Back
Abstract Session
Session: Abstracts: Miscellaneous Rheumatic and Inflammatory Diseases II (1106–1111)
1108: Abnormal Baseline Chest CT Shows Increased Risk for Immune Checkpoint Inhibitor Associated Pneumonitis
Sunday, November 13, 2022
11:00 AM – 11:10 AM Eastern Time
Location: Room 119
Pankti Reid, MD, MPH
University of Chicago Medical Center
Chicago, IL, United States
Presenting Author(s)
Danielle Stahlbaum1, Renea Jablonski1, Mary Strek2 and Pankti Reid1, 1University of Chicago Medical Center, Chicago, IL, 2University of Chicago, Chicago, IL
Background/Purpose: Immune checkpoint inhibitors (ICIs) have revolutionized cancer therapy but can result in off-target toxicities known as immune-related adverse events (irAEs). With increased use of ICIs, ICI-associated pneumonitis (ICI-pneumonitis) has been more commonly recognized and can be fatal. We sought to identify predictors for the development of ICI-pneumonitis with a focus on pulmonary specific risk factors.
Methods: We conducted a retrospective cohort study of patients with ICI treatment for cancer at a tertiary referral hospital from 2015 to 2019. ICI-pneumonitis was determined by the treating physician with corroboration via an independent physician specialist with expertise in irAEs and exclusion of alternative etiologies prior to case inclusion. Controls were patients treated with ICI without a diagnosis of ICI-pneumonitis. The most proximal chest CT imaging within 3 months prior to ICI therapy was reviewed. Chi-squared tests for categorical data, Student's t-tests for continuous data, and univariate logistic regression were used for statistical analysis.
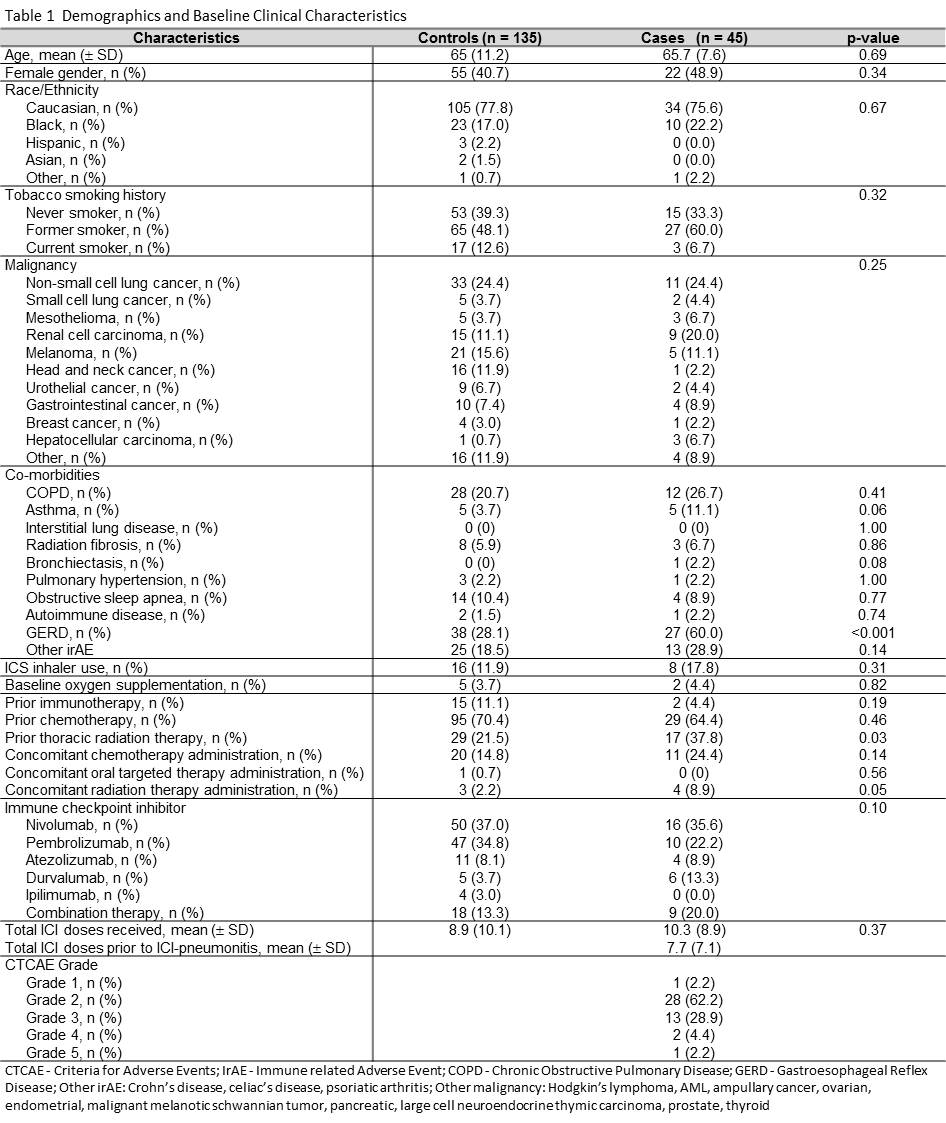
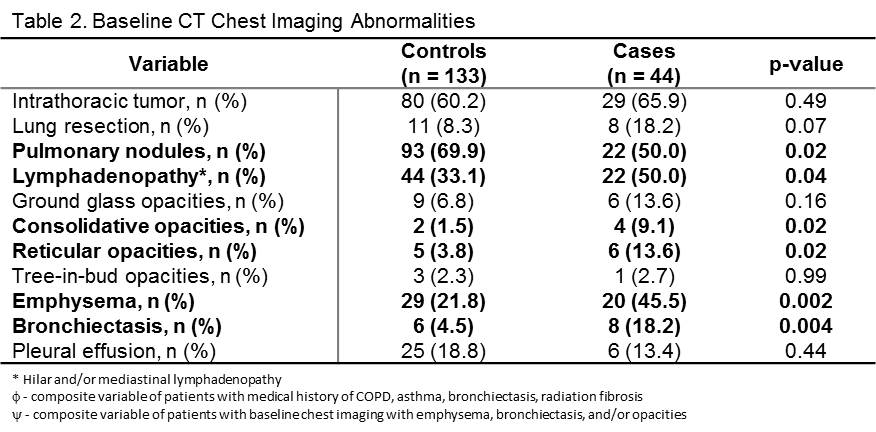
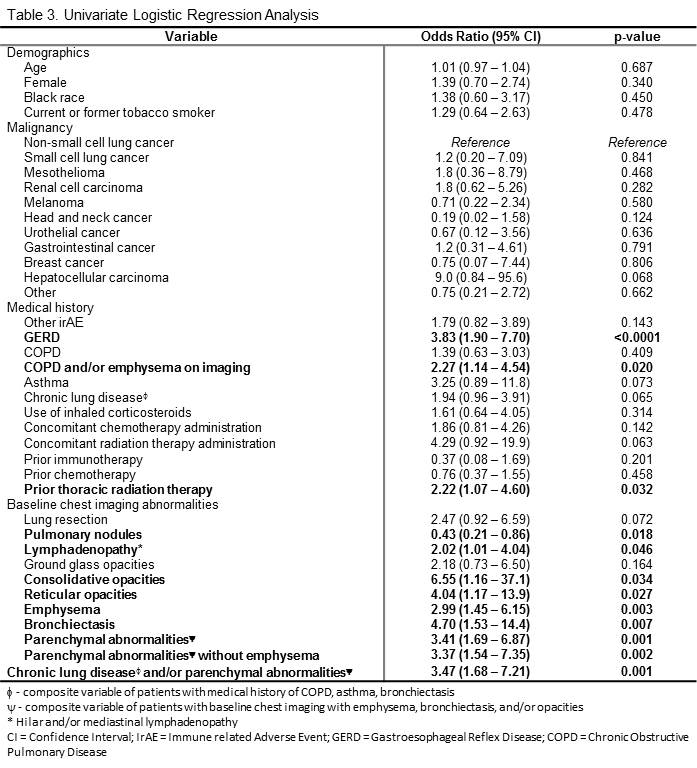
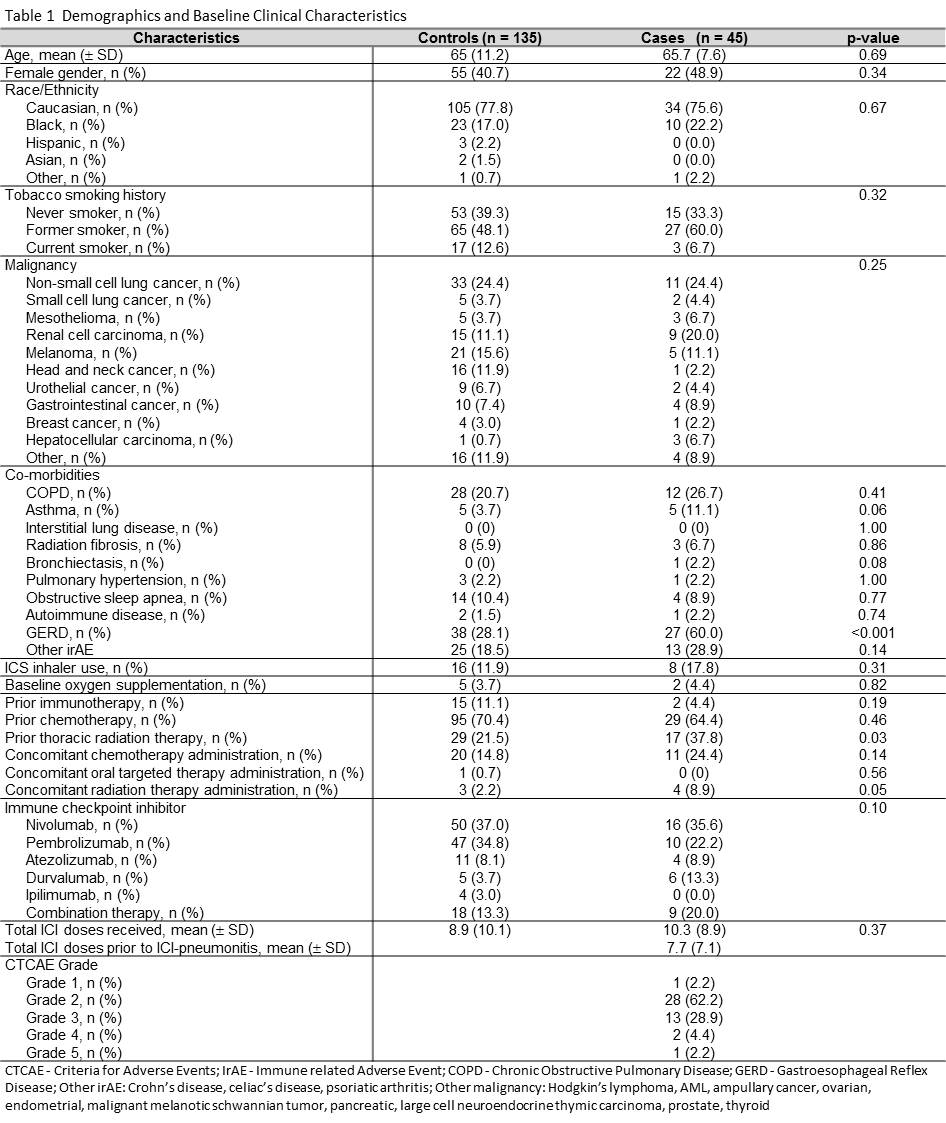
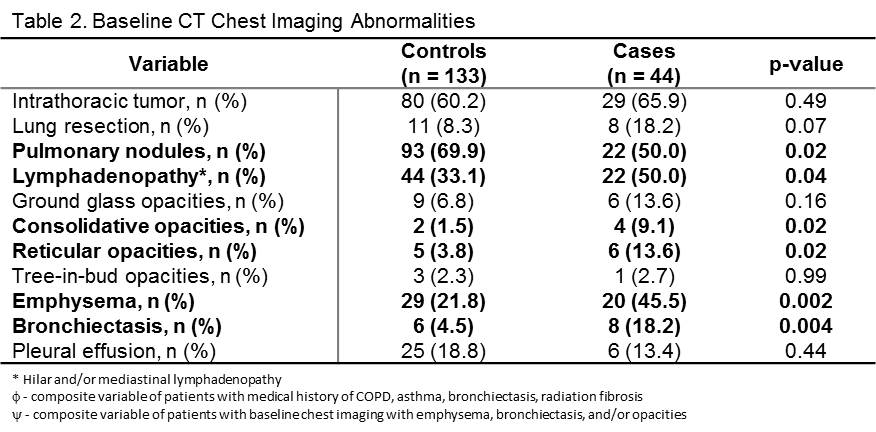
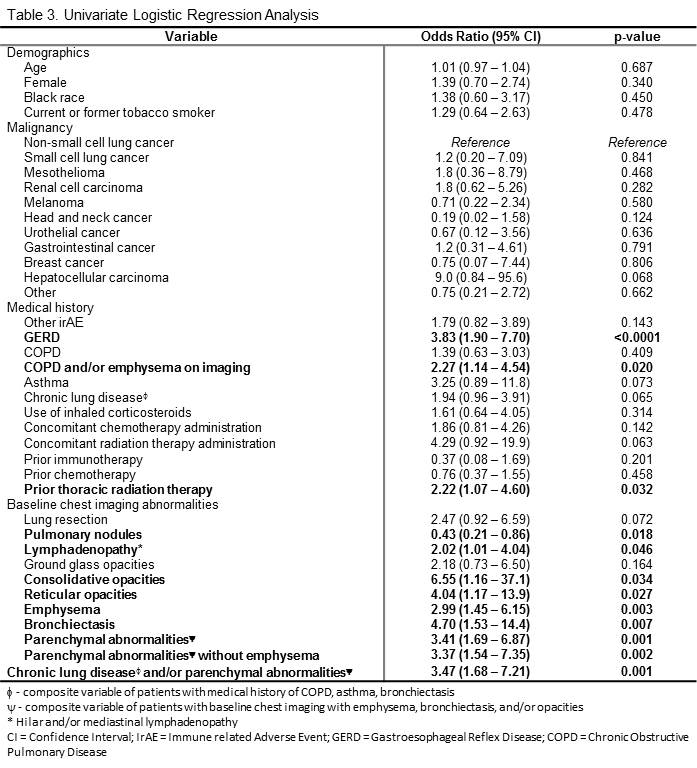
Results: We analyzed 45 cases of ICI-pneumonitis and 135 controls (Table 1). Patients with abnormal baseline chest CT imaging (emphysema; bronchiectasis; reticular, ground glass and/or consolidative opacities) (Table 2) had increased risk for ICI-pneumonitis (OR 3.41, 95%CI: 1.68 – 6.87, p = 0.001). Patients with baseline hilar and/or mediastinal lymphadenopathy had a two-fold higher risk for ICI-pneumonitis (OR 2.02, 95%CI 1.01 - 4.04, p = 0.046). There was also an association between development of ICI-pneumonitis with that of prior thoracic radiation (OR 2.22, 95%CI: 1.07 – 4.60, p = 0.032) and chronic obstructive pulmonary disease (COPD) and/or emphysema on imaging (OR 2.27, 95%CI: 1.14 – 4.54, p = 0.020). Patients with gastroesophageal reflux disease (GERD) had increased risk for ICI-pneumonitis (OR 3.83, 95%CI: 1.90 – 7.70, p = < 0.0001). Other potential risk factors including race, primary malignancy, smoking history, inhaled corticosteroid use, and diagnosis of another irAE were not statistically significant (Table 3). Twenty-five percent of all patients (32/124 total; 13/26 cases, 19/98 controls) had abnormal baseline chest CT consistent with chronic lung disease without a documented diagnosis. All patients with ICI-pneumonitis patients were treated with systemic corticosteroids with 22% (10/45) requiring prolonged taper or multiple courses. Eighty percent (8/10) of the patients requiring extended steroid therapy had comorbid pulmonary disease and/or abnormal baseline chest imaging.
Conclusion: Patients with baseline chest CT abnormalities, suggesting the presence of undiagnosed ILD, GERD, prior radiation or COPD, were at increased risk for developing ICI-pneumonitis. The large proportion of patients with baseline radiographic abnormalities without a clinical diagnosis of chronic lung disease highlights the importance of timely, multidisciplinary evaluation prior to ICI initiation. Future research should assess the safety and outcome of ICI use for patients with autoimmune lung disease as well as best practices for identification of high-risk patients prior to consideration of ICI therapy.
Disclosures: D. Stahlbaum, None; R. Jablonski, None; M. Strek, None; P. Reid, provisional patent.
Background/Purpose: Immune checkpoint inhibitors (ICIs) have revolutionized cancer therapy but can result in off-target toxicities known as immune-related adverse events (irAEs). With increased use of ICIs, ICI-associated pneumonitis (ICI-pneumonitis) has been more commonly recognized and can be fatal. We sought to identify predictors for the development of ICI-pneumonitis with a focus on pulmonary specific risk factors.
Methods: We conducted a retrospective cohort study of patients with ICI treatment for cancer at a tertiary referral hospital from 2015 to 2019. ICI-pneumonitis was determined by the treating physician with corroboration via an independent physician specialist with expertise in irAEs and exclusion of alternative etiologies prior to case inclusion. Controls were patients treated with ICI without a diagnosis of ICI-pneumonitis. The most proximal chest CT imaging within 3 months prior to ICI therapy was reviewed. Chi-squared tests for categorical data, Student's t-tests for continuous data, and univariate logistic regression were used for statistical analysis.
Results: We analyzed 45 cases of ICI-pneumonitis and 135 controls (Table 1). Patients with abnormal baseline chest CT imaging (emphysema; bronchiectasis; reticular, ground glass and/or consolidative opacities) (Table 2) had increased risk for ICI-pneumonitis (OR 3.41, 95%CI: 1.68 – 6.87, p = 0.001). Patients with baseline hilar and/or mediastinal lymphadenopathy had a two-fold higher risk for ICI-pneumonitis (OR 2.02, 95%CI 1.01 - 4.04, p = 0.046). There was also an association between development of ICI-pneumonitis with that of prior thoracic radiation (OR 2.22, 95%CI: 1.07 – 4.60, p = 0.032) and chronic obstructive pulmonary disease (COPD) and/or emphysema on imaging (OR 2.27, 95%CI: 1.14 – 4.54, p = 0.020). Patients with gastroesophageal reflux disease (GERD) had increased risk for ICI-pneumonitis (OR 3.83, 95%CI: 1.90 – 7.70, p = < 0.0001). Other potential risk factors including race, primary malignancy, smoking history, inhaled corticosteroid use, and diagnosis of another irAE were not statistically significant (Table 3). Twenty-five percent of all patients (32/124 total; 13/26 cases, 19/98 controls) had abnormal baseline chest CT consistent with chronic lung disease without a documented diagnosis. All patients with ICI-pneumonitis patients were treated with systemic corticosteroids with 22% (10/45) requiring prolonged taper or multiple courses. Eighty percent (8/10) of the patients requiring extended steroid therapy had comorbid pulmonary disease and/or abnormal baseline chest imaging.
Conclusion: Patients with baseline chest CT abnormalities, suggesting the presence of undiagnosed ILD, GERD, prior radiation or COPD, were at increased risk for developing ICI-pneumonitis. The large proportion of patients with baseline radiographic abnormalities without a clinical diagnosis of chronic lung disease highlights the importance of timely, multidisciplinary evaluation prior to ICI initiation. Future research should assess the safety and outcome of ICI use for patients with autoimmune lung disease as well as best practices for identification of high-risk patients prior to consideration of ICI therapy.
Disclosures: D. Stahlbaum, None; R. Jablonski, None; M. Strek, None; P. Reid, provisional patent.

