Back
Abstract Session
Session: Abstracts: Muscle Biology, Myositis and Myopathies (2237–2242)
2241: Autoantibodies and Damage in Patients with Idiopathic Inflammatory Myopathies: A Longitudinal Multicenter Study from the EuroMyositis International Network
Monday, November 14, 2022
5:30 PM – 5:40 PM Eastern Time
Location: Room 201
- FE
Fabricio Espinosa-Ortega, MD
Karolinska Institutet
Stockholm, Sweden
Presenting Author(s)
Fabricio Espinosa-Ortega1, Karin Lodin2, Marie Holmqvist1, Maryam Dastmalchi3, Angela Ceribelli4, Jiri Venkovsky5, Hector Chinoy6, Louise Diederichsen7, Samuel Shinjo8, Ingrid Lundberg9 and Helene Alexanderson1, 1Karolinska Institutet, Stockholm, Sweden, 2Karolinska University hospital, Huddinge, Sweden, 3Karolinska University Hospital, Stockholm, Sweden, 4Humanitas Research Hospital, Humanitas University, Rozzano (MI) Italy, Borgo San Giacomo, Italy, 5Charles Univ Prague, Inst Rheumatol, Prague, Czech Republic, Prague, Czech Republic, 6The University of Manchester, Sale, United Kingdom, 7Copenhagen University Hospital, Rigshospitalet, Dragør, Denmark, 8Faculdade de Medicina FMUSP, Universidade de São Paulo, São Paulo, Brazil, 9Karolinska Universitetssjukhuset, Karolinska Institutet, Stockholm, Sweden
Background/Purpose: Patients with idiopathic inflammatory myopathies (IIM) may harbor autoantibodies that are associated with well-defined clinical phenotypes. The association of these autoantibodies with level of damage is unknown. Therefore, we aimed to study the effect of autoantibodies on the trajectories of change of damage over time using a large international cohort of patients with IIM.
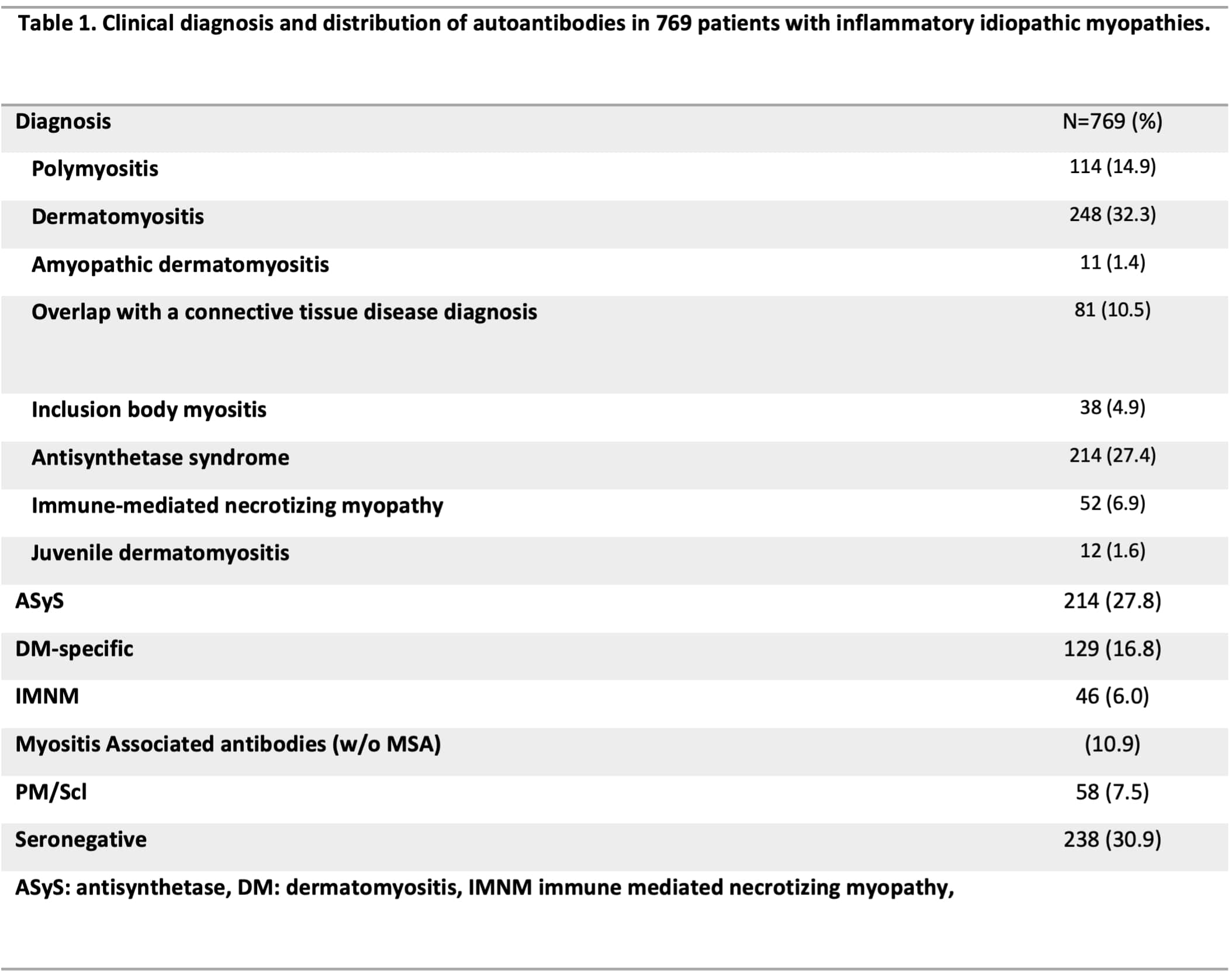
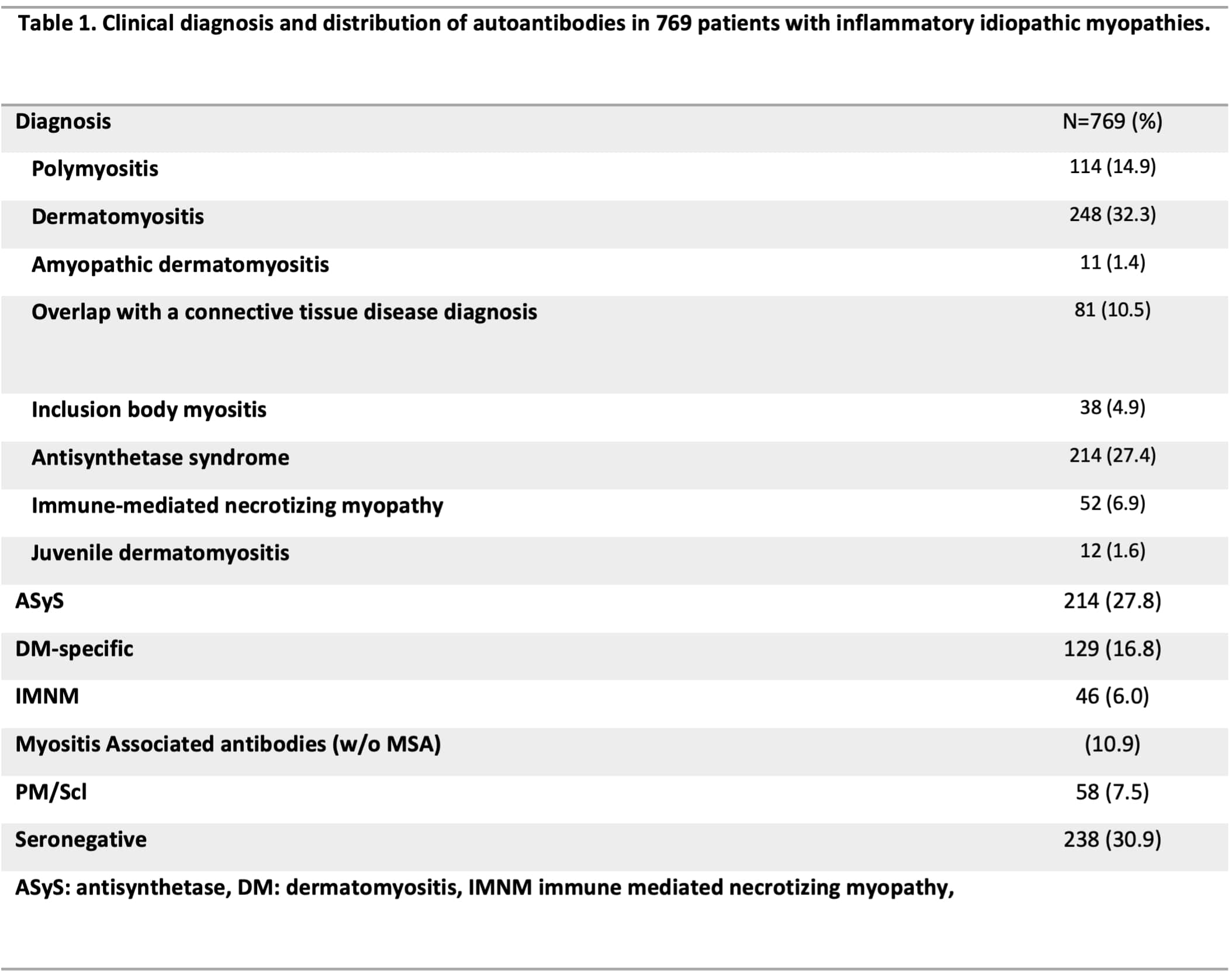
Methods: We conducted a longitudinal analysis using the EuroMyositis registry including patients classified as IIM (1) who were tested for autoantibodies and had at least 1 assessment of damage (Myositis Damage Index, MDI) (2) Patients were sub-grouped by their autoantibody status (Table 1). The primary outcome was the change on MDI extent of damage over the entire follow-up time (up to 16 years) analyzed by linear mixed models. The MDI score varies between 0-38, where 0 indicates no damage in 11 different organs, including malignancy and infection . We used the autoantibody status as independent variable of trajectories of change. The time point for the first MDI assessment registered was defined as the index date.
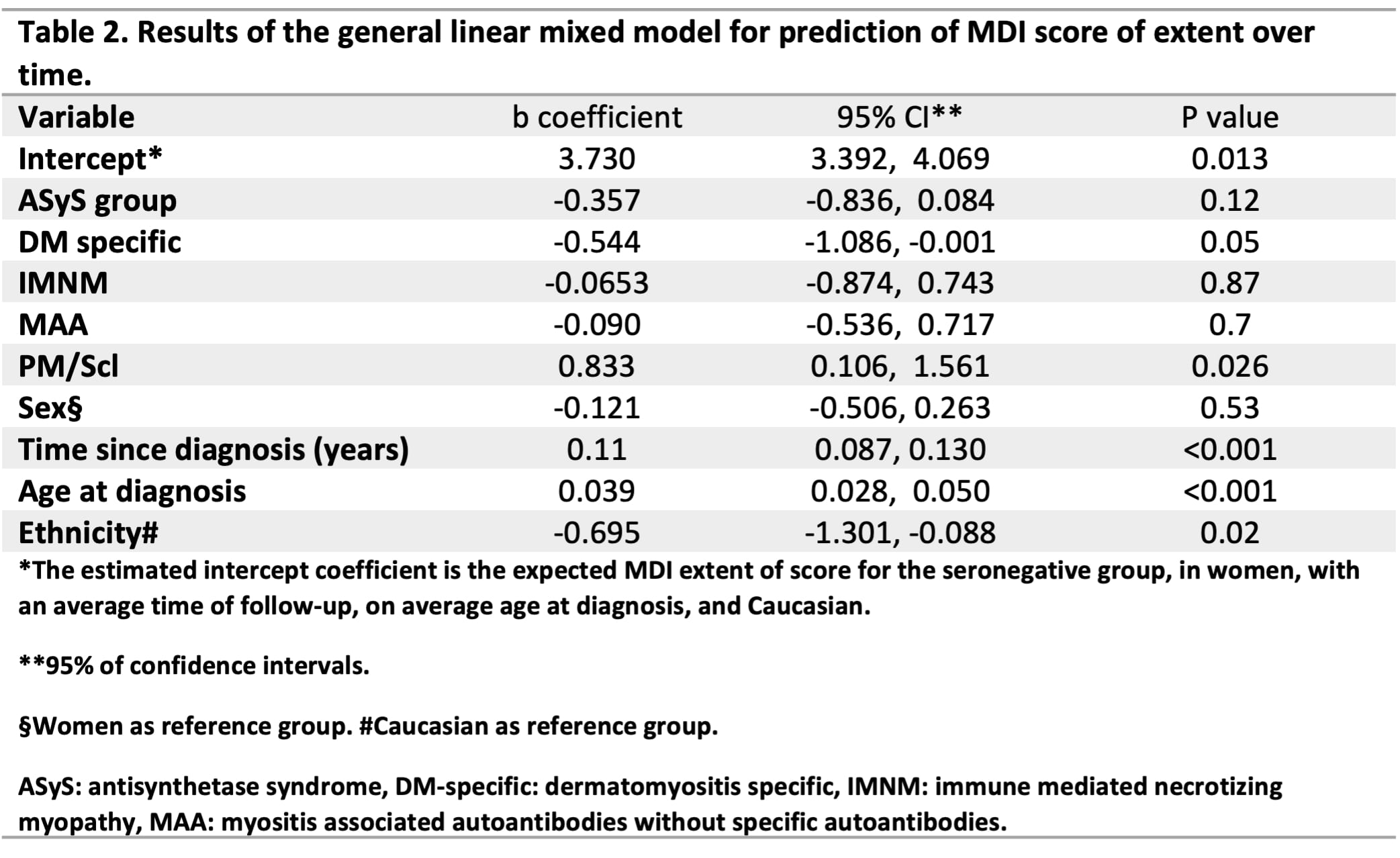
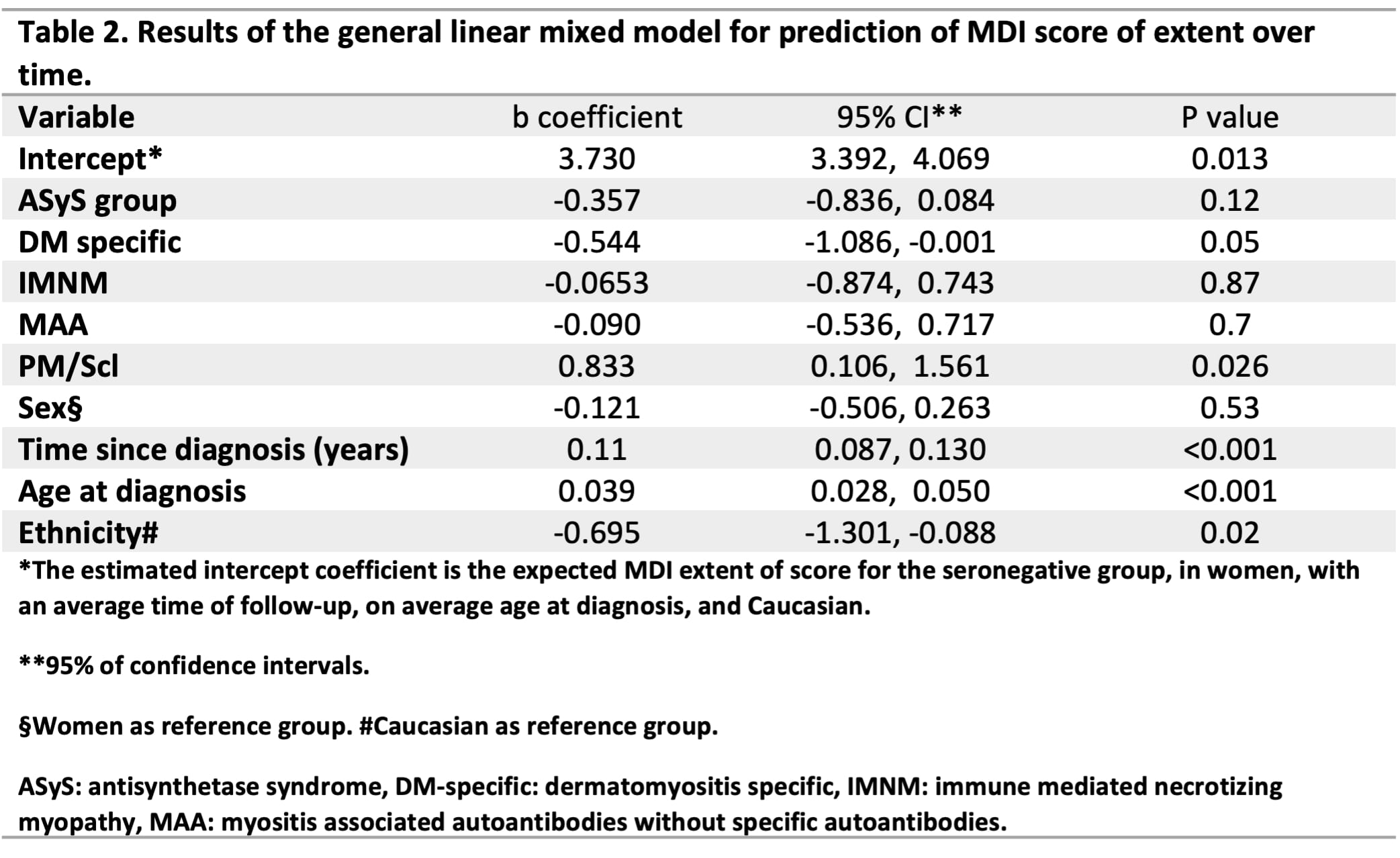
Results: A total of 769 patients were included, 70% (n=523) were women, mean age at diagnosis was 50 years, and median time of disease duration at index date was 1.67 years (IQR 0.54 – 5.0). The overall mean MDI score at index date was 3.17 (SD 2.18) and 85% of patients had at least 1 item of damage registered at index date. Compared with the seronegative group, patients with DM-specific antibodies registered less damage over time (on average 0.54 less score, P=0.05) while patients with PM/Scl antibodies registered higher damage (on average 0.83 higher score, P=0.026) independent of disease duration from diagnosis, age at diagnosis, sex, and ethnicity (Table 2 & Figure 1). The effect of disease duration had an estimated score increase of 0.11 in the MDI extent per year of disease duration since diagnosis, independent of the antibody-status.
Conclusion: Our study is the first to describe patterns and trajectories of change of damage over time in relation to autoantibody status in a large international multicenter cohort of patients with IIM. These findings indicate that the autoantibody status is useful as predictor of organ damage in these patients.
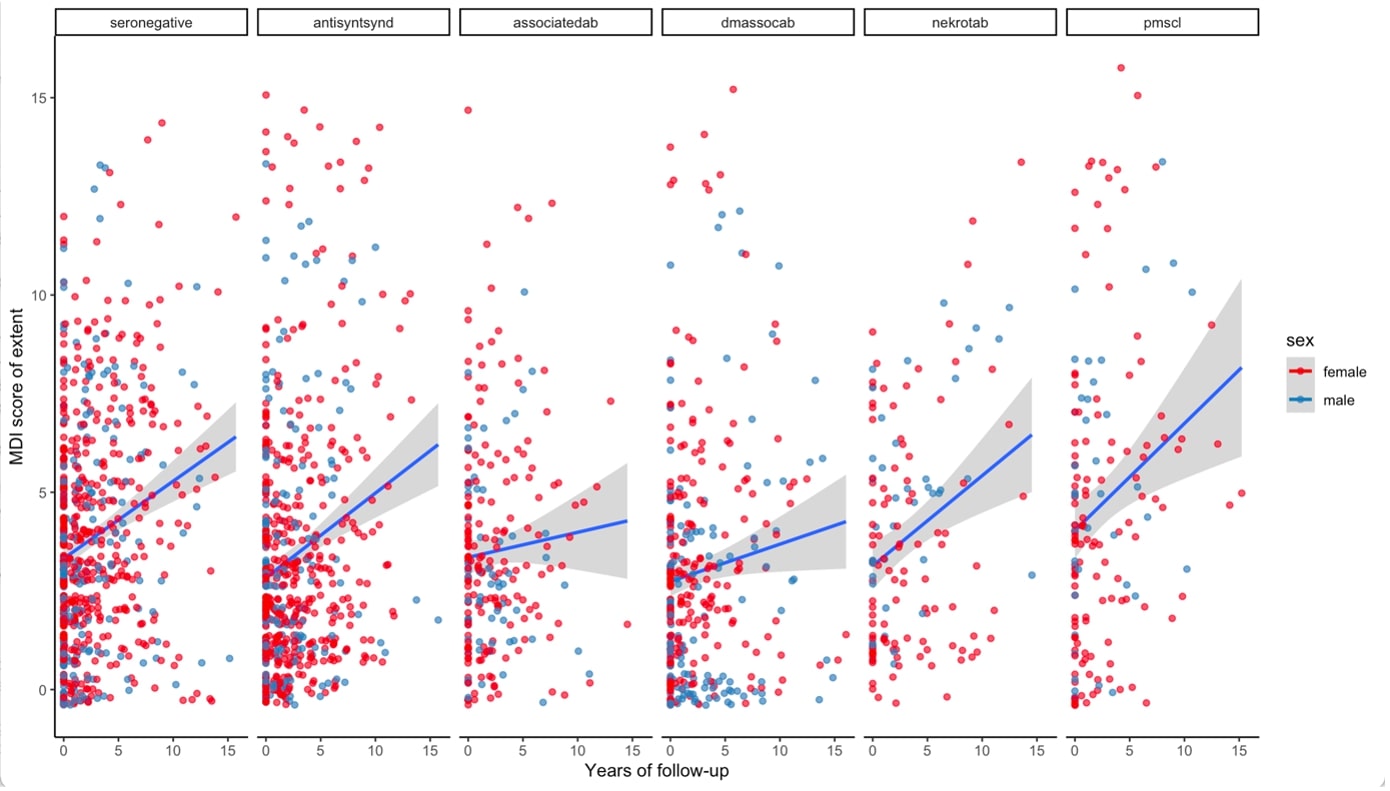 Figure 1. Predicted trajectories of the MDI score of extent by the autoantibody-defined groups and by sex in patients with idiopathic inflammatory myopathies.
Figure 1. Predicted trajectories of the MDI score of extent by the autoantibody-defined groups and by sex in patients with idiopathic inflammatory myopathies.
Legend. Each point represents a patient. The blue lines represent the predicted trajectory of the change on the MDI score of extent using linear regression. The grey shadow represents the confidence interval. Years of follow-up since the index date. NOTE: antisyntsynd: antisynthetase antibodies, associatedab: myositis associated autoantibodies without specific antiantibodies, dmassoc: dermatomyositis specific autoantibodies, nekrotab: immune mediated necrotizing autoantibodies.
Disclosures: F. Espinosa-Ortega, None; K. Lodin, None; M. Holmqvist, None; M. Dastmalchi, None; A. Ceribelli, None; J. Venkovsky, None; H. Chinoy, Eli Lilly, UCB; L. Diederichsen, None; S. Shinjo, None; I. Lundberg, Argenx, AstraZeneca, Bristol Myers Squibb, Novartis, Corbus, EMD Serono, Roche, Pfizer, Orphazyme, Octapharma, Kezar, Janssen; H. Alexanderson, None.
Background/Purpose: Patients with idiopathic inflammatory myopathies (IIM) may harbor autoantibodies that are associated with well-defined clinical phenotypes. The association of these autoantibodies with level of damage is unknown. Therefore, we aimed to study the effect of autoantibodies on the trajectories of change of damage over time using a large international cohort of patients with IIM.
Methods: We conducted a longitudinal analysis using the EuroMyositis registry including patients classified as IIM (1) who were tested for autoantibodies and had at least 1 assessment of damage (Myositis Damage Index, MDI) (2) Patients were sub-grouped by their autoantibody status (Table 1). The primary outcome was the change on MDI extent of damage over the entire follow-up time (up to 16 years) analyzed by linear mixed models. The MDI score varies between 0-38, where 0 indicates no damage in 11 different organs, including malignancy and infection . We used the autoantibody status as independent variable of trajectories of change. The time point for the first MDI assessment registered was defined as the index date.
Results: A total of 769 patients were included, 70% (n=523) were women, mean age at diagnosis was 50 years, and median time of disease duration at index date was 1.67 years (IQR 0.54 – 5.0). The overall mean MDI score at index date was 3.17 (SD 2.18) and 85% of patients had at least 1 item of damage registered at index date. Compared with the seronegative group, patients with DM-specific antibodies registered less damage over time (on average 0.54 less score, P=0.05) while patients with PM/Scl antibodies registered higher damage (on average 0.83 higher score, P=0.026) independent of disease duration from diagnosis, age at diagnosis, sex, and ethnicity (Table 2 & Figure 1). The effect of disease duration had an estimated score increase of 0.11 in the MDI extent per year of disease duration since diagnosis, independent of the antibody-status.
Conclusion: Our study is the first to describe patterns and trajectories of change of damage over time in relation to autoantibody status in a large international multicenter cohort of patients with IIM. These findings indicate that the autoantibody status is useful as predictor of organ damage in these patients.
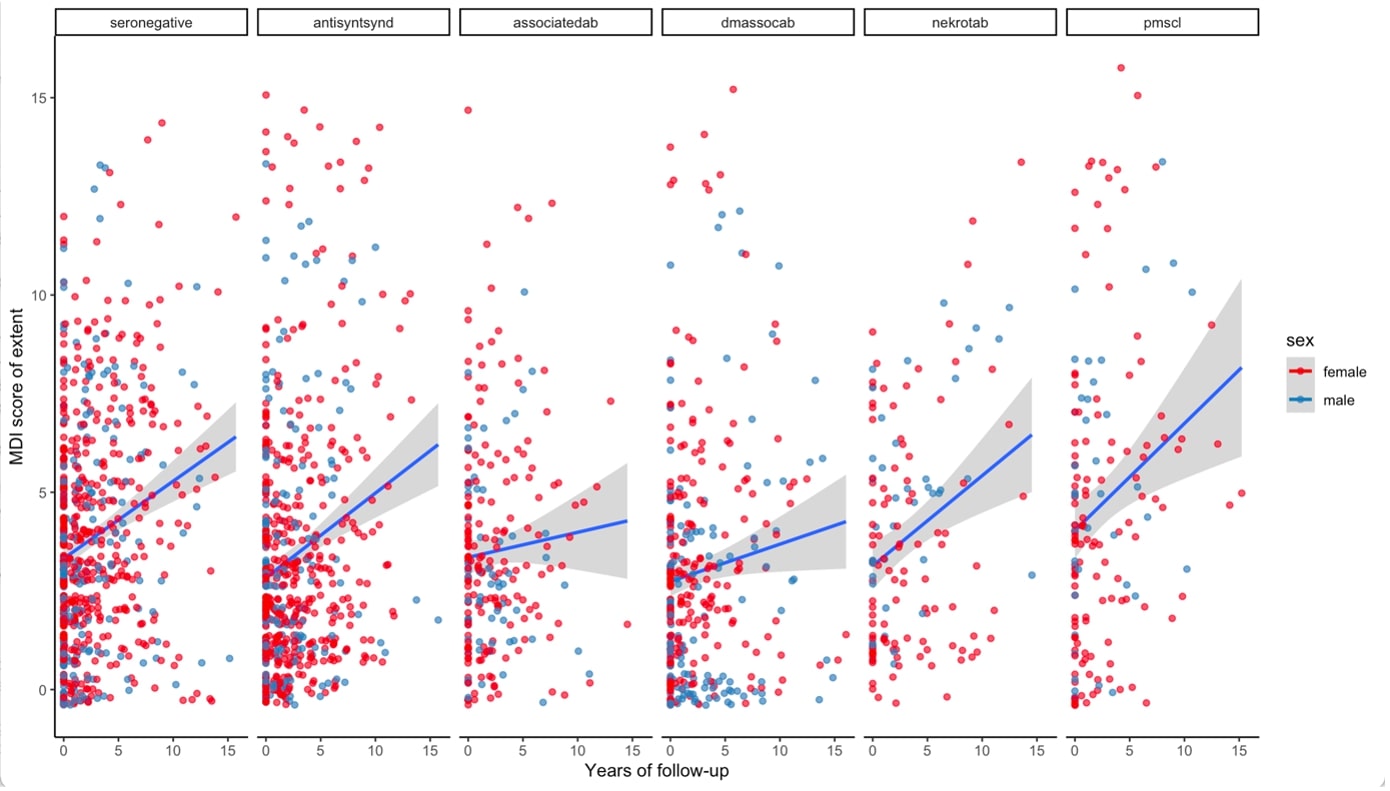 Figure 1. Predicted trajectories of the MDI score of extent by the autoantibody-defined groups and by sex in patients with idiopathic inflammatory myopathies.
Figure 1. Predicted trajectories of the MDI score of extent by the autoantibody-defined groups and by sex in patients with idiopathic inflammatory myopathies.Legend. Each point represents a patient. The blue lines represent the predicted trajectory of the change on the MDI score of extent using linear regression. The grey shadow represents the confidence interval. Years of follow-up since the index date. NOTE: antisyntsynd: antisynthetase antibodies, associatedab: myositis associated autoantibodies without specific antiantibodies, dmassoc: dermatomyositis specific autoantibodies, nekrotab: immune mediated necrotizing autoantibodies.
Disclosures: F. Espinosa-Ortega, None; K. Lodin, None; M. Holmqvist, None; M. Dastmalchi, None; A. Ceribelli, None; J. Venkovsky, None; H. Chinoy, Eli Lilly, UCB; L. Diederichsen, None; S. Shinjo, None; I. Lundberg, Argenx, AstraZeneca, Bristol Myers Squibb, Novartis, Corbus, EMD Serono, Roche, Pfizer, Orphazyme, Octapharma, Kezar, Janssen; H. Alexanderson, None.

