Back
Abstract Session
Session: Abstracts: Antiphospholipid Syndrome (2268–2271)
2269: Anti-NET Antibodies in Antiphospholipid Antibody-positive Patients: Results from the Antiphospholipid Syndrome Alliance for Clinical Trials and InternatiOnal Networking (APS ACTION) Clinical Database and Repository (“Registry”)
Monday, November 14, 2022
5:15 PM – 5:20 PM Eastern Time
Location: Room 119
- YZ
Yu (Ray) Zuo, MD, MS
University of Michigan
Ann Arbor, MI, United States
Presenting Author(s)
Yu (Ray) Zuo1, Sherwin Navaz1, Alex Tsodikov1, Katarina Kmetova2, Claire Hoy1, Srilakshmi Yalavarthi1, Danieli Castro Oliveira de Andrade3, Maria G. Tektonidou4, Savino Sciascia5, Vittorio Pengo6, Guillermo Ruiz-Irastorza7, H Michael Belmont8, maria gerosa9, Paul fortin10, Guilherme de Jesús11, D. Ware Branch12, Laura Andreoli13, Esther Rodriguez Almaraz14, Michelle Petri15, Ricard Cervera16, Rohan Willis17, Doruk Erkan18 and Jason S Knight19, 1University of Michigan, Ann Arbor, MI, 2Division of Rheumatology, University of Michigan, Ann Arbor, MI, 3Hospital das Clinicas HCFMUSP, Faculdade de Medicina, Universidade de São Paulo, São Paulo, Brazil, 4National and Kapodistrian University of Athens, Athens, Greece, 5University of Turin, Torino, Italy, 6Padova University Hospital, Padova, Italy, 7Autoimmune Diseases Research Unit, Biocruces Bizkaia Health Research Institute, Hospital Universitario Cruces, UPV/EHU, Barakaldo, Spain, 8NYU School of Medicine, New York, NY, 9University of Milan, Milano, Italy, 10CHU de Québec, Pavillon CHUL, Québec, Canada, 11Universidade do Estado do Rio de Janeiro, Rio De Janeiro, Brazil, 12University of Utah, Salt Lake City, UT, 13Rheumatology and Clinical Immunology Unit, ASST Spedali Civili and University of Brescia, Brescia, Italy, 14Hospital Universitario 12 de Octubre, Madrid, Spain, 15Johns Hopkins University School of Medicine, Division of Rheumatology, Baltimore, MD, 16Hospital Clínic de Barcelona, Barcelona, Spain, 17University of Texas Medical Branch, Galveston, TX, 18Hospital for Special Surgery, New York, NY, 19University of Michigan, Division of Rheumatology, Ann Arbor, MI
Background/Purpose: The release of neutrophil extracellular traps (NETs) by hyperactive neutrophils plays a role in the thromboinflammatory phenotype of APS. Previous work has demonstrated that some patients with APS have autoantibodies targeting NETs, which impair NET clearance and potentially activate complement. Here, we aimed to elucidate the presence, clinical associations, and antigen specificities of anti-NET antibodies in a large, ethnically diverse cohort of antiphospholipid antibody (aPL)-positive patients who did not have lupus.
Methods: Levels of anti-NET IgG/IgM were determined in sera of 308 patients with primary APS and 81 patients who were aPL positive but without "criteria" APS manifestations or other systemic autoimmune disease diagnosis. A positive cut-off for anti-NET level was established at the 99th percentile optical density of healthy-control samples. Multivariate logistic regression with best variable model selection was used to determine clinical associations. For a subset of patients (n=214), we profiled autoantibodies with a microarray platform that included 120 potential autoantigens (66 associated with NETs based on literature mining).
Results: We found elevated levels of anti-NET IgG or IgM in 45% of aPL-positive patients, whether they met criteria for primary APS or not (Figure 1A-B). There was a strong relationship between anti-NET IgG and anti-NET IgM (r=0.52, p< 0.0001). High anti-NET antibody levels correlated with a circulating marker of NETs, myeloperoxidase (MPO)-DNA complexes (IgG r=0.12, p=0.02; IgM r=0.16, p=0.001). Anti-NET activity also demonstrated a positive correlation with levels of traditional aPL (anti-beta-2 glycoprotein I IgG: r=0.21, p< 0.0001) and anticardiolipin IgG: r=0.19, p=0.0001). When considering clinical manifestations among aPL-positive patients, positive anti-NET IgG was strongly associated with brain white matter changes after adjusting for demographic variables and criteria aPL profiles (OR=11, 95% CI 1.9 to 62), but not with other aPL-related manifestations. By immunofluorescence microscopy, we determined that high anti-NET sera more efficiently deposited complement C3d on NETs. In pursuit of the antigen specificity of anti-NET antibodies, 214 samples were analyzed by autoantibody microarray. Anti-NET IgG positivity significantly associated with the following antigens: citrullinated-histone H1 and H4, MPO-DNA complexes, nucleosomes, centromere protein A (a histone H3 variant), heparan sulfate proteoglycan, laminin, and collagen VI. Meanwhile, anti-NET IgM positivity associated with the following: single-stranded DNA, double-stranded DNA, and proliferating cell nuclear antigen.
Conclusion: In summary, these data reveal high levels of anti-NET antibodies in 45% of aPL-positive patients wherein they potentially activate the complement cascade and contribute to white matter changes. While anti-NET IgM may especially target DNA in NETs, anti-NET IgG appear more likely to target protein antigens.
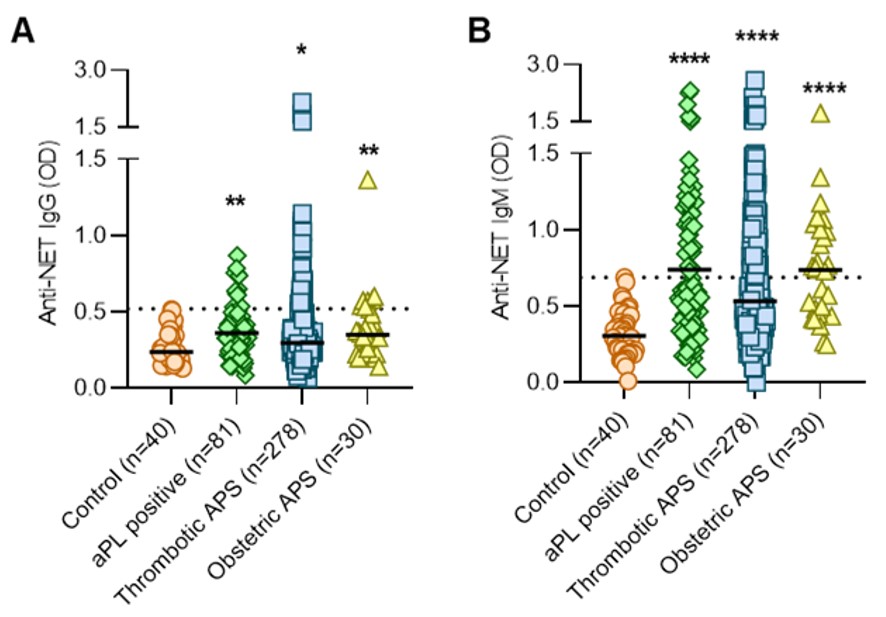 Figure 1. A-B, Anti-NET IgG and IgM were measured in the indicated groups; no patients in this cohort had lupus. As compared with healthy controls, high levels of anti-NET IgG and IgM were found in aPL-positive patients with no criteria manifestations (“aPL positive”), thrombotic manifestations, or obstetric manifestations. Levels of anti-NET IgG and IgM at 450-nm optical density (OD) were compared to Control by Kruskal–Wallis test corrected for multiple comparisons by Dunn’s method; *p < 0.05, **p < 0.01, and ****p < 0.0001. Horizontal black lines indicate medians and dashed lines indicate 99th percentile cut-offs.
Figure 1. A-B, Anti-NET IgG and IgM were measured in the indicated groups; no patients in this cohort had lupus. As compared with healthy controls, high levels of anti-NET IgG and IgM were found in aPL-positive patients with no criteria manifestations (“aPL positive”), thrombotic manifestations, or obstetric manifestations. Levels of anti-NET IgG and IgM at 450-nm optical density (OD) were compared to Control by Kruskal–Wallis test corrected for multiple comparisons by Dunn’s method; *p < 0.05, **p < 0.01, and ****p < 0.0001. Horizontal black lines indicate medians and dashed lines indicate 99th percentile cut-offs.
Disclosures: Y. Zuo, None; S. Navaz, None; A. Tsodikov, None; K. Kmetova, None; C. Hoy, None; S. Yalavarthi, None; D. Castro Oliveira de Andrade, None; M. Tektonidou, None; S. Sciascia, None; V. Pengo, None; G. Ruiz-Irastorza, None; H. Belmont, None; m. gerosa, None; P. fortin, None; G. de Jesús, None; D. Branch, None; L. Andreoli, GlaxoSmithKlein(GSK), Janssen, Novartis, UCB, Werfen; E. Rodriguez Almaraz, None; M. Petri, Exagen, AstraZeneca, Alexion, Amgen, AnaptysBio, Argenx, Aurinia, Biogen, Caribou Biosciences, CVS Health, EMD Serono, Eli Lilly, Emergent Biosolutions, GlaxoSmithKline (GSK), IQVIA, Janssen, Kira Pharmaceuticals, MedShr, Sanofi, SinoMab, Thermofisher, BPR Scientific Advisory Committee; R. Cervera, None; R. Willis, None; D. Erkan, None; J. Knight, Jazz Pharmaceuticals, Bristol Myers Squibb.
Background/Purpose: The release of neutrophil extracellular traps (NETs) by hyperactive neutrophils plays a role in the thromboinflammatory phenotype of APS. Previous work has demonstrated that some patients with APS have autoantibodies targeting NETs, which impair NET clearance and potentially activate complement. Here, we aimed to elucidate the presence, clinical associations, and antigen specificities of anti-NET antibodies in a large, ethnically diverse cohort of antiphospholipid antibody (aPL)-positive patients who did not have lupus.
Methods: Levels of anti-NET IgG/IgM were determined in sera of 308 patients with primary APS and 81 patients who were aPL positive but without "criteria" APS manifestations or other systemic autoimmune disease diagnosis. A positive cut-off for anti-NET level was established at the 99th percentile optical density of healthy-control samples. Multivariate logistic regression with best variable model selection was used to determine clinical associations. For a subset of patients (n=214), we profiled autoantibodies with a microarray platform that included 120 potential autoantigens (66 associated with NETs based on literature mining).
Results: We found elevated levels of anti-NET IgG or IgM in 45% of aPL-positive patients, whether they met criteria for primary APS or not (Figure 1A-B). There was a strong relationship between anti-NET IgG and anti-NET IgM (r=0.52, p< 0.0001). High anti-NET antibody levels correlated with a circulating marker of NETs, myeloperoxidase (MPO)-DNA complexes (IgG r=0.12, p=0.02; IgM r=0.16, p=0.001). Anti-NET activity also demonstrated a positive correlation with levels of traditional aPL (anti-beta-2 glycoprotein I IgG: r=0.21, p< 0.0001) and anticardiolipin IgG: r=0.19, p=0.0001). When considering clinical manifestations among aPL-positive patients, positive anti-NET IgG was strongly associated with brain white matter changes after adjusting for demographic variables and criteria aPL profiles (OR=11, 95% CI 1.9 to 62), but not with other aPL-related manifestations. By immunofluorescence microscopy, we determined that high anti-NET sera more efficiently deposited complement C3d on NETs. In pursuit of the antigen specificity of anti-NET antibodies, 214 samples were analyzed by autoantibody microarray. Anti-NET IgG positivity significantly associated with the following antigens: citrullinated-histone H1 and H4, MPO-DNA complexes, nucleosomes, centromere protein A (a histone H3 variant), heparan sulfate proteoglycan, laminin, and collagen VI. Meanwhile, anti-NET IgM positivity associated with the following: single-stranded DNA, double-stranded DNA, and proliferating cell nuclear antigen.
Conclusion: In summary, these data reveal high levels of anti-NET antibodies in 45% of aPL-positive patients wherein they potentially activate the complement cascade and contribute to white matter changes. While anti-NET IgM may especially target DNA in NETs, anti-NET IgG appear more likely to target protein antigens.
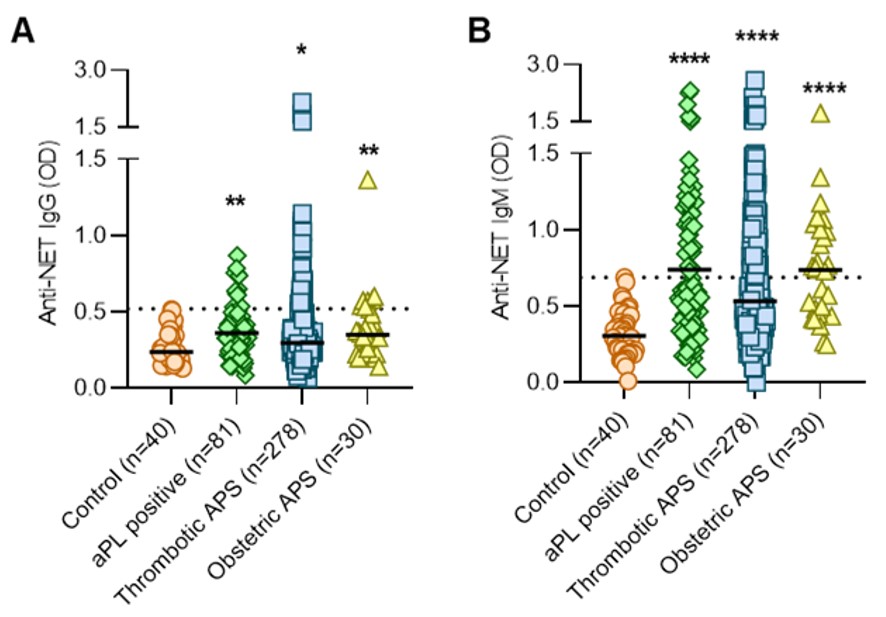 Figure 1. A-B, Anti-NET IgG and IgM were measured in the indicated groups; no patients in this cohort had lupus. As compared with healthy controls, high levels of anti-NET IgG and IgM were found in aPL-positive patients with no criteria manifestations (“aPL positive”), thrombotic manifestations, or obstetric manifestations. Levels of anti-NET IgG and IgM at 450-nm optical density (OD) were compared to Control by Kruskal–Wallis test corrected for multiple comparisons by Dunn’s method; *p < 0.05, **p < 0.01, and ****p < 0.0001. Horizontal black lines indicate medians and dashed lines indicate 99th percentile cut-offs.
Figure 1. A-B, Anti-NET IgG and IgM were measured in the indicated groups; no patients in this cohort had lupus. As compared with healthy controls, high levels of anti-NET IgG and IgM were found in aPL-positive patients with no criteria manifestations (“aPL positive”), thrombotic manifestations, or obstetric manifestations. Levels of anti-NET IgG and IgM at 450-nm optical density (OD) were compared to Control by Kruskal–Wallis test corrected for multiple comparisons by Dunn’s method; *p < 0.05, **p < 0.01, and ****p < 0.0001. Horizontal black lines indicate medians and dashed lines indicate 99th percentile cut-offs.Disclosures: Y. Zuo, None; S. Navaz, None; A. Tsodikov, None; K. Kmetova, None; C. Hoy, None; S. Yalavarthi, None; D. Castro Oliveira de Andrade, None; M. Tektonidou, None; S. Sciascia, None; V. Pengo, None; G. Ruiz-Irastorza, None; H. Belmont, None; m. gerosa, None; P. fortin, None; G. de Jesús, None; D. Branch, None; L. Andreoli, GlaxoSmithKlein(GSK), Janssen, Novartis, UCB, Werfen; E. Rodriguez Almaraz, None; M. Petri, Exagen, AstraZeneca, Alexion, Amgen, AnaptysBio, Argenx, Aurinia, Biogen, Caribou Biosciences, CVS Health, EMD Serono, Eli Lilly, Emergent Biosolutions, GlaxoSmithKline (GSK), IQVIA, Janssen, Kira Pharmaceuticals, MedShr, Sanofi, SinoMab, Thermofisher, BPR Scientific Advisory Committee; R. Cervera, None; R. Willis, None; D. Erkan, None; J. Knight, Jazz Pharmaceuticals, Bristol Myers Squibb.

