Back
Abstract Session
Session: Abstracts: RA – Diagnosis, Manifestations, and Outcomes III: RA ILD (2248–2253)
2252: Higher Matrix Metalloproteinase Levels Are Predictive of Incident Interstitial Lung Disease Among a Cohort of US Veterans with Rheumatoid Arthritis
Monday, November 14, 2022
5:30 PM – 5:40 PM Eastern Time
Location: Room 103

Brent Luedders, MD
University of Nebraska Medical Center
Omaha, NE, United States
Presenting Author(s)
Brent Luedders1, Dana Ascherman2, Joshua Baker3, Michael Duryee1, Yangyuna Yang1, Punyasha Roul4, Katherine Wysham5, Paul Monach6, Andreas Reimold7, Gail Kerr8, Gary Kunkel9, Grant Cannon10, Jill Poole1, Geoffrey Thiele1, Ted Mikuls11 and Bryant England1, 1University of Nebraska Medical Center, Omaha, NE, 2University of Pittsburgh, Pittsburgh, PA, 3University of Pennsylvania, Philadelphia, PA, 4UNMC, Omaha, NE, 5VA Puget Sound/University of Washington, Seattle, WA, 6VA Boston Healthcare System, Boston, MA, 7University of Texas Southwestern Medical Center, Dallas, TX, 8Washington DC VAMC/Georgetown and Howard Universities, Washington, DC, 9University of Utah, Salt Lake City, UT, 10Retired, Salt Lake City, UT, 11Division of Rheumatology, University of Nebraska Medical Center, Omaha, NE
Background/Purpose: Matrix metalloproteinases (MMPs) degrade extracellular matrix and have been implicated to play a role in a number of fibrotic processes. Specifically, MMPs have been speculated to play a role in the pathogenesis of rheumatoid arthritis-associated interstitial lung disease (RA-ILD) as well as idiopathic pulmonary fibrosis (IPF), which shares historadiological features with RA-ILD. Although past studies have demonstrated that select circulating MMPs are increased in patients with established RA-ILD and IPF, there have been no prior studies examining whether MMP concentrations predict incident disease. We hypothesized that higher plasma MMP levels in RA patients would be predictive of incident RA-ILD.
Methods: We performed a cohort study of participants with RA and without prevalent ILD in the Veterans Affairs Rheumatoid Arthritis registry, a multicenter, prospective cohort of U.S. Veterans with RA. MMP-1, -3, -7, and -9 concentrations were measured using the MesoScale Discovery platform on plasma samples collected at registry enrollment. MMP values were log-transformed, standardized, and categorized into quartiles. Participants were followed from enrollment until ILD development, death, or end of study period (2003 – 2020). Incident ILD post-enrollment was validated through medical record review of clinical diagnoses, imaging findings, and biopsy reports. The associations of serum MMP concentrations and quartiles with incident ILD were assessed with Cox regression models adjusting for age, sex, race, smoking status, anti-cyclic citrullinated peptide antibody positivity, and RA disease activity at enrollment. In sensitivity analyses, we excluded RA-ILD cases developing within the first year after enrollment to avoid potential inclusion of undiagnosed prevalent RA-ILD cases.
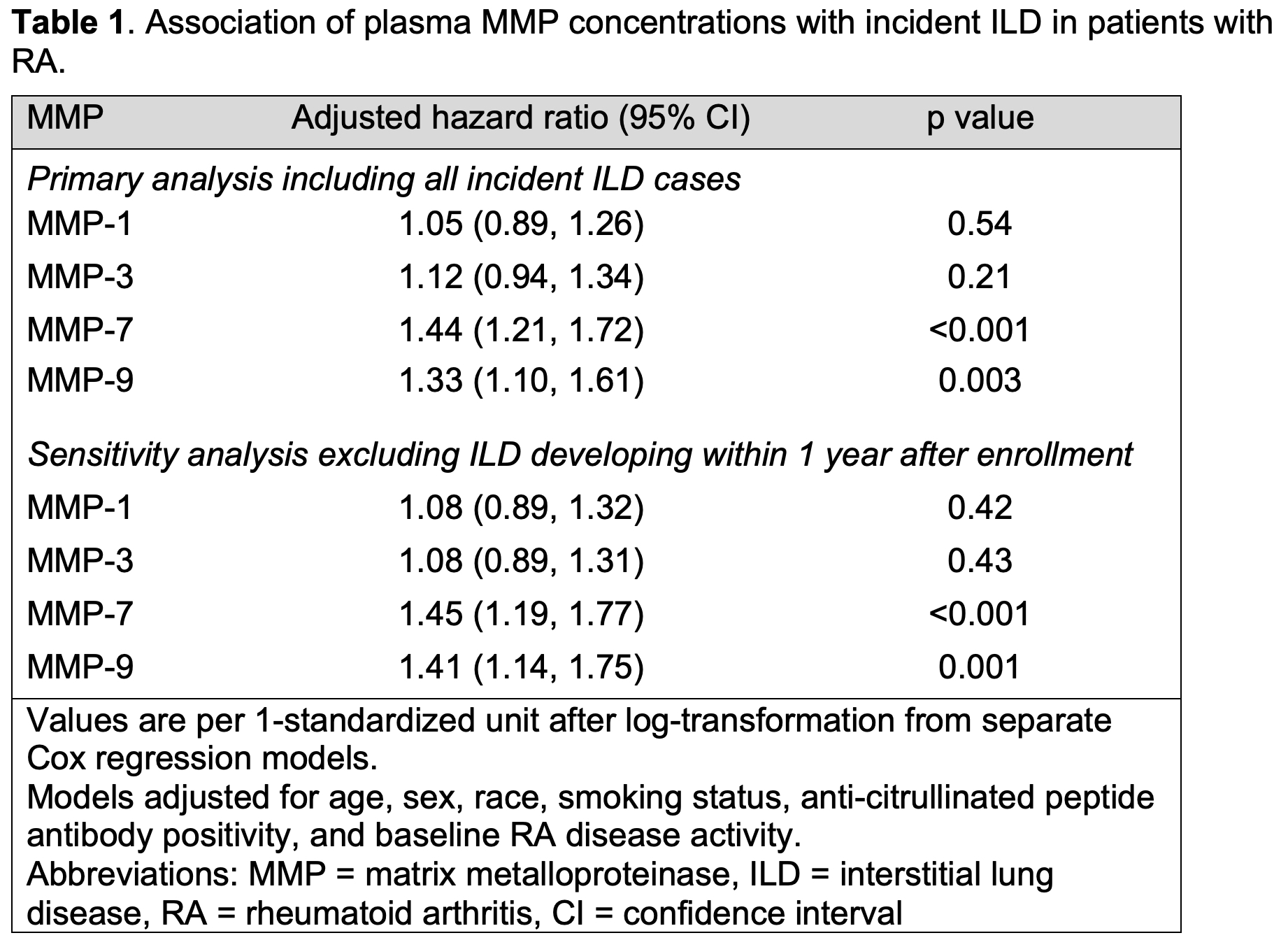
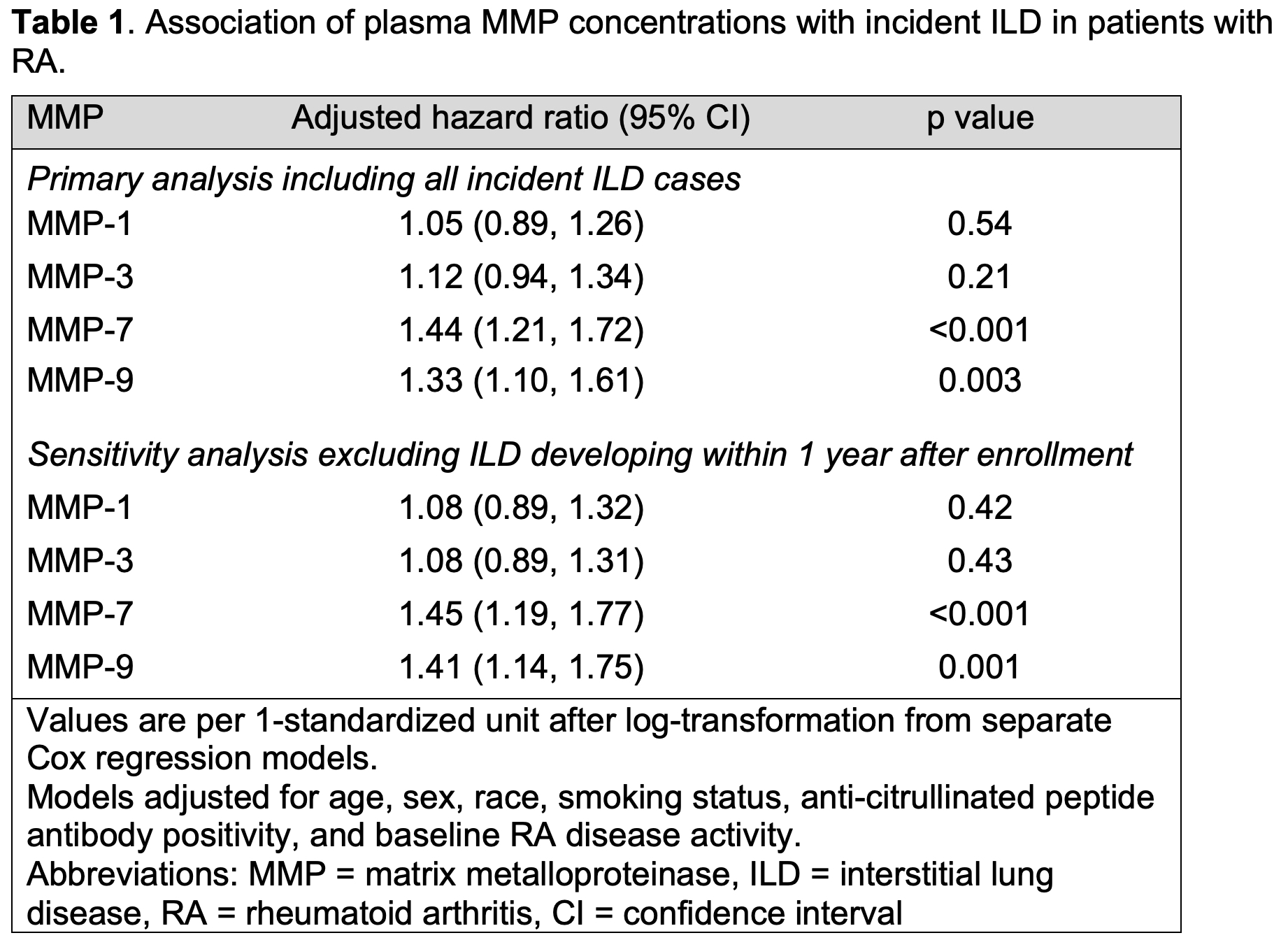
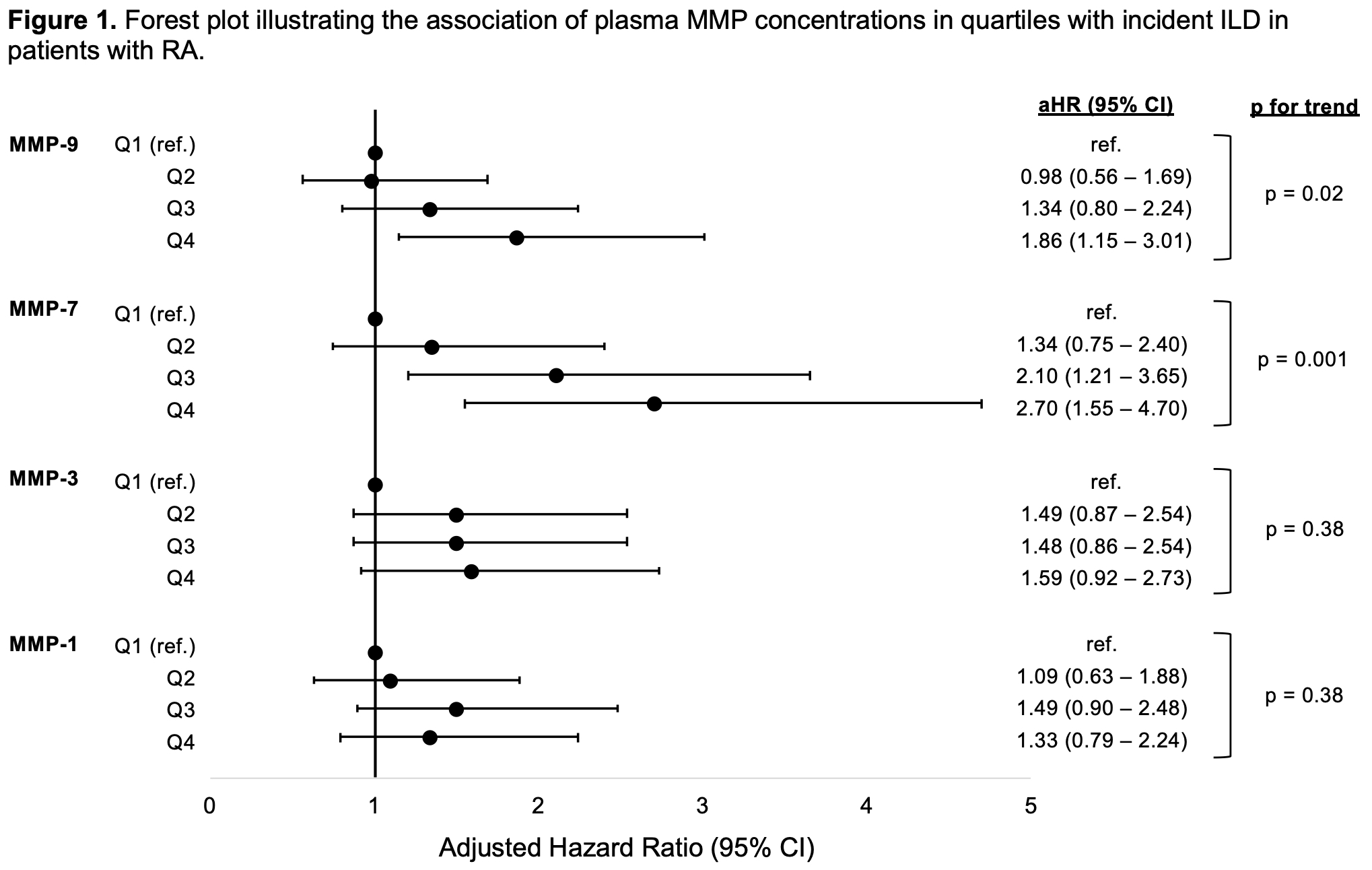
Results: RA-ILD developed in 133 of 2,215 RA participants (89% male, mean age 64 years) over a mean follow-up of 7.8 (SD 4.3) years. Higher plasma concentrations of MMP-7 (aHR 1.44 [1.21, 1.72]) and MMP-9 (aHR 1.33 [1.10, 1.61]) were independently associated with incident RA-ILD during follow-up (Table 1). Individuals with the highest quartile of MMP-7 had a near 3-fold increased risk of developing ILD (aHR 2.70 [1.55, 4.70]) and those with the highest quartile of MMP-9 had a near 2-fold increased risk (aHR 1.86 [1.15, 3.01]). A dose-response relationship was present for both MMP-7 and MMP-9 in which higher quartiles had a higher risk of incident ILD (Figure 1). Inclusion of MMP-1, -3, -7, and -9 concentrations in the same model showed a persistent association of the highest quartile of MMP-7 (aHR 2.49 [1.40, 4.43]) but not MMP-9 (aHR 1.65 [0.98, 2.76]) with incident ILD. Sensitivity analyses excluding RA-ILD cases developing within the first year after enrollment (n=21) were consistent with the primary results (Table 1).
Conclusion: Building on prior work finding MMPs to be associated with established RA-ILD, we found that higher plasma concentrations of MMP-7 and -9 were predictive of an increased risk of developing incident RA-ILD in a multicenter, prospective RA cohort. These peripheral biomarkers show promise for inclusion in RA-ILD risk models, and their predictive performance should be validated in other RA cohorts.
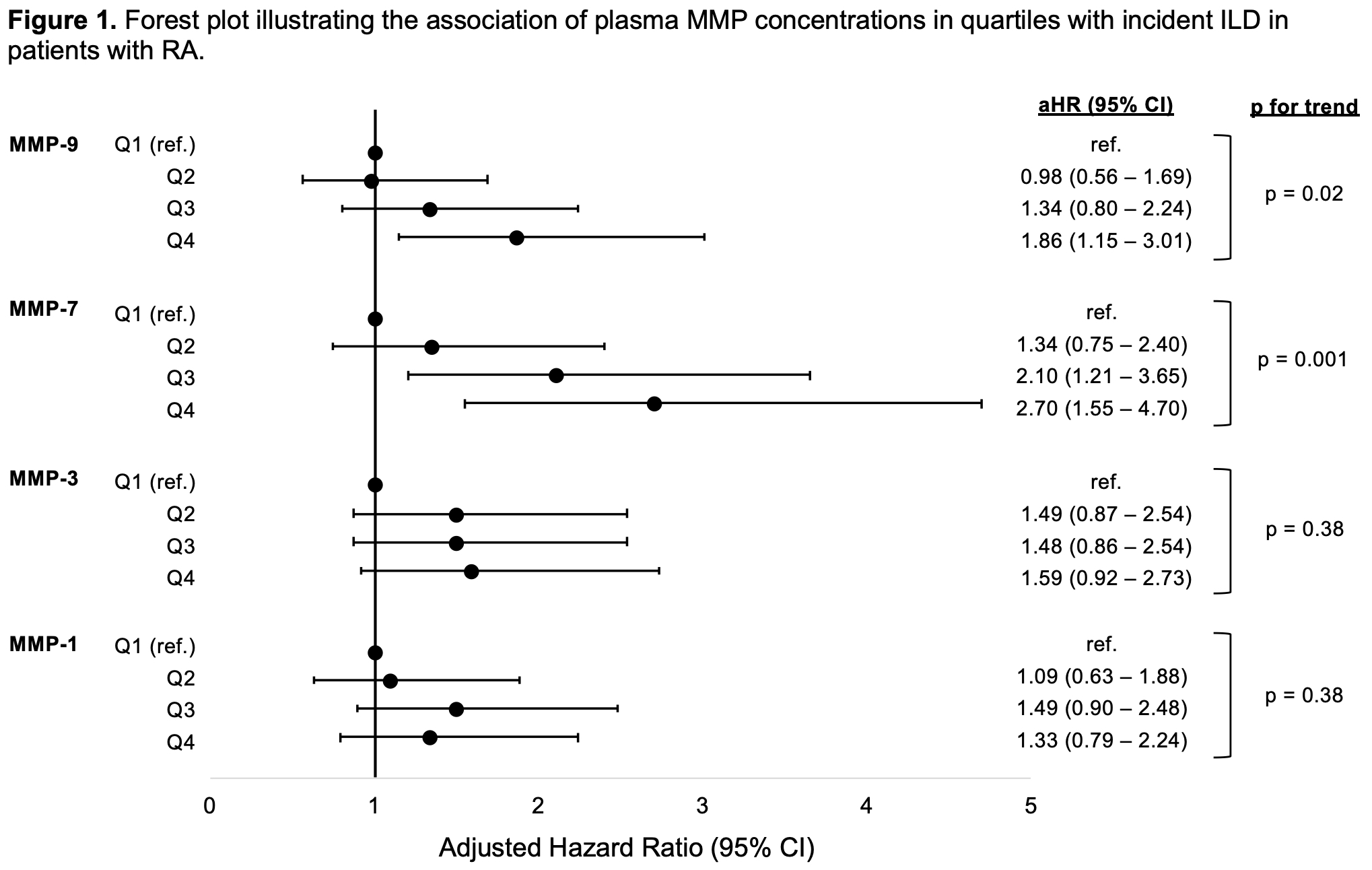 MMPs assessed in separate Cox models adjusting for age, sex, race, smoking, anti-citrullinated peptide antibody positivity, and RA disease activity. Abbreviations: MMP = matrix metalloproteinase, ILD = interstitial lung disease, RA = rheumatoid arthritis, aHR = adjusted hazard ratio, Q = quartile, CI = confidence interval.
MMPs assessed in separate Cox models adjusting for age, sex, race, smoking, anti-citrullinated peptide antibody positivity, and RA disease activity. Abbreviations: MMP = matrix metalloproteinase, ILD = interstitial lung disease, RA = rheumatoid arthritis, aHR = adjusted hazard ratio, Q = quartile, CI = confidence interval.
Disclosures: B. Luedders, None; D. Ascherman, None; J. Baker, Bristol-Myers Squibb(BMS), RediTrex, Pfizer; M. Duryee, None; Y. Yang, None; P. Roul, None; K. Wysham, None; P. Monach, Chemocentryx, Kiniksa, BMS/Celgene, Gilead; A. Reimold, None; G. Kerr, Pfizer, Janssen; G. Kunkel, None; G. Cannon, None; J. Poole, AstraZeneca; G. Thiele, None; T. Mikuls, Gilead Sciences, Bristol-Myers Squibb, Horizon, Sanofi, Pfizer Inc; B. England, Boehringer-Ingelheim.
Background/Purpose: Matrix metalloproteinases (MMPs) degrade extracellular matrix and have been implicated to play a role in a number of fibrotic processes. Specifically, MMPs have been speculated to play a role in the pathogenesis of rheumatoid arthritis-associated interstitial lung disease (RA-ILD) as well as idiopathic pulmonary fibrosis (IPF), which shares historadiological features with RA-ILD. Although past studies have demonstrated that select circulating MMPs are increased in patients with established RA-ILD and IPF, there have been no prior studies examining whether MMP concentrations predict incident disease. We hypothesized that higher plasma MMP levels in RA patients would be predictive of incident RA-ILD.
Methods: We performed a cohort study of participants with RA and without prevalent ILD in the Veterans Affairs Rheumatoid Arthritis registry, a multicenter, prospective cohort of U.S. Veterans with RA. MMP-1, -3, -7, and -9 concentrations were measured using the MesoScale Discovery platform on plasma samples collected at registry enrollment. MMP values were log-transformed, standardized, and categorized into quartiles. Participants were followed from enrollment until ILD development, death, or end of study period (2003 – 2020). Incident ILD post-enrollment was validated through medical record review of clinical diagnoses, imaging findings, and biopsy reports. The associations of serum MMP concentrations and quartiles with incident ILD were assessed with Cox regression models adjusting for age, sex, race, smoking status, anti-cyclic citrullinated peptide antibody positivity, and RA disease activity at enrollment. In sensitivity analyses, we excluded RA-ILD cases developing within the first year after enrollment to avoid potential inclusion of undiagnosed prevalent RA-ILD cases.
Results: RA-ILD developed in 133 of 2,215 RA participants (89% male, mean age 64 years) over a mean follow-up of 7.8 (SD 4.3) years. Higher plasma concentrations of MMP-7 (aHR 1.44 [1.21, 1.72]) and MMP-9 (aHR 1.33 [1.10, 1.61]) were independently associated with incident RA-ILD during follow-up (Table 1). Individuals with the highest quartile of MMP-7 had a near 3-fold increased risk of developing ILD (aHR 2.70 [1.55, 4.70]) and those with the highest quartile of MMP-9 had a near 2-fold increased risk (aHR 1.86 [1.15, 3.01]). A dose-response relationship was present for both MMP-7 and MMP-9 in which higher quartiles had a higher risk of incident ILD (Figure 1). Inclusion of MMP-1, -3, -7, and -9 concentrations in the same model showed a persistent association of the highest quartile of MMP-7 (aHR 2.49 [1.40, 4.43]) but not MMP-9 (aHR 1.65 [0.98, 2.76]) with incident ILD. Sensitivity analyses excluding RA-ILD cases developing within the first year after enrollment (n=21) were consistent with the primary results (Table 1).
Conclusion: Building on prior work finding MMPs to be associated with established RA-ILD, we found that higher plasma concentrations of MMP-7 and -9 were predictive of an increased risk of developing incident RA-ILD in a multicenter, prospective RA cohort. These peripheral biomarkers show promise for inclusion in RA-ILD risk models, and their predictive performance should be validated in other RA cohorts.
 MMPs assessed in separate Cox models adjusting for age, sex, race, smoking, anti-citrullinated peptide antibody positivity, and RA disease activity. Abbreviations: MMP = matrix metalloproteinase, ILD = interstitial lung disease, RA = rheumatoid arthritis, aHR = adjusted hazard ratio, Q = quartile, CI = confidence interval.
MMPs assessed in separate Cox models adjusting for age, sex, race, smoking, anti-citrullinated peptide antibody positivity, and RA disease activity. Abbreviations: MMP = matrix metalloproteinase, ILD = interstitial lung disease, RA = rheumatoid arthritis, aHR = adjusted hazard ratio, Q = quartile, CI = confidence interval.Disclosures: B. Luedders, None; D. Ascherman, None; J. Baker, Bristol-Myers Squibb(BMS), RediTrex, Pfizer; M. Duryee, None; Y. Yang, None; P. Roul, None; K. Wysham, None; P. Monach, Chemocentryx, Kiniksa, BMS/Celgene, Gilead; A. Reimold, None; G. Kerr, Pfizer, Janssen; G. Kunkel, None; G. Cannon, None; J. Poole, AstraZeneca; G. Thiele, None; T. Mikuls, Gilead Sciences, Bristol-Myers Squibb, Horizon, Sanofi, Pfizer Inc; B. England, Boehringer-Ingelheim.

