Back
Abstract Session
Session: Abstracts: Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes II: Imaging (2254–2259)
2257: MRI Spinal Lesions in Patients Without MRI or Radiographic Lesions in the Sacroiliac Joints Typical of Axial Spondyloarthritis
Monday, November 14, 2022
11:45 AM – 11:55 AM Eastern Time
Location: Room 204
- WM
Walter P. Maksymowych, MD
University of Alberta
Edmonton, AB, Canada
Presenting Author(s)
Walter P Maksymowych1, Mikkel Østergaard2, Xenofon Baraliakos3, Pedro Machado4, Susanne J. Pedersen5, Ulrich Weber6, Iris Eshed7, Manouk de Hooge8, Joachim Sieper9, Denis Poddubnyy10, Martin Rudwaleit11, Désirée van der Heijde12, Robert Landewé13 and Robert G Lambert14, 1Department of Medicine, University of Alberta, Edmonton, AB, Canada, 2Rigshospitalet, University of Copenhagen, Glostrup, Denmark, 3Rheumazentrum Ruhrgebiet Herne, Herne, Germany, 4University College London, London, United Kingdom, 5Rigshospitalet, University of Copenhagen, Copenhagen, Denmark, 6Practice Buchsbaum Schaffhausen, Schaffhausen, Switzerland, 7Sheba Medical Center, Tel Aviv, Israel, 8Ghent University Hospital, Luxembourg, Luxembourg, 9Charité - Universitätsmedizin, Berlin, Berlin, Germany, 10Department of Gastroenterology, Infectious Diseases and Rheumatology, Charité – Universitätsmedizin Berlin, Berlin, Germany, 11University of Bielefeld, Klinikum Bielefeld, Bielefeld; Germany Klinikum Bielefeld and Charité Berlin, Germany, and Gent University, Gent, Belgium, 12Department of Rheumatology, Leiden University Medical Center, Leiden, The Netherlands, Leiden, Netherlands, 13Amsterdam University Medical Center, Meerssen, Netherlands, 14University of Alberta, Edmonton, AB, Canada
Background/Purpose: There is limited data as to the frequency of spinal lesions on MRI in patients without MRI or radiographic features typical of sacroiliac joint (SIJ) disease in axial spondyloarthritis (axSpA). This may inform to what degree spine MRI might enhance the diagnostic information provided by SIJ MRI alone. We aimed to assess the frequency of MRI lesions of the spine in the ASAS-Classification Cohort according to the presence of MRI SIJ lesions typical of axSpA and/or radiographic sacroiliitis according to the modified New York criteria (mNY+).
Methods: MRI spine lesions were recorded by 9 central readers in an eCRF that captures global assessment of the spine ("Is the MRI consistent with axSpA: yes/no") (yes=MRIglobal spine+) and detailed anatomical-based scoring of each discovertebral unit plus lateral and posterior structures for bone marrow edema, fat lesions, erosion, and ankylosis, according to ASAS standardized definitions for spinal lesions. Independently, readers globally assessed SIJ scans for active and/or structural lesions typical of axSpA (MRIglobal SIJ+) . We compared the frequency of a positive MRIglobal spine+ and frequencies of different types of spinal lesions according to the presence/absence of axSpA on global evaluation of SIJ MRI scans by ≥5 of 9 readers (MRIglobal SIJ+) and according to the presence/absence of mNY+ radiographic sacroiliitis using Fisher's exact test. Analysis was also stratified by rheumatologist clinical diagnosis.
Results: Among 51 cases with SIJ as well as spine MRI scans and radiographs of the SIJ,19 (37.3%) had a positive MRIglobal SIJ+ scan, and 12 (23.5%) and 7 (13.7%) had a positive MRIglobal spine+ scan according to ≥2 and ≥5 reader agreement, respectively. A positive MRIglobal spine+ scan occurred significantly more frequently in the presence of a positive MRIglobal SIJ+ scan (Table 1) and the presence of radiographic sacroiliitis but was also recorded in 4 of 32(12.5%) (≥2 readers) and 1 of 32(3.4%) (≥5 readers) cases that were negative for a MRIglobal SIJ- scan and x-ray negative (Table 2), all 4 cases being diagnosed with axSpA. Moreover, vertebral corner BME lesions, but not spinal structural lesions, were significantly more frequent in cases that were negative for a MRIglobal SIJ- scan but had been clinically diagnosed as axSpA versus non-axSpA (Table 3).
Conclusion: Spinal lesions on MRI indicative of axSpA per majority central read occurred in about 3% of patients without positive imaging in the SIJ on either MRI or radiography. Frequency of spinal vertebral corner BME lesions was significantly higher in cases with negative SIJ imaging on either MRI or radiography but clinically diagnosed with axSpA.
.jpg) Table 1. Frequency of Spinal MRI lesions According to an MRI SIJ scan Positive for AxSpA
Table 1. Frequency of Spinal MRI lesions According to an MRI SIJ scan Positive for AxSpA
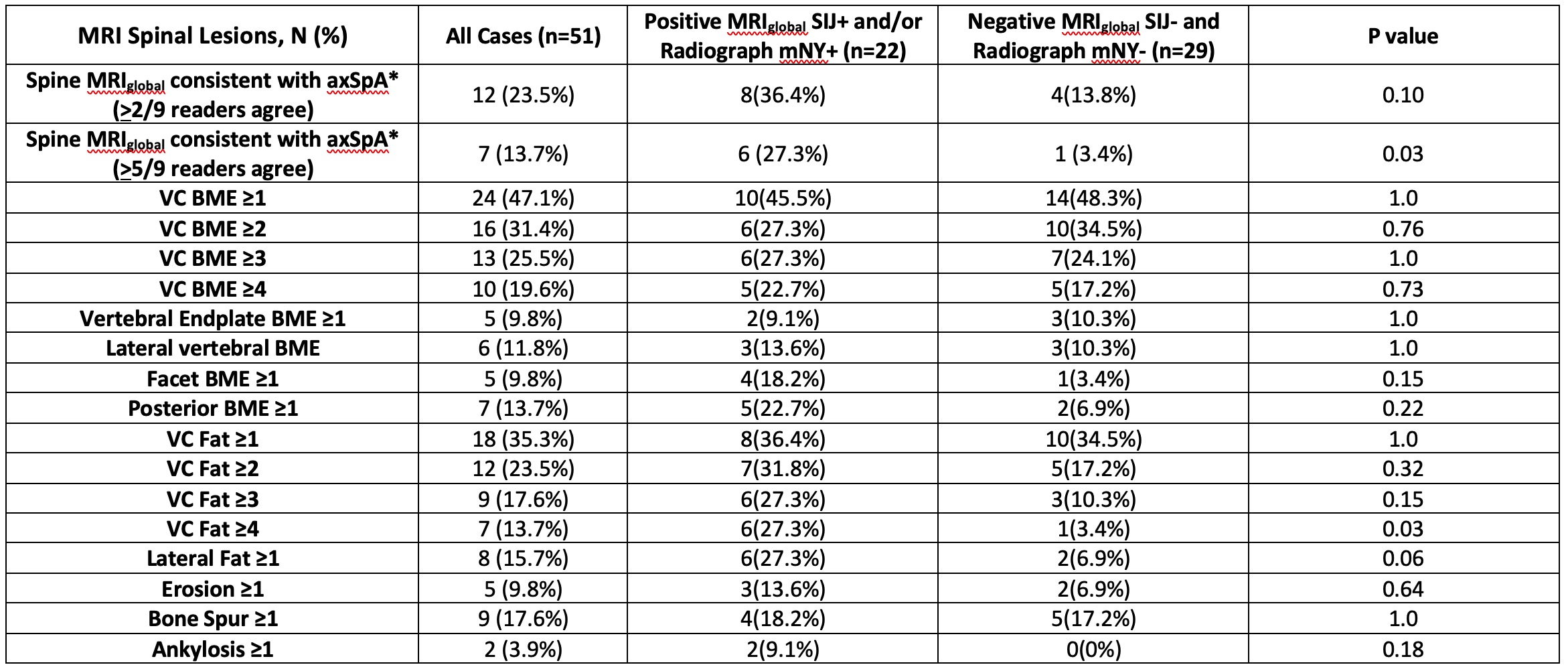 Table 2. Frequency of Spinal MRI lesions According to an MRI SIJ scan Positive for AxSpA and/or Presence/Absence of Radiographic Sacroiliitis (mNY+)
Table 2. Frequency of Spinal MRI lesions According to an MRI SIJ scan Positive for AxSpA and/or Presence/Absence of Radiographic Sacroiliitis (mNY+)
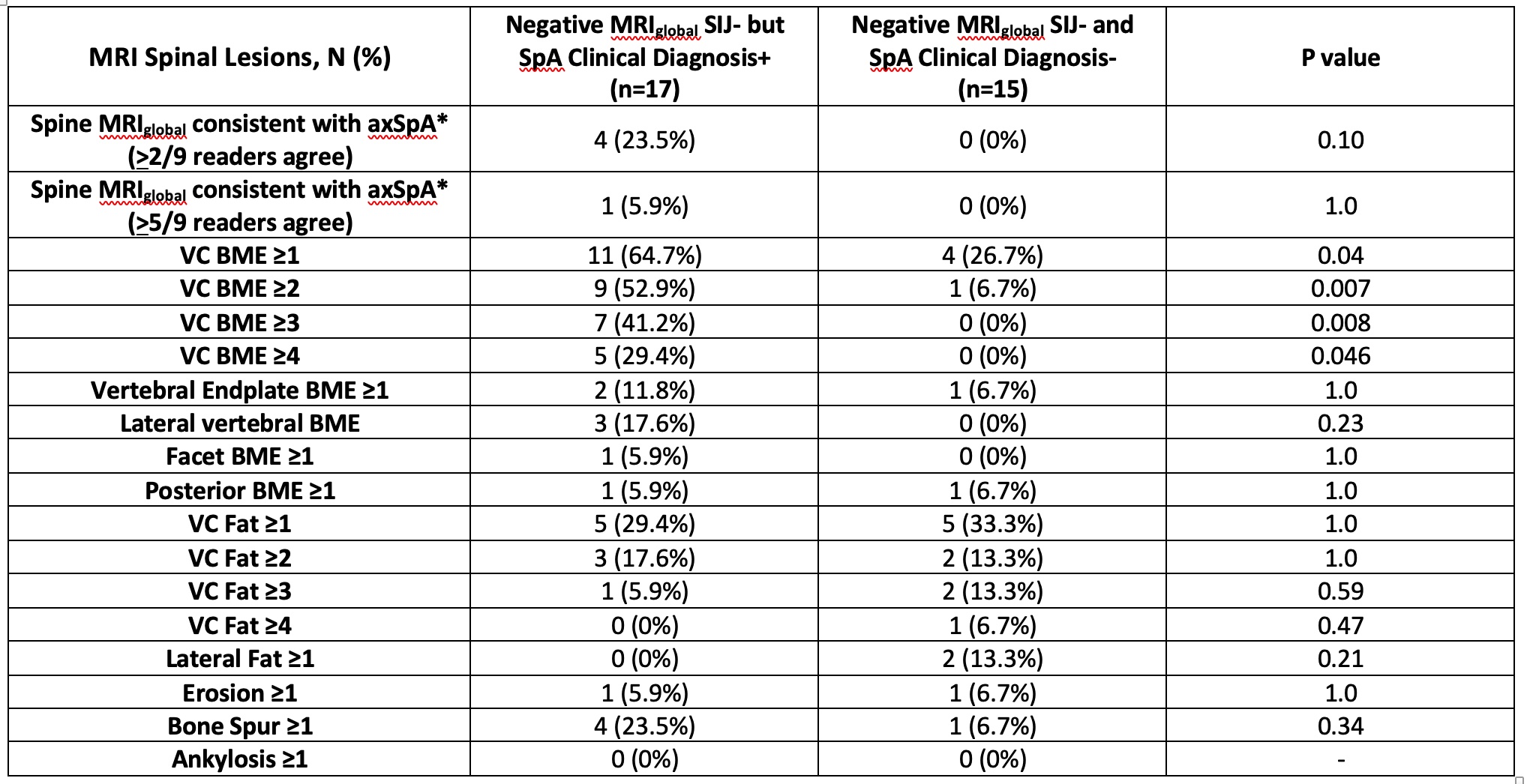 Table 3. Frequency of Spinal MRI lesions in Cases with Negative MRI SIJ scan for AxSpA according to Presence/Absence of Clinical Diagnosis of axSpA
Table 3. Frequency of Spinal MRI lesions in Cases with Negative MRI SIJ scan for AxSpA according to Presence/Absence of Clinical Diagnosis of axSpA
Disclosures: W. Maksymowych, AbbVie, Boehringer-Ingelheim, Celgene, Eli Lilly, Galapagos, Janssen, Novartis, Pfizer, UCB, CARE Arthritis Limited; M. Østergaard, AbbVie/Abbott, Amgen, Bristol-Myers Squibb(BMS), Celgene, Eli Lilly, Janssen, Gilead, Novartis, Pfizer, UCB; X. Baraliakos, AbbVie, Lilly, Galapagos, MSD, Novartis, Pfizer, UCB, Bristol-Myers Squibb, Janssen, Roche, Sandoz, Sanofi; P. Machado, AbbVie/Abbott, Eli Lilly, UCB, Novartis, Orphazyme, Galapagos; S. Pedersen, Novartis, AbbVie/Abbott, UCB, Pfizer, Merck/MSD; U. Weber, None; I. Eshed, None; M. de Hooge, None; J. Sieper, AbbVie/Abbott, Novartis, Eli Lilly, Merck/MSD, UCB, Janssen, Pfizer, Roche; D. Poddubnyy, AbbVie, Biocad, Bristol-Myers Squibb, Eli Lilly, Gilead, GlaxoSmithKline, MSD, Moonlake, Novartis, Pfizer, Samsung-Bioepis, UCB; M. Rudwaleit, AbbVie, Bristol-Myers Squibb (BMS), Boehringer-Ingelheim, Chugai, Eli Lilly, Janssen, Novartis, Pfizer, UCB Pharma; D. van der Heijde, AbbVie, Bayer, BMS, Cyxone, Eisai, Galapagos, Gilead, Glaxo-Smith-Kline, Janssen, Novartis, Pfizer, UCB, Imaging Rheumatology bv, Lilly; R. Landewé, Abbott, Amgen, AstraZeneca, BMS, GSK, Novartis, Merck, Pfizer, Schering-Plough, UCB Pharma; R. Lambert, Calyx, CARE Arthritis, Image Analysis Group.
Background/Purpose: There is limited data as to the frequency of spinal lesions on MRI in patients without MRI or radiographic features typical of sacroiliac joint (SIJ) disease in axial spondyloarthritis (axSpA). This may inform to what degree spine MRI might enhance the diagnostic information provided by SIJ MRI alone. We aimed to assess the frequency of MRI lesions of the spine in the ASAS-Classification Cohort according to the presence of MRI SIJ lesions typical of axSpA and/or radiographic sacroiliitis according to the modified New York criteria (mNY+).
Methods: MRI spine lesions were recorded by 9 central readers in an eCRF that captures global assessment of the spine ("Is the MRI consistent with axSpA: yes/no") (yes=MRIglobal spine+) and detailed anatomical-based scoring of each discovertebral unit plus lateral and posterior structures for bone marrow edema, fat lesions, erosion, and ankylosis, according to ASAS standardized definitions for spinal lesions. Independently, readers globally assessed SIJ scans for active and/or structural lesions typical of axSpA (MRIglobal SIJ+) . We compared the frequency of a positive MRIglobal spine+ and frequencies of different types of spinal lesions according to the presence/absence of axSpA on global evaluation of SIJ MRI scans by ≥5 of 9 readers (MRIglobal SIJ+) and according to the presence/absence of mNY+ radiographic sacroiliitis using Fisher's exact test. Analysis was also stratified by rheumatologist clinical diagnosis.
Results: Among 51 cases with SIJ as well as spine MRI scans and radiographs of the SIJ,19 (37.3%) had a positive MRIglobal SIJ+ scan, and 12 (23.5%) and 7 (13.7%) had a positive MRIglobal spine+ scan according to ≥2 and ≥5 reader agreement, respectively. A positive MRIglobal spine+ scan occurred significantly more frequently in the presence of a positive MRIglobal SIJ+ scan (Table 1) and the presence of radiographic sacroiliitis but was also recorded in 4 of 32(12.5%) (≥2 readers) and 1 of 32(3.4%) (≥5 readers) cases that were negative for a MRIglobal SIJ- scan and x-ray negative (Table 2), all 4 cases being diagnosed with axSpA. Moreover, vertebral corner BME lesions, but not spinal structural lesions, were significantly more frequent in cases that were negative for a MRIglobal SIJ- scan but had been clinically diagnosed as axSpA versus non-axSpA (Table 3).
Conclusion: Spinal lesions on MRI indicative of axSpA per majority central read occurred in about 3% of patients without positive imaging in the SIJ on either MRI or radiography. Frequency of spinal vertebral corner BME lesions was significantly higher in cases with negative SIJ imaging on either MRI or radiography but clinically diagnosed with axSpA.
.jpg) Table 1. Frequency of Spinal MRI lesions According to an MRI SIJ scan Positive for AxSpA
Table 1. Frequency of Spinal MRI lesions According to an MRI SIJ scan Positive for AxSpA 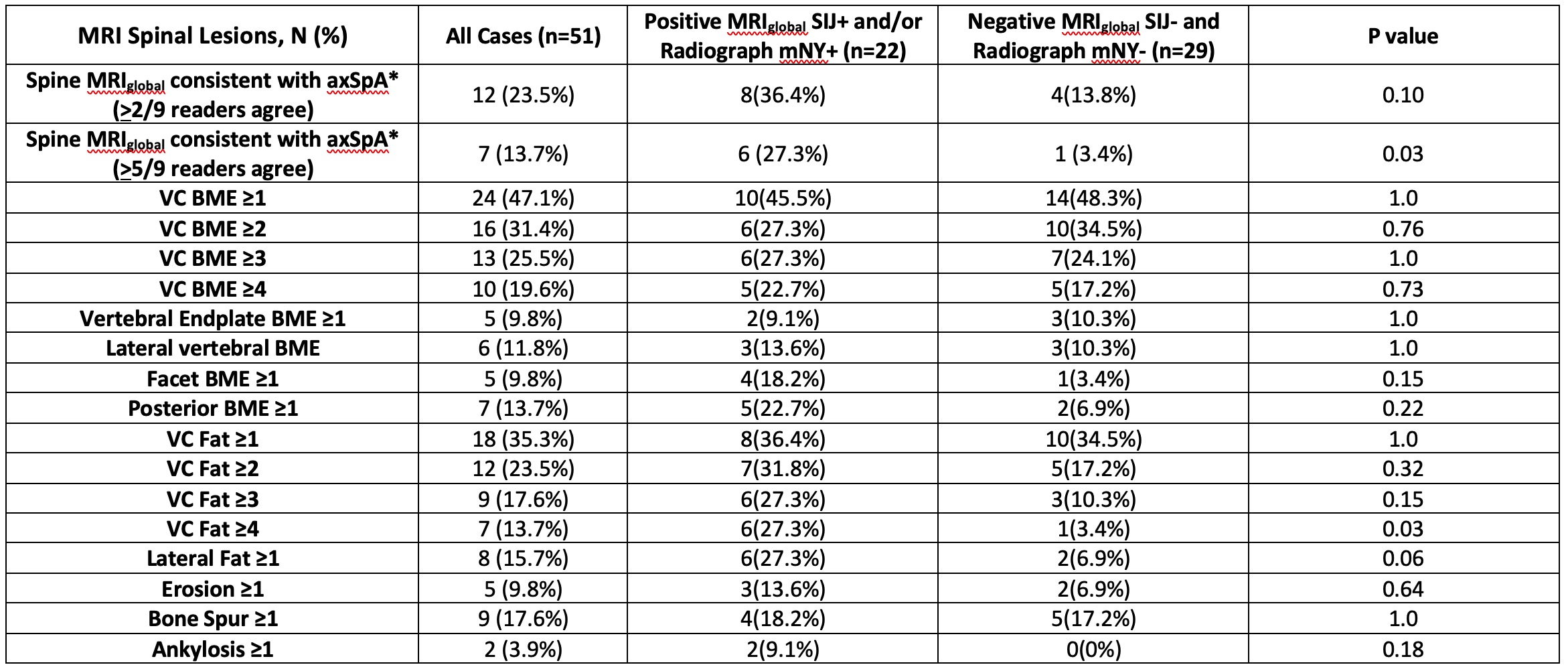 Table 2. Frequency of Spinal MRI lesions According to an MRI SIJ scan Positive for AxSpA and/or Presence/Absence of Radiographic Sacroiliitis (mNY+)
Table 2. Frequency of Spinal MRI lesions According to an MRI SIJ scan Positive for AxSpA and/or Presence/Absence of Radiographic Sacroiliitis (mNY+)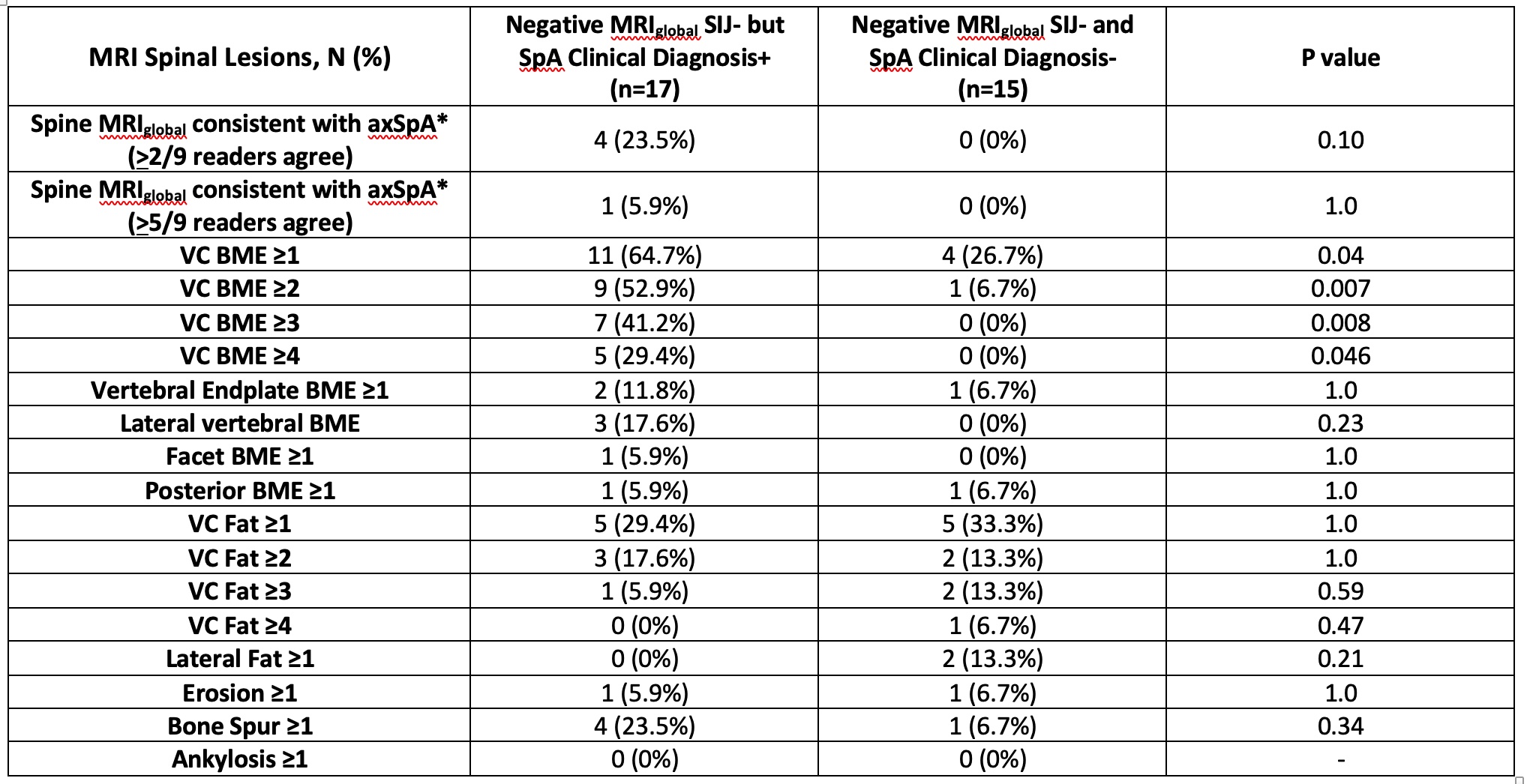 Table 3. Frequency of Spinal MRI lesions in Cases with Negative MRI SIJ scan for AxSpA according to Presence/Absence of Clinical Diagnosis of axSpA
Table 3. Frequency of Spinal MRI lesions in Cases with Negative MRI SIJ scan for AxSpA according to Presence/Absence of Clinical Diagnosis of axSpADisclosures: W. Maksymowych, AbbVie, Boehringer-Ingelheim, Celgene, Eli Lilly, Galapagos, Janssen, Novartis, Pfizer, UCB, CARE Arthritis Limited; M. Østergaard, AbbVie/Abbott, Amgen, Bristol-Myers Squibb(BMS), Celgene, Eli Lilly, Janssen, Gilead, Novartis, Pfizer, UCB; X. Baraliakos, AbbVie, Lilly, Galapagos, MSD, Novartis, Pfizer, UCB, Bristol-Myers Squibb, Janssen, Roche, Sandoz, Sanofi; P. Machado, AbbVie/Abbott, Eli Lilly, UCB, Novartis, Orphazyme, Galapagos; S. Pedersen, Novartis, AbbVie/Abbott, UCB, Pfizer, Merck/MSD; U. Weber, None; I. Eshed, None; M. de Hooge, None; J. Sieper, AbbVie/Abbott, Novartis, Eli Lilly, Merck/MSD, UCB, Janssen, Pfizer, Roche; D. Poddubnyy, AbbVie, Biocad, Bristol-Myers Squibb, Eli Lilly, Gilead, GlaxoSmithKline, MSD, Moonlake, Novartis, Pfizer, Samsung-Bioepis, UCB; M. Rudwaleit, AbbVie, Bristol-Myers Squibb (BMS), Boehringer-Ingelheim, Chugai, Eli Lilly, Janssen, Novartis, Pfizer, UCB Pharma; D. van der Heijde, AbbVie, Bayer, BMS, Cyxone, Eisai, Galapagos, Gilead, Glaxo-Smith-Kline, Janssen, Novartis, Pfizer, UCB, Imaging Rheumatology bv, Lilly; R. Landewé, Abbott, Amgen, AstraZeneca, BMS, GSK, Novartis, Merck, Pfizer, Schering-Plough, UCB Pharma; R. Lambert, Calyx, CARE Arthritis, Image Analysis Group.

