Back
Ignite Talk
Session: Ignite Session 4C
0957: Timeliness of Fetal Echocardiography for Congenital Heart Block Detection in Anti-Ro/La-Positive Pregnancies
Sunday, November 13, 2022
10:25 AM – 10:30 AM Eastern Time
Location: South Philly Stage
- AO
Amanda Ohayon, BSc, MSc
McGill
Montréal, QC, CanadaDisclosure: Disclosure information not submitted.
Ignite Speaker(s)
Amanda Ohayon1, Nikola Wilk1, Arielle Mendel2, Mayssa Moukarzel1, Jessica Simoneau1, Wadi Mawad1, Gabriel Altit1 and Evelyne Vinet2, 1McGill University Health Center, Montréal, QC, Canada, 2McGill University Health Centre, Montréal, QC, Canada
Background/Purpose: Best practice guidelines recommend screening for congenital heart block (CHB) in anti-Ro/La-positive pregnancies with serial echocardiography starting between 16 to 18 weeks of gestational age (GA). As the most vulnerable period for CHB is from 18 to 24 weeks and early detection may improve outcomes, we evaluated timing of: 1) first fetal echocardiography for CHB screening, and 2) CHB detection in anti-Ro/La pregnancies at our institution.
Methods: We retrospectively identified all pregnancies undergoing fetal echocardiography for CHB screening and/or diagnosis between 2013 to 2021 at the McGill University Health Centre, using an electronic database. We included those with anti-Ro/La antibodies as ascertained by chart review. In pregnancies referred for CHB screening, we estimated GA at the first and last fetal echocardiography based on the date of the last menstrual period recorded at the first trimester obstetrical visit. For all CHB cases occurring during the study interval (including incidental cases not detected by screening), we also determined GA at echocardiographic detection of CHB.
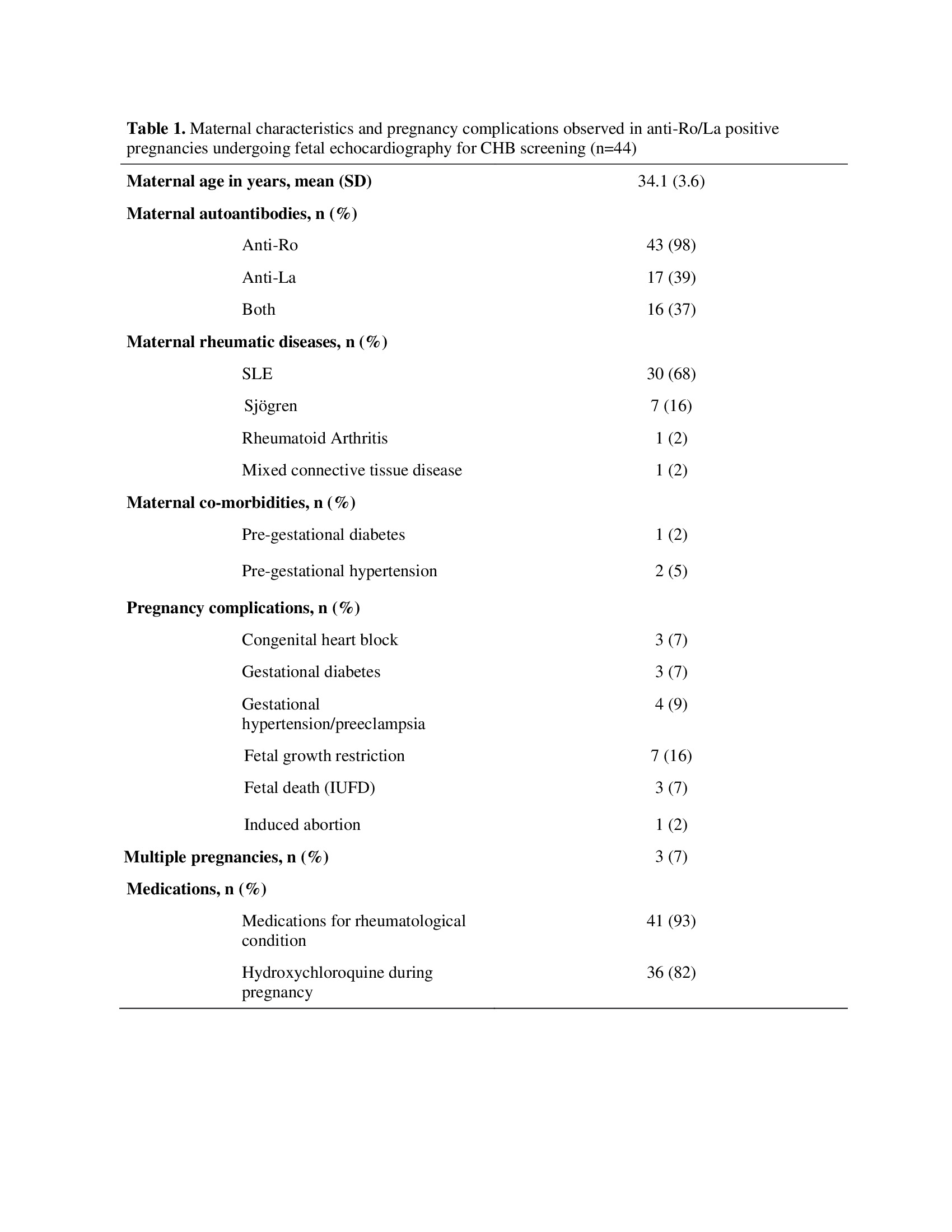
Results: We identified 44 pregnancies (including 3 twin pregnancies), with 98% exposed to anti-Ro and 39% to anti-La (Table 1). Mean maternal age at first fetal echocardiography was 34.1 (standard deviation, SD 3.6) years. Majority of pregnancies occurred in SLE women (68%) and most (82%) were exposed to hydroxychloroquine. Mean GA at first fetal echocardiography was 20.4 (SD 2.8) weeks, with 32% of echocardiographies performed at ≤18 weeks, 55% at < 20 weeks and 91% at < 22 weeks (Table 2). Four pregnancies had only one fetal echocardiography throughout pregnancy: two due to late GA at first screen (30.6 and 29.1 weeks) and two due to pregnancy loss. In the 42 pregnancies with ≥2 fetal echocardiographies, last screen was at a mean of 31.5 (SD 2.8) weeks of GA. Over the study period, CHB was detected in 3/47 (6%) fetuses undergoing screening, all on their first echocardiography at 19.0, 22.4 and 29.3 weeks, respectively. Two other CHB cases were referred for echocardiography at 20.3 and 23.4 weeks of GA after incidental finding of bradycardia, with subsequent testing confirming maternal anti-Ro/La antibodies. Only one fetus (who was undergoing CHB screening) reversed from a 3rd-degree atrioventricular block (AVB) to a 1st-degree AVB after receiving dexamethasone. The other four CHB fetuses remained in 3rd-degree AVB throughout pregnancy.
Conclusion: We observed that most fetal echocardiography screening for CHB in anti-Ro/La pregnancies did not occur by the recommended 16 to 18 weeks of GA. This represents an important potential care gap as all CHB were present on the first fetal echocardiography, and all were already 3rd-degree. Despite this, one fetus (out of five CHB cases) reversed from 3rd to 1st-degree AVB after dexamethasone. Timely initial screening (between 16 to 18 weeks) and/or alternative diagnostic approach might be necessary to detect earlier reversible cardiac involvement in anti-Ro/La-positive pregnancies.
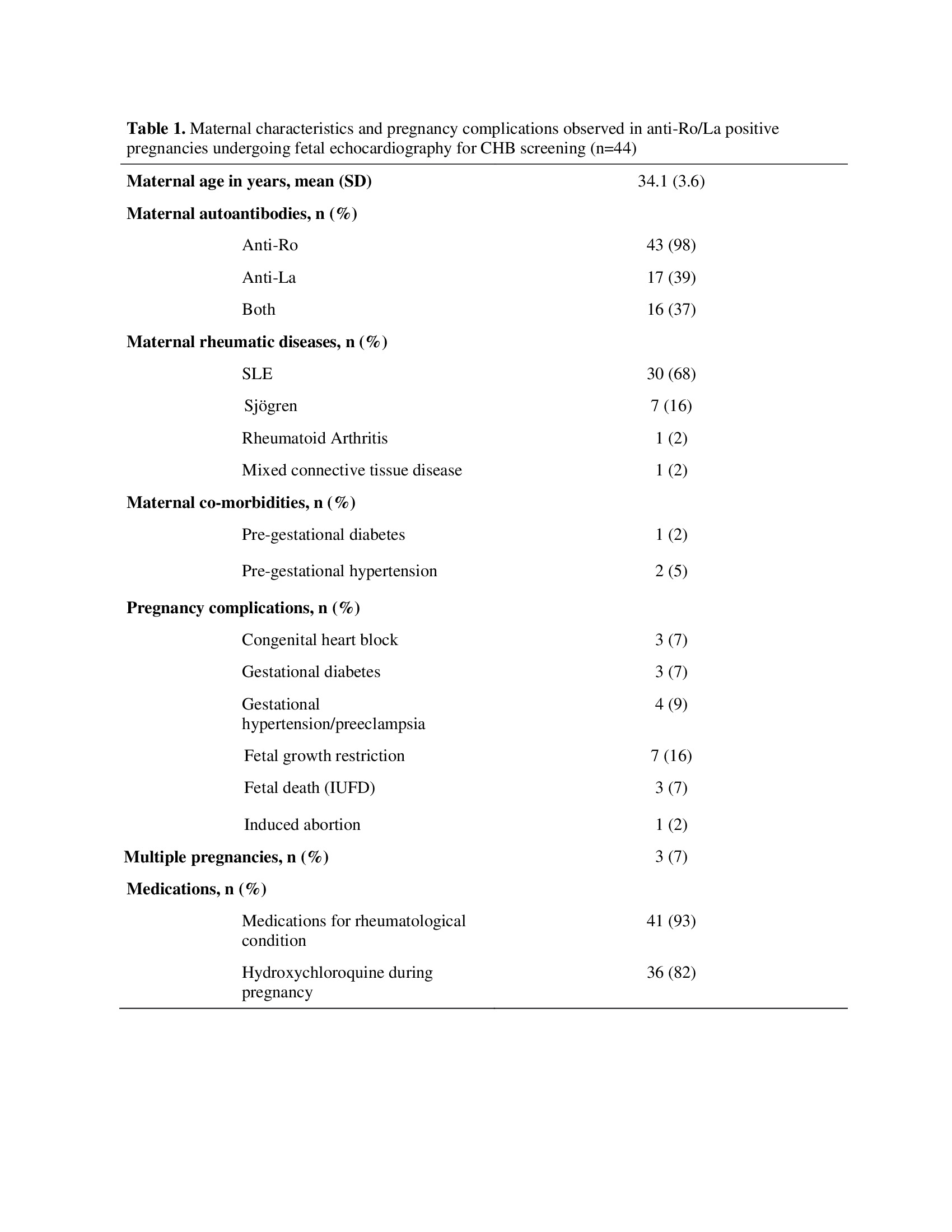 Legend: Categorical results are expressed as count (%). Continuous results are expressed as mean (SD). SD: standard deviation; SLE: Systemic Lupus Erythematosus; IUFD: Intrauterine Fetal Demise.
Legend: Categorical results are expressed as count (%). Continuous results are expressed as mean (SD). SD: standard deviation; SLE: Systemic Lupus Erythematosus; IUFD: Intrauterine Fetal Demise.
.jpg) Legend: Categorical results are expressed as count (%). Continuous results are expressed as mean (SD) or median (interquartile range). GA: Gestational Age; SD: standard deviation; IQR: interquartile range.
Legend: Categorical results are expressed as count (%). Continuous results are expressed as mean (SD) or median (interquartile range). GA: Gestational Age; SD: standard deviation; IQR: interquartile range.
Disclosures: A. Ohayon, None; N. Wilk, None; A. Mendel, None; M. Moukarzel, None; J. Simoneau, None; W. Mawad, None; G. Altit, None; E. Vinet, None.
Background/Purpose: Best practice guidelines recommend screening for congenital heart block (CHB) in anti-Ro/La-positive pregnancies with serial echocardiography starting between 16 to 18 weeks of gestational age (GA). As the most vulnerable period for CHB is from 18 to 24 weeks and early detection may improve outcomes, we evaluated timing of: 1) first fetal echocardiography for CHB screening, and 2) CHB detection in anti-Ro/La pregnancies at our institution.
Methods: We retrospectively identified all pregnancies undergoing fetal echocardiography for CHB screening and/or diagnosis between 2013 to 2021 at the McGill University Health Centre, using an electronic database. We included those with anti-Ro/La antibodies as ascertained by chart review. In pregnancies referred for CHB screening, we estimated GA at the first and last fetal echocardiography based on the date of the last menstrual period recorded at the first trimester obstetrical visit. For all CHB cases occurring during the study interval (including incidental cases not detected by screening), we also determined GA at echocardiographic detection of CHB.
Results: We identified 44 pregnancies (including 3 twin pregnancies), with 98% exposed to anti-Ro and 39% to anti-La (Table 1). Mean maternal age at first fetal echocardiography was 34.1 (standard deviation, SD 3.6) years. Majority of pregnancies occurred in SLE women (68%) and most (82%) were exposed to hydroxychloroquine. Mean GA at first fetal echocardiography was 20.4 (SD 2.8) weeks, with 32% of echocardiographies performed at ≤18 weeks, 55% at < 20 weeks and 91% at < 22 weeks (Table 2). Four pregnancies had only one fetal echocardiography throughout pregnancy: two due to late GA at first screen (30.6 and 29.1 weeks) and two due to pregnancy loss. In the 42 pregnancies with ≥2 fetal echocardiographies, last screen was at a mean of 31.5 (SD 2.8) weeks of GA. Over the study period, CHB was detected in 3/47 (6%) fetuses undergoing screening, all on their first echocardiography at 19.0, 22.4 and 29.3 weeks, respectively. Two other CHB cases were referred for echocardiography at 20.3 and 23.4 weeks of GA after incidental finding of bradycardia, with subsequent testing confirming maternal anti-Ro/La antibodies. Only one fetus (who was undergoing CHB screening) reversed from a 3rd-degree atrioventricular block (AVB) to a 1st-degree AVB after receiving dexamethasone. The other four CHB fetuses remained in 3rd-degree AVB throughout pregnancy.
Conclusion: We observed that most fetal echocardiography screening for CHB in anti-Ro/La pregnancies did not occur by the recommended 16 to 18 weeks of GA. This represents an important potential care gap as all CHB were present on the first fetal echocardiography, and all were already 3rd-degree. Despite this, one fetus (out of five CHB cases) reversed from 3rd to 1st-degree AVB after dexamethasone. Timely initial screening (between 16 to 18 weeks) and/or alternative diagnostic approach might be necessary to detect earlier reversible cardiac involvement in anti-Ro/La-positive pregnancies.
 Legend: Categorical results are expressed as count (%). Continuous results are expressed as mean (SD). SD: standard deviation; SLE: Systemic Lupus Erythematosus; IUFD: Intrauterine Fetal Demise.
Legend: Categorical results are expressed as count (%). Continuous results are expressed as mean (SD). SD: standard deviation; SLE: Systemic Lupus Erythematosus; IUFD: Intrauterine Fetal Demise..jpg) Legend: Categorical results are expressed as count (%). Continuous results are expressed as mean (SD) or median (interquartile range). GA: Gestational Age; SD: standard deviation; IQR: interquartile range.
Legend: Categorical results are expressed as count (%). Continuous results are expressed as mean (SD) or median (interquartile range). GA: Gestational Age; SD: standard deviation; IQR: interquartile range. Disclosures: A. Ohayon, None; N. Wilk, None; A. Mendel, None; M. Moukarzel, None; J. Simoneau, None; W. Mawad, None; G. Altit, None; E. Vinet, None.

