Back
Poster Session B
Session: (0807–0832) Miscellaneous Rheumatic and Inflammatory Diseases Poster II
0820: Therapeutic Practices and Outcomes of Chronic Sarcoidosis Arthropathy in the United States: A Nationwide Registry Study
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- DA
Diala Alawneh, MD
University of Illinois at Chicago
Chicago, IL, United States
Abstract Poster Presenter(s)
Diala Alawneh1, Moustafa Younis2, Bashar Alzghoul2, Christian Ascoli1, Tricha Shivas3, Mary McGowan3, Khaldoon Alawneh4, Divya Patel2, Israel Rubinstein1 and Nadera Sweiss1, 1University of Illinois at Chicago, Chicago, IL, 2University of Florida, Gainesville, FL, 3Foundation for Sarcoidosis Research, Chicago, IL, 4Jordan University of Science and Technology, Irbid, Jordan
Background/Purpose: Chronic arthropathy is a rare manifestation of sarcoidosis reported in only 0.2% of patients. However, treatment is challenging because no general consensus regarding appropriate therapy has been published. Accordingly, we sought to determine therapeutic practices and outcomes of patients with chronic sarcoidosis arthropathy in the United States (US) based on a national registry questionnaire.
Methods: We conducted a retrospective review of 3,835 respondents to the Foundation for Sarcoidosis Research - Sarcoidosis Advanced Registry for Cures Questionnaire (FSR-SARC). This US-based registry comprises of patient surveys completed between June 2014 and August 2019. Data is presented as means ± SD, odds ratio (OR) and confidence intervals (IR) where appropriate. Univariate data analyses were performed as indicated. P< 0.05 was considered statistically significant.
Results: A total of 773 (20%) patients with chronic sarcoidosis arthropathy with a mean (± SD) age of 42 (±12) years were identified; 634 (82%) were female, 578 (75%) Caucasian, and 161 (21%) African American. Among these, 713 (92%) had multiorgan involvement (defined as >=3 organs). Patients with chronic sarcoidosis arthropathy were 19 times more likely to have multiorgan involvement in comparison to those without (OR= 19; 95% CI: 14-25; p< 0.0001). These patients were more likely to be disabled (OR= 2.4; 95% CI: 2.0-2.8; p< 0.0001) and require mobility devices (OR= 2.5; 95% CI: 2.0-3.1; p< 0.0001). Patients with chronic sarcoidosis arthropathy had the following associated chronic disorders: 71 (11%) had Lofgren syndrome, 192 (25%) had fibromyalgia, 278 (36%) had chronic fatigue syndrome and 281 (37%) had chronic pain syndrome. Patients with chronic sarcoidosis arthropathy were 3.5 times more likely to have fibromyalgia (OR=3.5; 95% CI: 2.8-4.5; p< 0.0001).
A total of 690 (99%) patients received the following therapies during the course of their disease; 657 (85%) corticosteroids, 484 (80%) cytotoxic medications, and 186 (36%) TNF-α inhibitors. Patients with sarcoidosis arthropathy were actively on the following treatments: 505 (65%) acetaminophen/NSAIDS, 330 (43%) narcotics, 291 (38%) COX-2 inhibitors/ gabapentin/ pregabalin/ tramadol, 116 (15%) hydroxychloroquine, 34 (4%) corticosteroids, 153 (20%) methotrexate, 40 (5%) azathioprine, 25 (3%) leflunomide, 34 (4%) mycophenolate mofetil, 62 (8%) infliximab, 23 (3%) adalimumab, 7 (1%) rituximab, 4 (0.5%) cyclophosphamide, 16 (2%) IVIG, and 202 (26%) physical therapy.
Patients with chronic sarcoidosis arthropathy were more likely to be treated with corticosteroids, hydroxychloroquine, cytotoxic medications, and TNF-α inhibitors than those without chronic arthropathy as shown in figure 1 (all odds were statistically significant with p< 0.0001) .
Conclusion: The prevalence of chronic sarcoidosis arthropathy in this US cohort was similar to that reported in the literature. This condition is disabling and limits patient's activity of daily living. In addition, these patients are more likely to have multiorgan involvement. Corticosteroids, NSAIDs and hydroxychloroquine were the most commonly prescribed therapies.
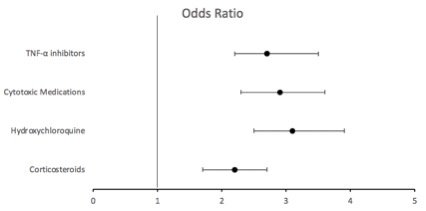 Figure 1: Odds of different therapies when comparing patients with sarcoidosis arthropathy vs those without.
Figure 1: Odds of different therapies when comparing patients with sarcoidosis arthropathy vs those without.
Disclosures: D. Alawneh, None; M. Younis, None; B. Alzghoul, None; C. Ascoli, None; T. Shivas, None; M. McGowan, None; K. Alawneh, None; D. Patel, None; I. Rubinstein, None; N. Sweiss, None.
Background/Purpose: Chronic arthropathy is a rare manifestation of sarcoidosis reported in only 0.2% of patients. However, treatment is challenging because no general consensus regarding appropriate therapy has been published. Accordingly, we sought to determine therapeutic practices and outcomes of patients with chronic sarcoidosis arthropathy in the United States (US) based on a national registry questionnaire.
Methods: We conducted a retrospective review of 3,835 respondents to the Foundation for Sarcoidosis Research - Sarcoidosis Advanced Registry for Cures Questionnaire (FSR-SARC). This US-based registry comprises of patient surveys completed between June 2014 and August 2019. Data is presented as means ± SD, odds ratio (OR) and confidence intervals (IR) where appropriate. Univariate data analyses were performed as indicated. P< 0.05 was considered statistically significant.
Results: A total of 773 (20%) patients with chronic sarcoidosis arthropathy with a mean (± SD) age of 42 (±12) years were identified; 634 (82%) were female, 578 (75%) Caucasian, and 161 (21%) African American. Among these, 713 (92%) had multiorgan involvement (defined as >=3 organs). Patients with chronic sarcoidosis arthropathy were 19 times more likely to have multiorgan involvement in comparison to those without (OR= 19; 95% CI: 14-25; p< 0.0001). These patients were more likely to be disabled (OR= 2.4; 95% CI: 2.0-2.8; p< 0.0001) and require mobility devices (OR= 2.5; 95% CI: 2.0-3.1; p< 0.0001). Patients with chronic sarcoidosis arthropathy had the following associated chronic disorders: 71 (11%) had Lofgren syndrome, 192 (25%) had fibromyalgia, 278 (36%) had chronic fatigue syndrome and 281 (37%) had chronic pain syndrome. Patients with chronic sarcoidosis arthropathy were 3.5 times more likely to have fibromyalgia (OR=3.5; 95% CI: 2.8-4.5; p< 0.0001).
A total of 690 (99%) patients received the following therapies during the course of their disease; 657 (85%) corticosteroids, 484 (80%) cytotoxic medications, and 186 (36%) TNF-α inhibitors. Patients with sarcoidosis arthropathy were actively on the following treatments: 505 (65%) acetaminophen/NSAIDS, 330 (43%) narcotics, 291 (38%) COX-2 inhibitors/ gabapentin/ pregabalin/ tramadol, 116 (15%) hydroxychloroquine, 34 (4%) corticosteroids, 153 (20%) methotrexate, 40 (5%) azathioprine, 25 (3%) leflunomide, 34 (4%) mycophenolate mofetil, 62 (8%) infliximab, 23 (3%) adalimumab, 7 (1%) rituximab, 4 (0.5%) cyclophosphamide, 16 (2%) IVIG, and 202 (26%) physical therapy.
Patients with chronic sarcoidosis arthropathy were more likely to be treated with corticosteroids, hydroxychloroquine, cytotoxic medications, and TNF-α inhibitors than those without chronic arthropathy as shown in figure 1 (all odds were statistically significant with p< 0.0001) .
Conclusion: The prevalence of chronic sarcoidosis arthropathy in this US cohort was similar to that reported in the literature. This condition is disabling and limits patient's activity of daily living. In addition, these patients are more likely to have multiorgan involvement. Corticosteroids, NSAIDs and hydroxychloroquine were the most commonly prescribed therapies.
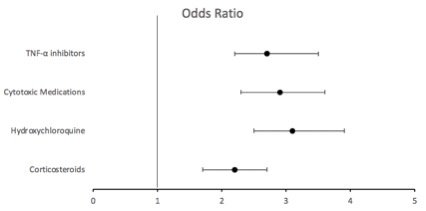 Figure 1: Odds of different therapies when comparing patients with sarcoidosis arthropathy vs those without.
Figure 1: Odds of different therapies when comparing patients with sarcoidosis arthropathy vs those without. Disclosures: D. Alawneh, None; M. Younis, None; B. Alzghoul, None; C. Ascoli, None; T. Shivas, None; M. McGowan, None; K. Alawneh, None; D. Patel, None; I. Rubinstein, None; N. Sweiss, None.

