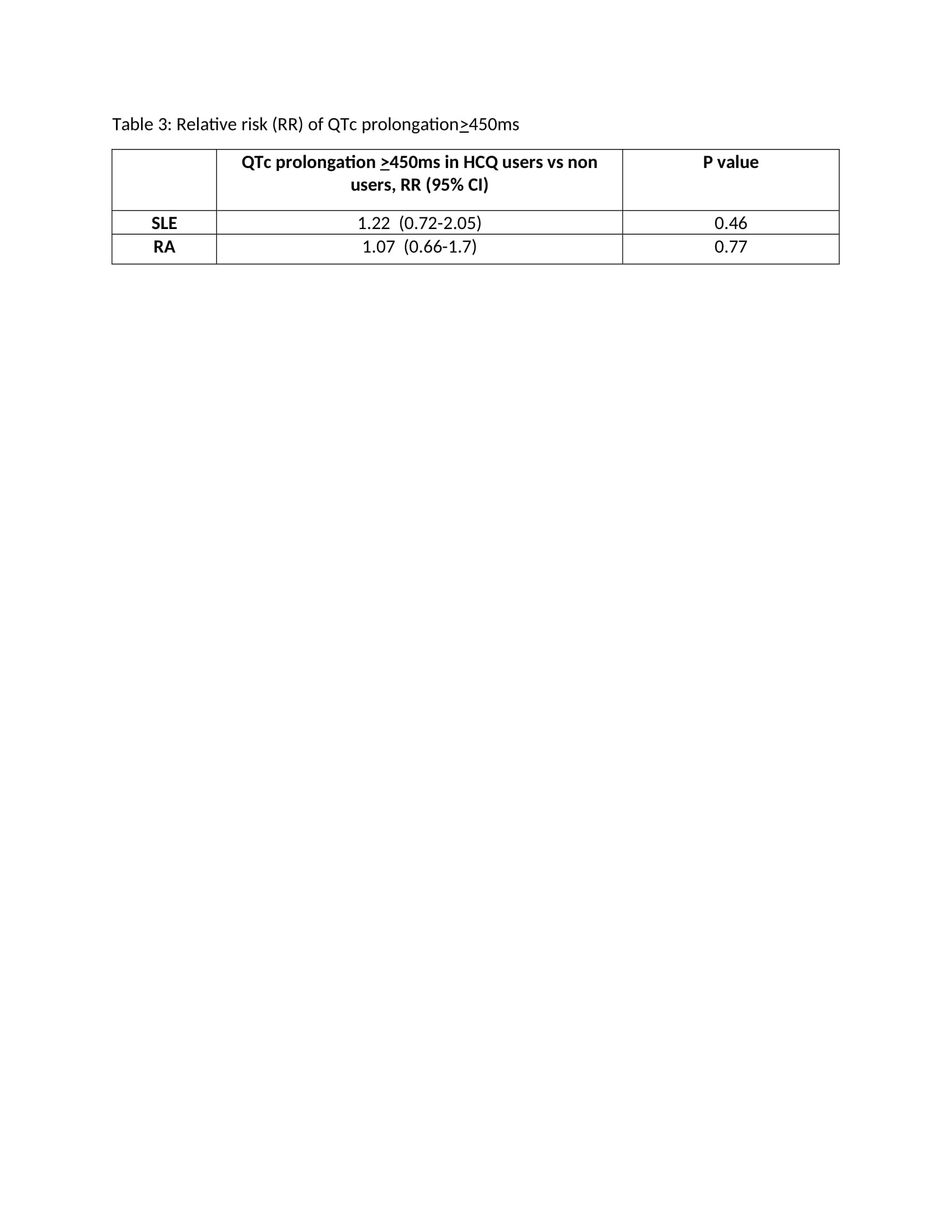
35% RA and 55% SLE HCQ users had prolonged QTc ( >450ms). The statistical analyses was unadjusted and showed an increased but non-significant risk of QTC prolongation among HCQ users in SLE and RA. Table 3 highlights the relative risk of QTc prolongation in HCQ users in SLE and RA.
Conclusion: In this exploratory study, we observed an increased but non-significant risk of QTc prolongation associated with HCQ use in SLE and RA. Given the known longevity of HCQ use and overall higher risk of arrhythmias in patients with chronic SLE and RA, this finding could be consequential if confirmed if larger studies. As next steps, we plan to expand our cohort and perform a multivariable regression analysis including covariates such as other medications that prolong QTc, electrolytes, and manually validating the QTc values.
Disclosures: T. Bichile, None; S. Manzi, AstraZeneca, GlaxoSmithKline (GSK), Exagen Diagnostics Inc, AbbVie, HGS, Cugene, Lilly, UCB Advisory Board, Lupus Foundation of America; T. Sharma, None.
Background/Purpose: The effect of hydroxychloroquine (HCQ) on QTc interval in patients with rheumatic diseases is under scrutiny since the COVID-19 pandemic, however studies have shown conflicting data.The aim of this study is to investigate the effect of HCQ on QTc prolongation in SLE and RA patients.
Methods: A retrospective cohort of adult patients with SLE and RA was constructed from December 1, 2014 to September 30, 2020 using electronic health records (EHR). RA was defined as ICD 10 codes M05 or M06 and SLE defined as ICD10 M35 by a rheumatologist during the study period. Patients were categorized as HCQ users or nonusers and had at least one EKG during the study period with reported QTc interval. The primary outcome was incidence of QTc prolongation defined as ≥450ms based on the Heart Rhythm Society guidelines. We analyzed data using Chi square test to estimate risk of QTc prolongation among HCQ users and nonusers.
Results: The study included 145 patients with RA and QTc data, of which 48 were HCQ users (33%) and 97 were nonusers (67%). There were 69 patients with SLE and QTc data, of which 47 were HCQ users (68%) and 22 were nonusers (32%). Majority of the study population was Caucasian and female. The mean HCQ dose in users with RA was 250mg, and in users with SLE was 276mg. The mean QTc in RA users was 446ms as compared to 437ms in nonusers. The mean QTc in SLE users was 456ms as compared to 447ms in nonusers. Table 1 and 2 highlight the demographics of our study population.
35% RA and 55% SLE HCQ users had prolonged QTc ( >450ms). The statistical analyses was unadjusted and showed an increased but non-significant risk of QTC prolongation among HCQ users in SLE and RA. Table 3 highlights the relative risk of QTc prolongation in HCQ users in SLE and RA.
Conclusion: In this exploratory study, we observed an increased but non-significant risk of QTc prolongation associated with HCQ use in SLE and RA. Given the known longevity of HCQ use and overall higher risk of arrhythmias in patients with chronic SLE and RA, this finding could be consequential if confirmed if larger studies. As next steps, we plan to expand our cohort and perform a multivariable regression analysis including covariates such as other medications that prolong QTc, electrolytes, and manually validating the QTc values.
Disclosures: T. Bichile, None; S. Manzi, AstraZeneca, GlaxoSmithKline (GSK), Exagen Diagnostics Inc, AbbVie, HGS, Cugene, Lilly, UCB Advisory Board, Lupus Foundation of America; T. Sharma, None.

