Back
Poster Session B
Osteoarthritis (OA) and related disorders
Session: (0833–0849) Orthopedics, Low Back Pain, and Rehabilitation Poster
0834: Use of the Routine Assessment of Patient Index Data 3 (RAPID3) Questionnaire in the Assessment of Chronic Lower Back Pain
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- BT
Brendan Thoms, PhD, MBBS
University of Vermont Medical Center
South Burlington, VT, United States
Abstract Poster Presenter(s)
Brendan Thoms1, Bradley Tompkins2 and Chi Chi Lau1, 1University of Vermont Medical Center, Burlington, VT, 2University of Vermont, Burlington, VT
Background/Purpose: Chronic lower back pain (LBP) is a common primary care presentation with substantial socio-economic impact. There are several indices to measure pain / function from LBP. The Oswestry Disability Index (ODI) is a well-regarded tool for assessing lower back pain / function and to detect clinical improvement. The Routine Assessment of Patient Index Data 3 (RAPID3) questionnaire, known for its ease of use in assessing rheumatoid arthritis, has been reported to parallel measures for other rheumatologic conditions, but has not yet been applied to LBP. It would be useful for rheumatology practices to have a score that could be followed for inflammatory and non-inflammatory conditions. Our objective was to measure back pain and function in patients over 36-weeks receiving routine care using the RAPID3 questionnaire / ODI and assess for a correlation.
Methods: We performed a prospective study of adults with greater than 3 months of LBP receiving routine care from Primary Care or Rheumatology clinics at the University of Vermont Medical Center. Patient pain and function were measured at baseline, 4-, 12- and 36-weeks using the RAPID3 questionnaire and ODI completed at each clinic visit. Regression analysis was used to assess for a correlation between RAPID3 as the dependent variable and ODI.
Results: Of 85 participants who completed both questionnaires at week 0, the majority were female (n = 60, median age 51) and attended rheumatology clinic (92%). The most frequent underlying diagnoses associated with chronic LBP were: Degenerative disk disease / facet joint arthritis (50.4%), Seronegative spondylarthropathies (25.2%) and Fibromyalgia (13%). At baseline, 4-, 12- or 36-weeks there was a significant direct correlation between ODI and RAPID3 scores with the correlation coefficients ranging between 0.45 – 0.59 (meaning for each 1 point rise in ODI score, the Rapid3 score increased by 0.45 - 0.59) depending on the timepoint (Fig 1, Table 1). There was no significant difference in RAPID3 or ODI scores between baseline to 4-, 12- or 36-weeks in response to routine care.
Conclusion: RAPID3 correlated significantly with the ODI over a 36 week observation period. Therefore the RAPID3 may be a useful tool to assess LBP along with other rheumatologic conditions. LBP did not improve significantly over 36-weeks as a result of routine care, thus we were unable to assess the validity of the RAPID3 in detecting clinical LBP improvement.
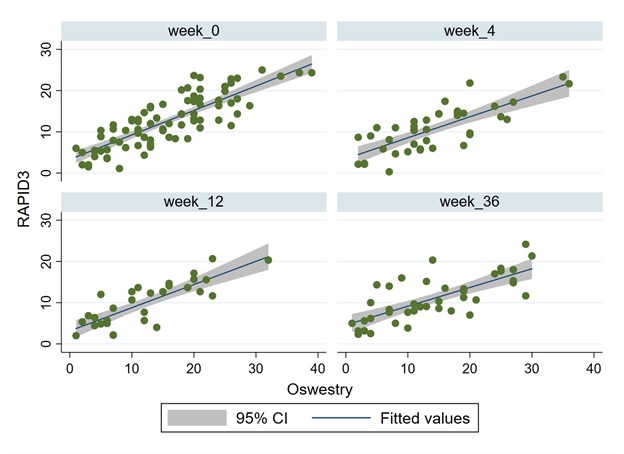 Figure 1. Regression analysis of Routine Assessment of Patient Index Data 3 (RAPID3) to Oswestry Disability Index (ODI) scores in patients with chronic lower back pain receiving routine care at week 0, week 4, week 12 and week 36.
Figure 1. Regression analysis of Routine Assessment of Patient Index Data 3 (RAPID3) to Oswestry Disability Index (ODI) scores in patients with chronic lower back pain receiving routine care at week 0, week 4, week 12 and week 36.
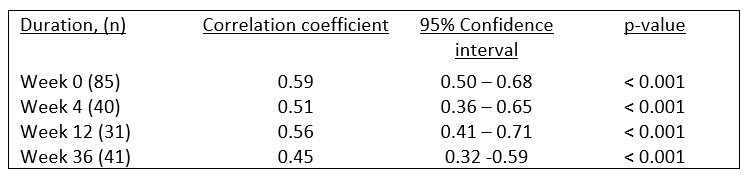 Table 1. Correlation coefficients between ODI and RAPID3 scores at baseline, 4-, 12- and 36-weeks.
Table 1. Correlation coefficients between ODI and RAPID3 scores at baseline, 4-, 12- and 36-weeks.
Disclosures: B. Thoms, None; B. Tompkins, None; C. Lau, None.
Background/Purpose: Chronic lower back pain (LBP) is a common primary care presentation with substantial socio-economic impact. There are several indices to measure pain / function from LBP. The Oswestry Disability Index (ODI) is a well-regarded tool for assessing lower back pain / function and to detect clinical improvement. The Routine Assessment of Patient Index Data 3 (RAPID3) questionnaire, known for its ease of use in assessing rheumatoid arthritis, has been reported to parallel measures for other rheumatologic conditions, but has not yet been applied to LBP. It would be useful for rheumatology practices to have a score that could be followed for inflammatory and non-inflammatory conditions. Our objective was to measure back pain and function in patients over 36-weeks receiving routine care using the RAPID3 questionnaire / ODI and assess for a correlation.
Methods: We performed a prospective study of adults with greater than 3 months of LBP receiving routine care from Primary Care or Rheumatology clinics at the University of Vermont Medical Center. Patient pain and function were measured at baseline, 4-, 12- and 36-weeks using the RAPID3 questionnaire and ODI completed at each clinic visit. Regression analysis was used to assess for a correlation between RAPID3 as the dependent variable and ODI.
Results: Of 85 participants who completed both questionnaires at week 0, the majority were female (n = 60, median age 51) and attended rheumatology clinic (92%). The most frequent underlying diagnoses associated with chronic LBP were: Degenerative disk disease / facet joint arthritis (50.4%), Seronegative spondylarthropathies (25.2%) and Fibromyalgia (13%). At baseline, 4-, 12- or 36-weeks there was a significant direct correlation between ODI and RAPID3 scores with the correlation coefficients ranging between 0.45 – 0.59 (meaning for each 1 point rise in ODI score, the Rapid3 score increased by 0.45 - 0.59) depending on the timepoint (Fig 1, Table 1). There was no significant difference in RAPID3 or ODI scores between baseline to 4-, 12- or 36-weeks in response to routine care.
Conclusion: RAPID3 correlated significantly with the ODI over a 36 week observation period. Therefore the RAPID3 may be a useful tool to assess LBP along with other rheumatologic conditions. LBP did not improve significantly over 36-weeks as a result of routine care, thus we were unable to assess the validity of the RAPID3 in detecting clinical LBP improvement.
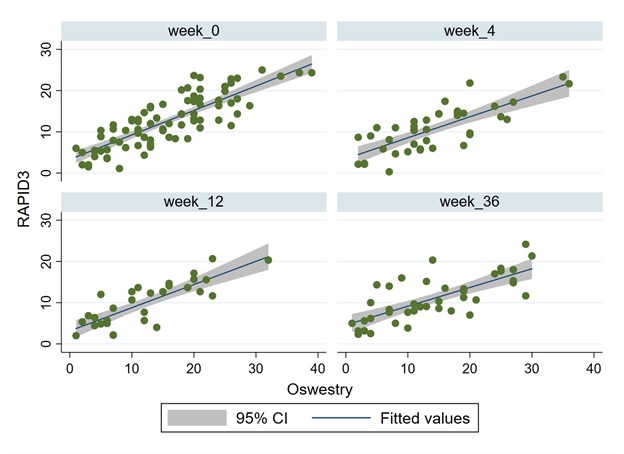 Figure 1. Regression analysis of Routine Assessment of Patient Index Data 3 (RAPID3) to Oswestry Disability Index (ODI) scores in patients with chronic lower back pain receiving routine care at week 0, week 4, week 12 and week 36.
Figure 1. Regression analysis of Routine Assessment of Patient Index Data 3 (RAPID3) to Oswestry Disability Index (ODI) scores in patients with chronic lower back pain receiving routine care at week 0, week 4, week 12 and week 36.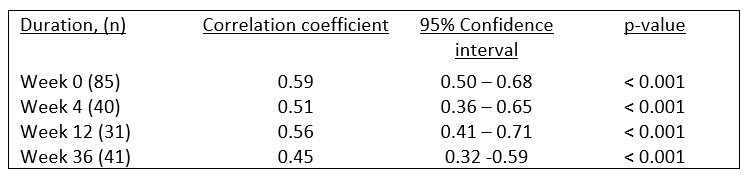 Table 1. Correlation coefficients between ODI and RAPID3 scores at baseline, 4-, 12- and 36-weeks.
Table 1. Correlation coefficients between ODI and RAPID3 scores at baseline, 4-, 12- and 36-weeks.Disclosures: B. Thoms, None; B. Tompkins, None; C. Lau, None.

