Back
Poster Session B
Systemic lupus erythematosus (SLE)
Session: (0974–1003) SLE – Treatment Poster II
0980: The Effect and Outcomes of HCQ Alone and in Combination with Anti-Depressants on QTc
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- KR
Kourtney Rudzinski, DO
Lehigh Valley Health Network
Easton, PA, United States
Abstract Poster Presenter(s)
Kourtney Rudzinski1, Zaina Shahid2, Yasin kanakrieh2, Saloni Goyal2, Kyle Shaak2 and James Ross3, 1Lehigh Valley Health Network, Tatamy, PA, 2Lehigh Valley Health Network, Allentown, PA, 3lvhn, Macungie, PA
Background/Purpose: Hydroxychloroquine (HCQ) has faced increased scrutiny during the COVID pandemic for its association with QTc prolongation. In our field, patients are commonly on antidepressant medications that can further increase these risks. Our goal in this study was to see if HCQ in combination with antidepressants was associated with increased risk of QTc prolongation or increased life-threatening arrhythmias or sudden cardiac death (SCD). We have also gathered data on confounding variables such as concomitant use of anti-arrhythmics, antibiotics, antifungals, as well as the presence of CHF and CAD.
Methods: A retrospective chart review from March 15 2015 to May 12 2021 gathered 949 records of patients on HCQ for more than 1 month, over the age of 18, and with an EKG documented while on HCQ. Descriptive statistics were used to summarize the demographic characteristics of the study sample, including patient demographics and clinical baseline characteristics. The primary analysis of the study was a two-step process utilizing the chi-square test of independence and binomial logistic regression. Chi-square analyses were used to test for associations between demographic and clinical variables and the outcome of a prolonged QTc. Variables that were included in this stage were gender, race, ethnicity, actively taking antidepressants, actively taking anti-arrhythmics and renal and/or hepatic disease. If bivariate analysis resulted in a p-value less than 0.25 the variable was included in logistic regression analysis. Additional chi-square tests were used to compare a diagnosed prolonged QTc based on antidepressant prescription, as well as renal or hepatic disease.
Results: All variables included in the logistic regression model were found to be significantly associated with a prolonged QTc at the 5% significance level: CAD, CHF, actively taking antidepressants, actively taking anti-arrhythmics and renal and/or hepatic disease. The odds of having prolonged QTc while on HCQ was highest among those taking anti-arrhythmics, followed by those with CHF, then presence of hepatic or renal disease, then presence of CAD, and lastly followed by patients on antidepressants. The electrolyte abnormality most frequently associated with prolonged QTc was hypokalemia. Patients taking antidepressants had a significantly higher chance of a prolonged QTc but no significant difference was seen for life-threatening arrhythmia or SCD.
Conclusion: While our study did have limitations, it demonstrated that antidepressant use with HCQ was associated with prolonged QTc but did not increase life-threatening arrhythmias or SCD. Our results showed the highest risks for QTc prolongation were in patients on anti-arrhymthics, followed by patients with CHF, and then patients with hepatic or renal disease. Therefore, special considerations might need to be considered in these populations. Future studies can assess benefits of baseline EKGs to determine if adding HCQ results in new or worsening QTc in higher risk populations.
References:
1. Dietle, A. (2015). QTc Prolongation With Antidepressants and Antipsychotics. US Pharm, 40(11), HS34-HS40.
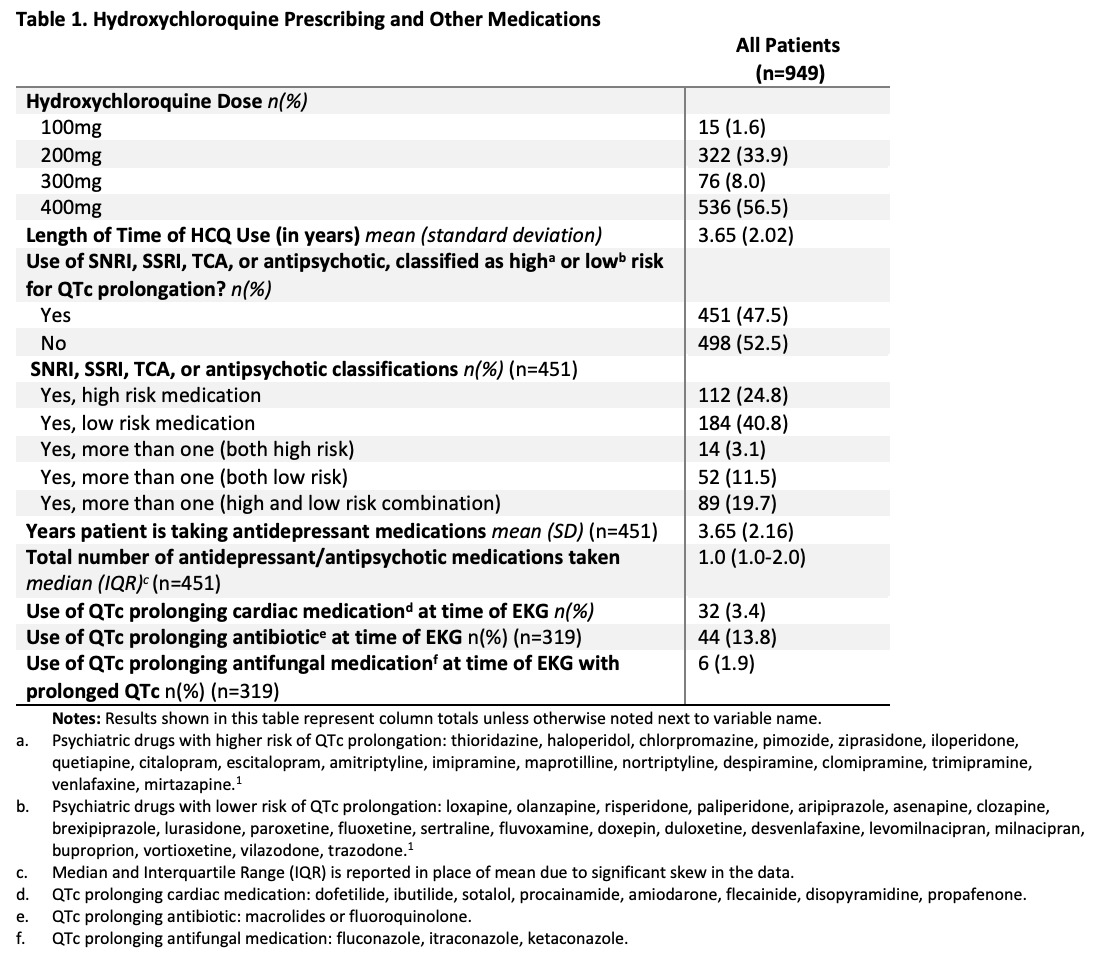 Table 1. Hydroxychloroquine Prescribing and Other Medications
Table 1. Hydroxychloroquine Prescribing and Other Medications
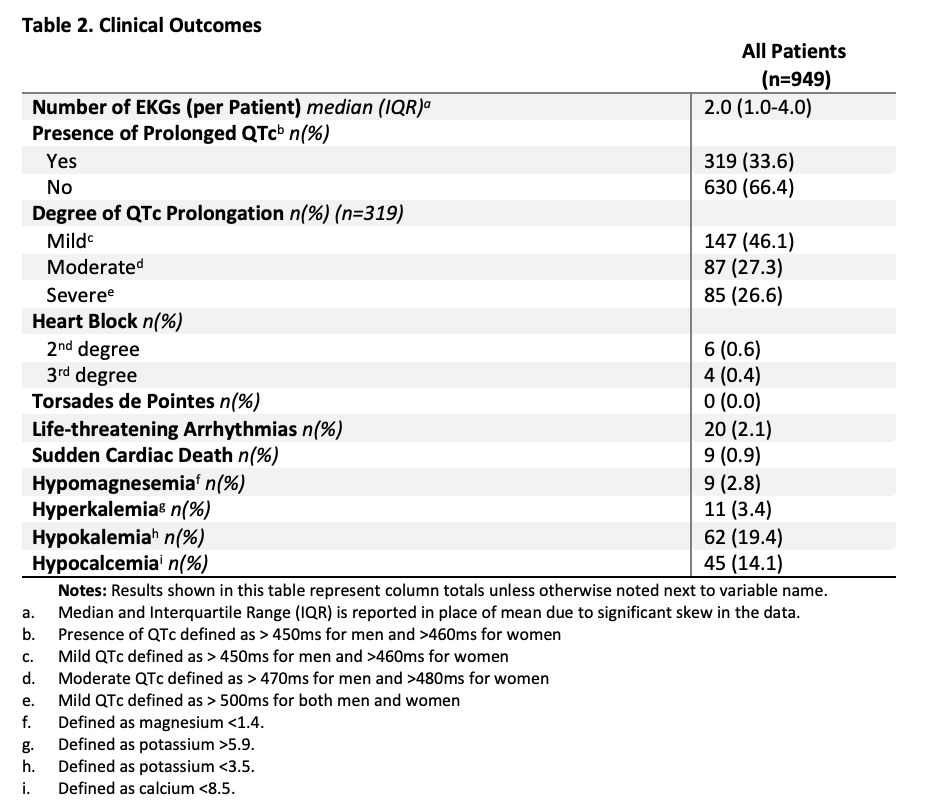 Table 2. Clinical Outcomes
Table 2. Clinical Outcomes
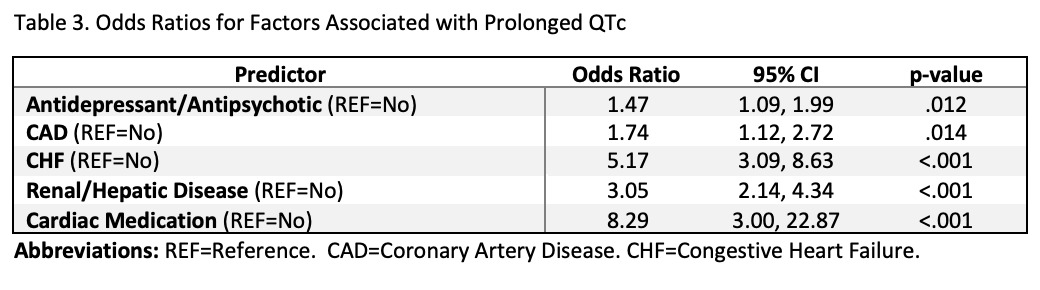 Table 3. Odds Ratio for Factors Associated with Prolonged QTc
Table 3. Odds Ratio for Factors Associated with Prolonged QTc
Disclosures: K. Rudzinski, None; Z. Shahid, None; Y. kanakrieh, None; S. Goyal, None; K. Shaak, None; J. Ross, None.
Background/Purpose: Hydroxychloroquine (HCQ) has faced increased scrutiny during the COVID pandemic for its association with QTc prolongation. In our field, patients are commonly on antidepressant medications that can further increase these risks. Our goal in this study was to see if HCQ in combination with antidepressants was associated with increased risk of QTc prolongation or increased life-threatening arrhythmias or sudden cardiac death (SCD). We have also gathered data on confounding variables such as concomitant use of anti-arrhythmics, antibiotics, antifungals, as well as the presence of CHF and CAD.
Methods: A retrospective chart review from March 15 2015 to May 12 2021 gathered 949 records of patients on HCQ for more than 1 month, over the age of 18, and with an EKG documented while on HCQ. Descriptive statistics were used to summarize the demographic characteristics of the study sample, including patient demographics and clinical baseline characteristics. The primary analysis of the study was a two-step process utilizing the chi-square test of independence and binomial logistic regression. Chi-square analyses were used to test for associations between demographic and clinical variables and the outcome of a prolonged QTc. Variables that were included in this stage were gender, race, ethnicity, actively taking antidepressants, actively taking anti-arrhythmics and renal and/or hepatic disease. If bivariate analysis resulted in a p-value less than 0.25 the variable was included in logistic regression analysis. Additional chi-square tests were used to compare a diagnosed prolonged QTc based on antidepressant prescription, as well as renal or hepatic disease.
Results: All variables included in the logistic regression model were found to be significantly associated with a prolonged QTc at the 5% significance level: CAD, CHF, actively taking antidepressants, actively taking anti-arrhythmics and renal and/or hepatic disease. The odds of having prolonged QTc while on HCQ was highest among those taking anti-arrhythmics, followed by those with CHF, then presence of hepatic or renal disease, then presence of CAD, and lastly followed by patients on antidepressants. The electrolyte abnormality most frequently associated with prolonged QTc was hypokalemia. Patients taking antidepressants had a significantly higher chance of a prolonged QTc but no significant difference was seen for life-threatening arrhythmia or SCD.
Conclusion: While our study did have limitations, it demonstrated that antidepressant use with HCQ was associated with prolonged QTc but did not increase life-threatening arrhythmias or SCD. Our results showed the highest risks for QTc prolongation were in patients on anti-arrhymthics, followed by patients with CHF, and then patients with hepatic or renal disease. Therefore, special considerations might need to be considered in these populations. Future studies can assess benefits of baseline EKGs to determine if adding HCQ results in new or worsening QTc in higher risk populations.
References:
1. Dietle, A. (2015). QTc Prolongation With Antidepressants and Antipsychotics. US Pharm, 40(11), HS34-HS40.
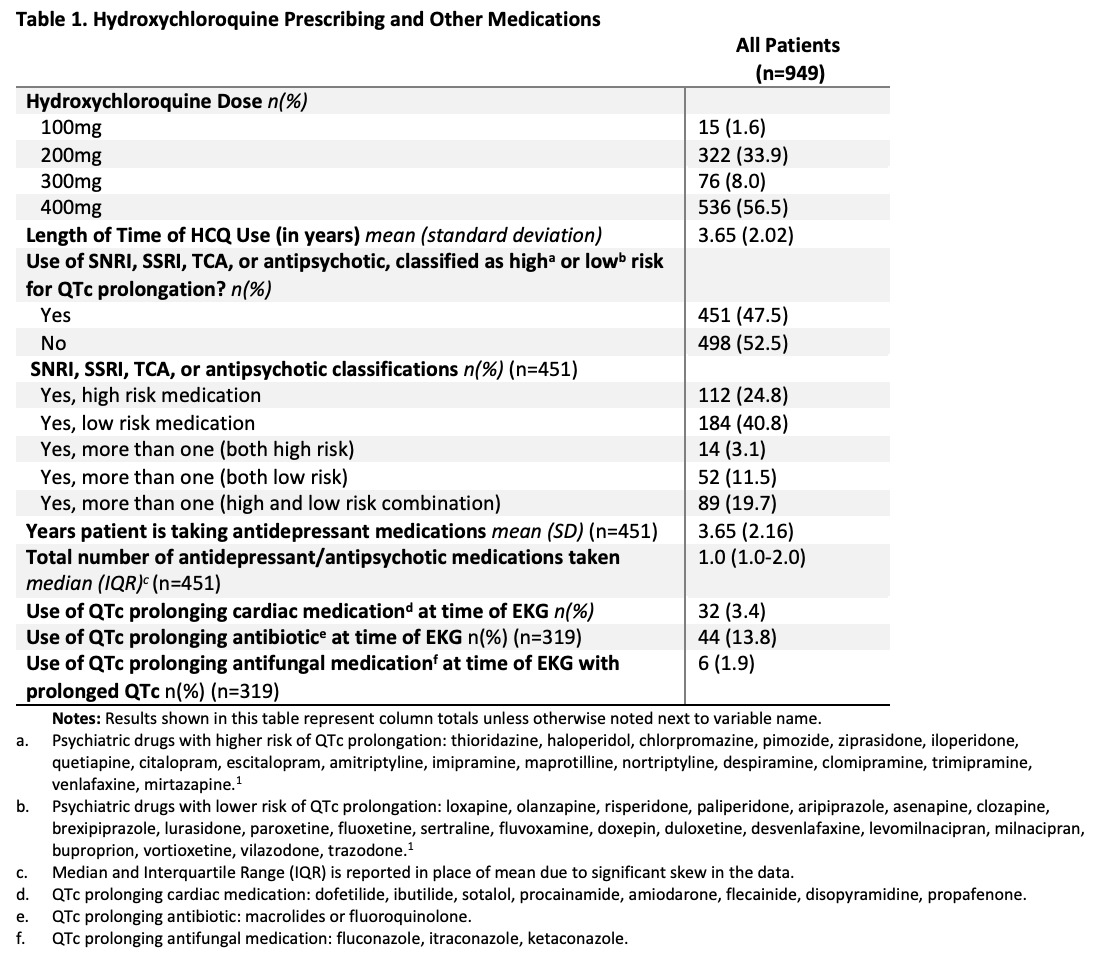 Table 1. Hydroxychloroquine Prescribing and Other Medications
Table 1. Hydroxychloroquine Prescribing and Other Medications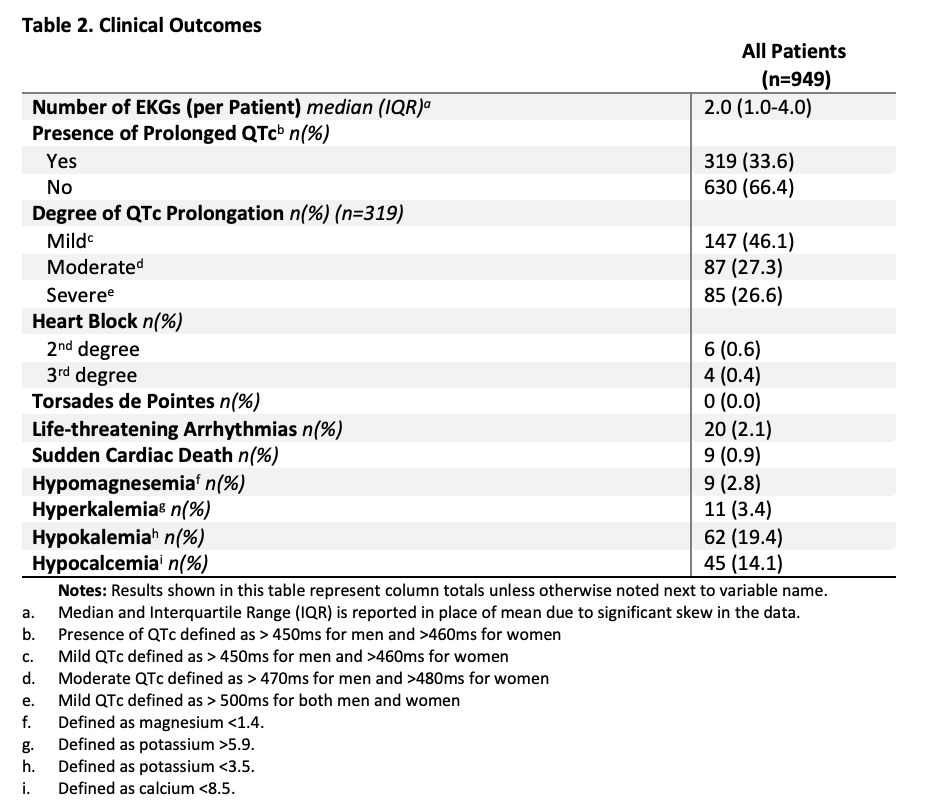 Table 2. Clinical Outcomes
Table 2. Clinical Outcomes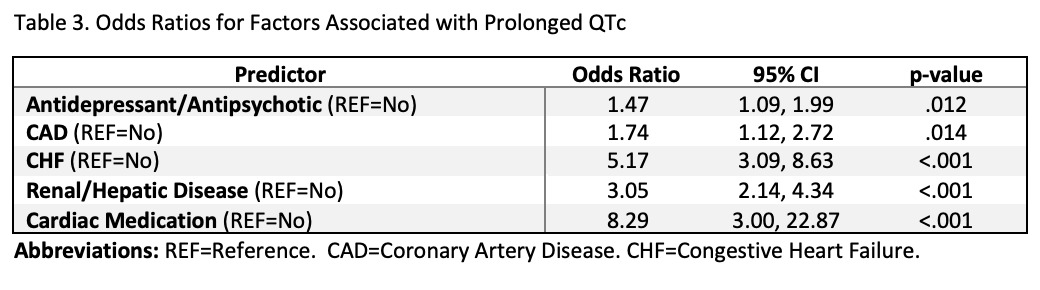 Table 3. Odds Ratio for Factors Associated with Prolonged QTc
Table 3. Odds Ratio for Factors Associated with Prolonged QTcDisclosures: K. Rudzinski, None; Z. Shahid, None; Y. kanakrieh, None; S. Goyal, None; K. Shaak, None; J. Ross, None.

