Back
Poster Session C
Systemic lupus erythematosus (SLE)
Session: (1440–1485) SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
1468: Apathy Measurement in a Cohort of Systemic Lupus Erythematosus
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- IM
Ikechukwu Mbonu, MD
Ikechukwu Mbonu
Virginia Beach, VA, United States
Abstract Poster Presenter(s)
Mike Putman1, David Gazeley2 and Ikechukwu Mbonu3, 1The Medical College of Wisconsin, Milwaukee, WI, 2Medical College of Wisconsin, Wauwatosa, WI, 3Medical College of Wisconsin, Milwaukee, WI
Background/Purpose: Up to 40% of patients with systemic lupus erythematosus (SLE) have measurable cognitive dysfunction on neuropsychiatric testing. Around 83% of patients are nonadherent with hydroxychloroquine (HCQ), a foundational and well tolerated medication in lupus treatment. We hypothesized that many more patients experience some form of cognitive dysfunction that contributes to medication nonadherence. In Parkinson's disease, apathy has been associated with functional decline, medication nonadherence, poor executive function and lower quality of life. No prior studies have investigated apathy in a prospective cohort of patients with SLE.
Methods: Adult, English-speaking patients ≥18 years old with SLE were consecutively approached to participate. For comparator groups, patients with inflammatory bowel disease (IBD) were recruited at Medical College of Wisconsin (MCW) gastroenterology clinic and healthy controls were recruited from a MCW Sports Medicine clinic. Patients completed the Apathy Evaluation Scale (AES), a validated 18 item, self-administered survey. Scores on the survey range from 18-72, with higher scores suggesting higher level of apathy. A score of 31 was used to dichotomize the score into apathy-present or apathy-absent. Adherence to HCQ levels were defined by a serum level of 500 ng/ml at baseline. Categorical variables were compared using Fishers exact test, bivariate differences in apathy were assessed using a one-way ANOVA, the dichotomized apathy score evaluated in a logistic regression model that controlled for age, gender, and race/ethnicity, and the association between HCQ serum levels and apathy were analyzed in a linear regression.
Results: In total 107 patients were enrolled (47 SLE, 30 IBD, 30 healthy controls). Patients with SLE were more likely to be female (93% SLE vs. 43% IBD vs. 67% healthy controls, p < 0.01), Black/African American (60% SLE vs. 3% IBD vs. 7% healthy controls, p < 0.01), and single, not married (55% SLE vs. 33% IBD vs. 10% healthy controls, p < 0.01). The overall mean apathy score was 26.8 with a standard deviation (SD) of 6.1; higher apathy scores were observed in patients with SLE (30.3 +/- 3.8 SLE vs. 25.3 +/- 5.4 IBD vs. 23.9 +/- 3.8 healthy controls, p < 0.01). In a logistic regression model that evaluated apathy as a dichotomous variable, patients with SLE had higher adjusted odds of apathy as compared to healthy controls (OR 5.1, CI 1.1-29.8). Four out of 32 patients (12%) were adherent to HCQ when defined by baseline serum HCQ levels ≥500 ng/ml. In a linear regression model of the SLE cohort, HCQ serum levels decreased by 0.017 ng/ml for every increase of 1 on the apathy scale (p = 0.02).
Conclusion: In this study, patients with SLE had higher levels of apathy as compared to healthy controls. Lower serum HCQ levels correlated with higher measured apathy level. Future studies should confirm these preliminary findings and may investigate interventions to address apathy.
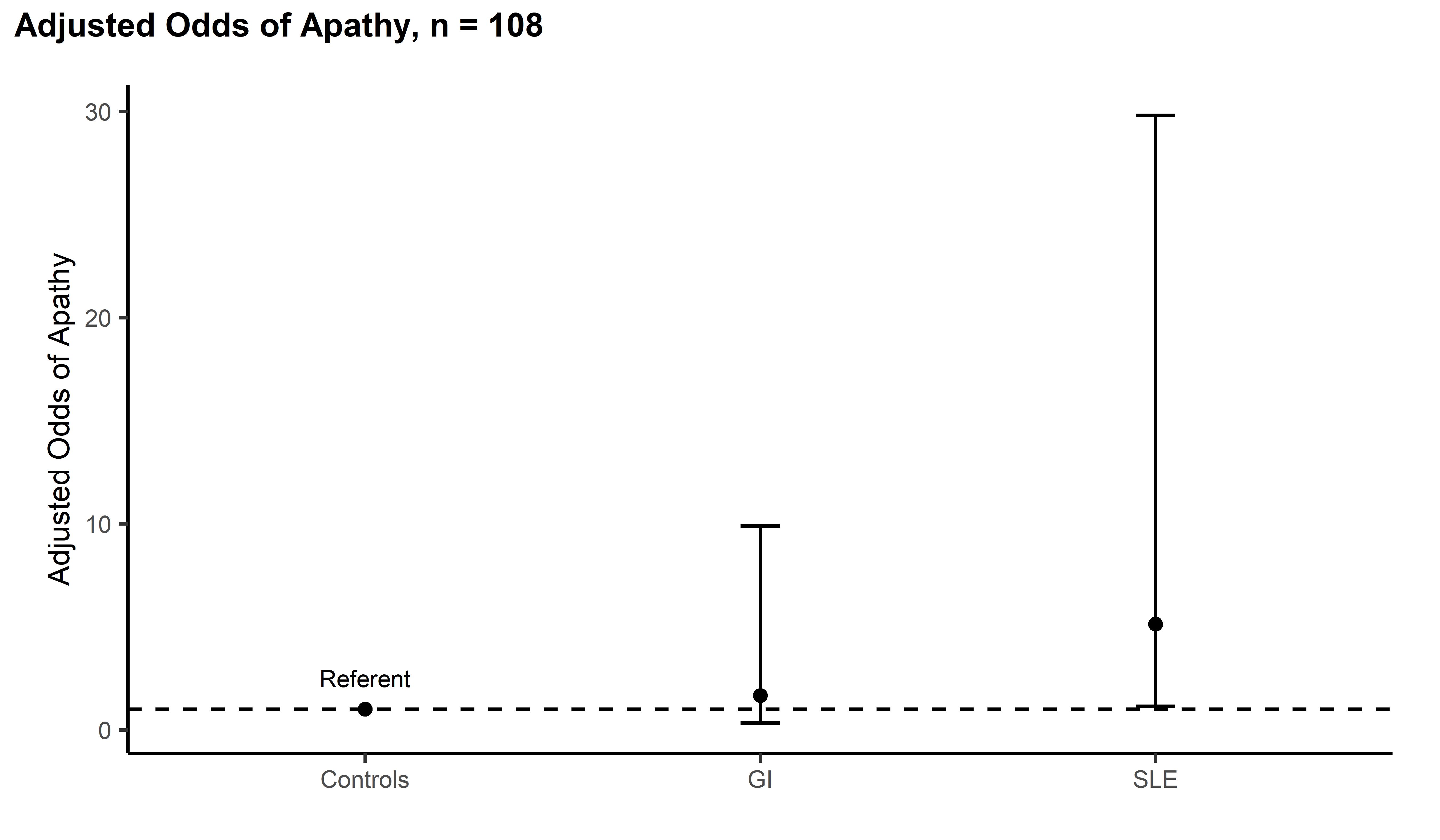 Adjusted Odds of Apathy by Group
Adjusted Odds of Apathy by Group
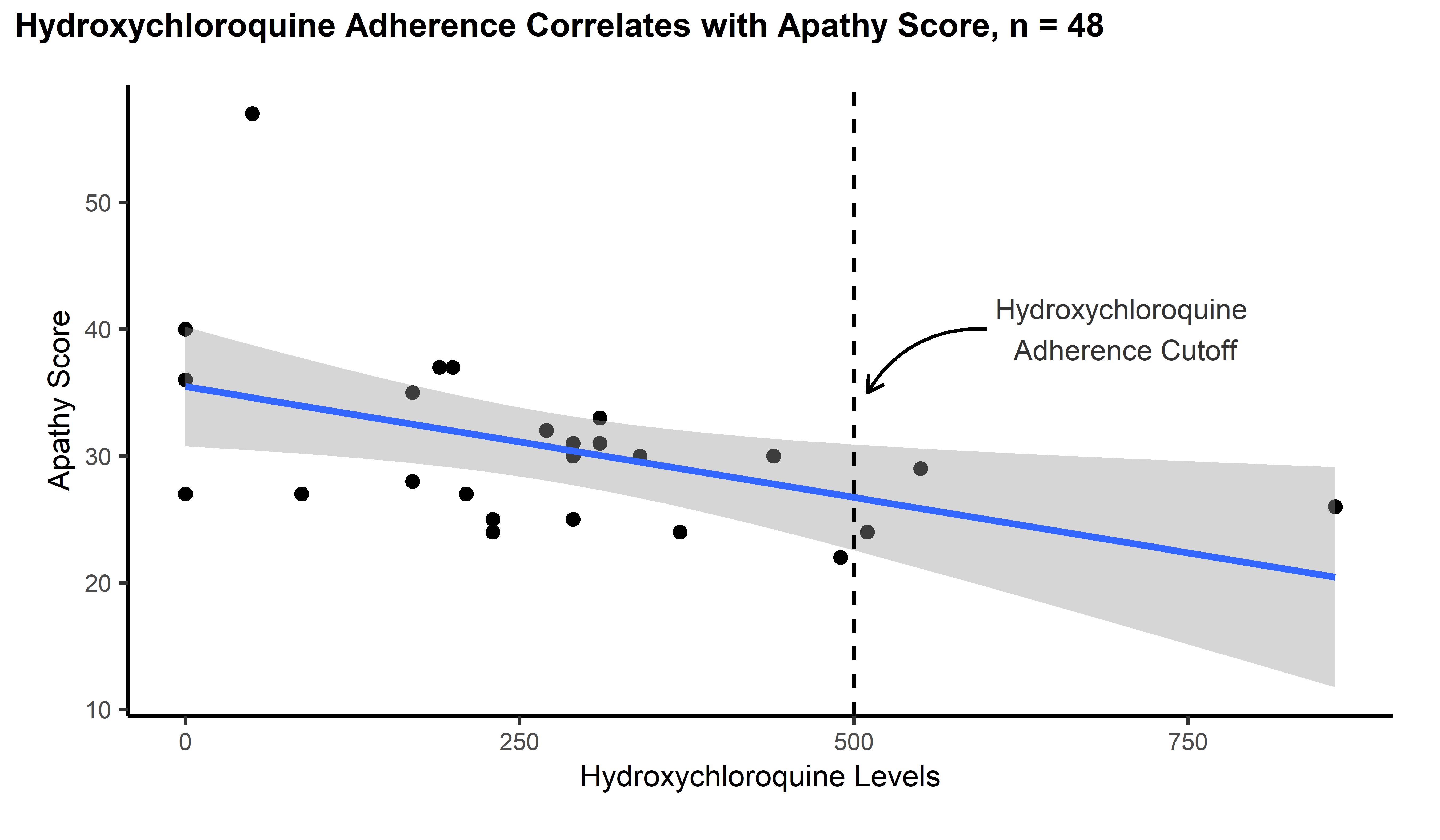 Apathy association with Hydroxychloroquine levels
Apathy association with Hydroxychloroquine levels
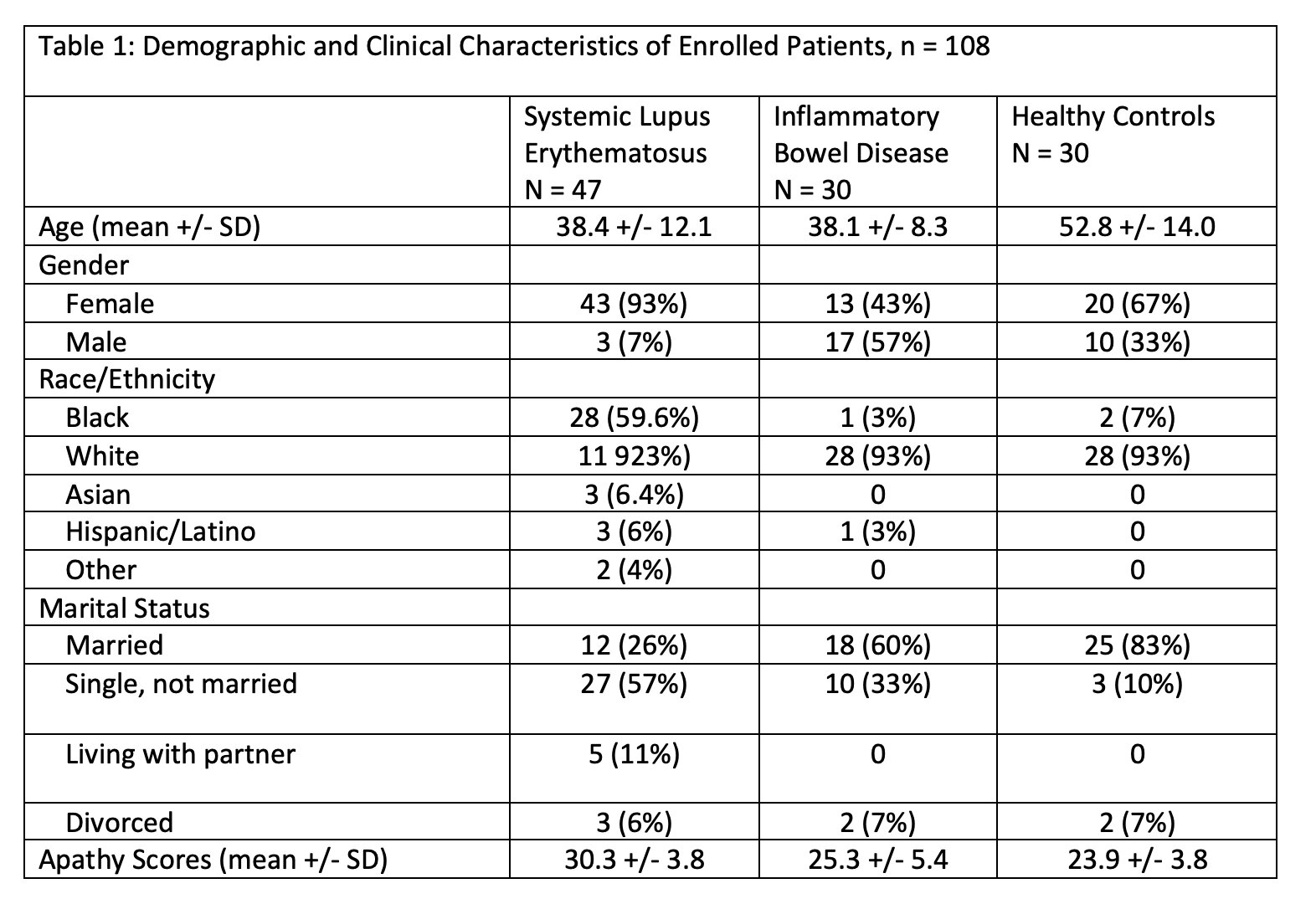 Demographics and Characteristics of Enrolled patients
Demographics and Characteristics of Enrolled patients
Disclosures: M. Putman, AstraZeneca, AbbVie/Abbott, Novartis; D. Gazeley, None; I. Mbonu, None.
Background/Purpose: Up to 40% of patients with systemic lupus erythematosus (SLE) have measurable cognitive dysfunction on neuropsychiatric testing. Around 83% of patients are nonadherent with hydroxychloroquine (HCQ), a foundational and well tolerated medication in lupus treatment. We hypothesized that many more patients experience some form of cognitive dysfunction that contributes to medication nonadherence. In Parkinson's disease, apathy has been associated with functional decline, medication nonadherence, poor executive function and lower quality of life. No prior studies have investigated apathy in a prospective cohort of patients with SLE.
Methods: Adult, English-speaking patients ≥18 years old with SLE were consecutively approached to participate. For comparator groups, patients with inflammatory bowel disease (IBD) were recruited at Medical College of Wisconsin (MCW) gastroenterology clinic and healthy controls were recruited from a MCW Sports Medicine clinic. Patients completed the Apathy Evaluation Scale (AES), a validated 18 item, self-administered survey. Scores on the survey range from 18-72, with higher scores suggesting higher level of apathy. A score of 31 was used to dichotomize the score into apathy-present or apathy-absent. Adherence to HCQ levels were defined by a serum level of 500 ng/ml at baseline. Categorical variables were compared using Fishers exact test, bivariate differences in apathy were assessed using a one-way ANOVA, the dichotomized apathy score evaluated in a logistic regression model that controlled for age, gender, and race/ethnicity, and the association between HCQ serum levels and apathy were analyzed in a linear regression.
Results: In total 107 patients were enrolled (47 SLE, 30 IBD, 30 healthy controls). Patients with SLE were more likely to be female (93% SLE vs. 43% IBD vs. 67% healthy controls, p < 0.01), Black/African American (60% SLE vs. 3% IBD vs. 7% healthy controls, p < 0.01), and single, not married (55% SLE vs. 33% IBD vs. 10% healthy controls, p < 0.01). The overall mean apathy score was 26.8 with a standard deviation (SD) of 6.1; higher apathy scores were observed in patients with SLE (30.3 +/- 3.8 SLE vs. 25.3 +/- 5.4 IBD vs. 23.9 +/- 3.8 healthy controls, p < 0.01). In a logistic regression model that evaluated apathy as a dichotomous variable, patients with SLE had higher adjusted odds of apathy as compared to healthy controls (OR 5.1, CI 1.1-29.8). Four out of 32 patients (12%) were adherent to HCQ when defined by baseline serum HCQ levels ≥500 ng/ml. In a linear regression model of the SLE cohort, HCQ serum levels decreased by 0.017 ng/ml for every increase of 1 on the apathy scale (p = 0.02).
Conclusion: In this study, patients with SLE had higher levels of apathy as compared to healthy controls. Lower serum HCQ levels correlated with higher measured apathy level. Future studies should confirm these preliminary findings and may investigate interventions to address apathy.
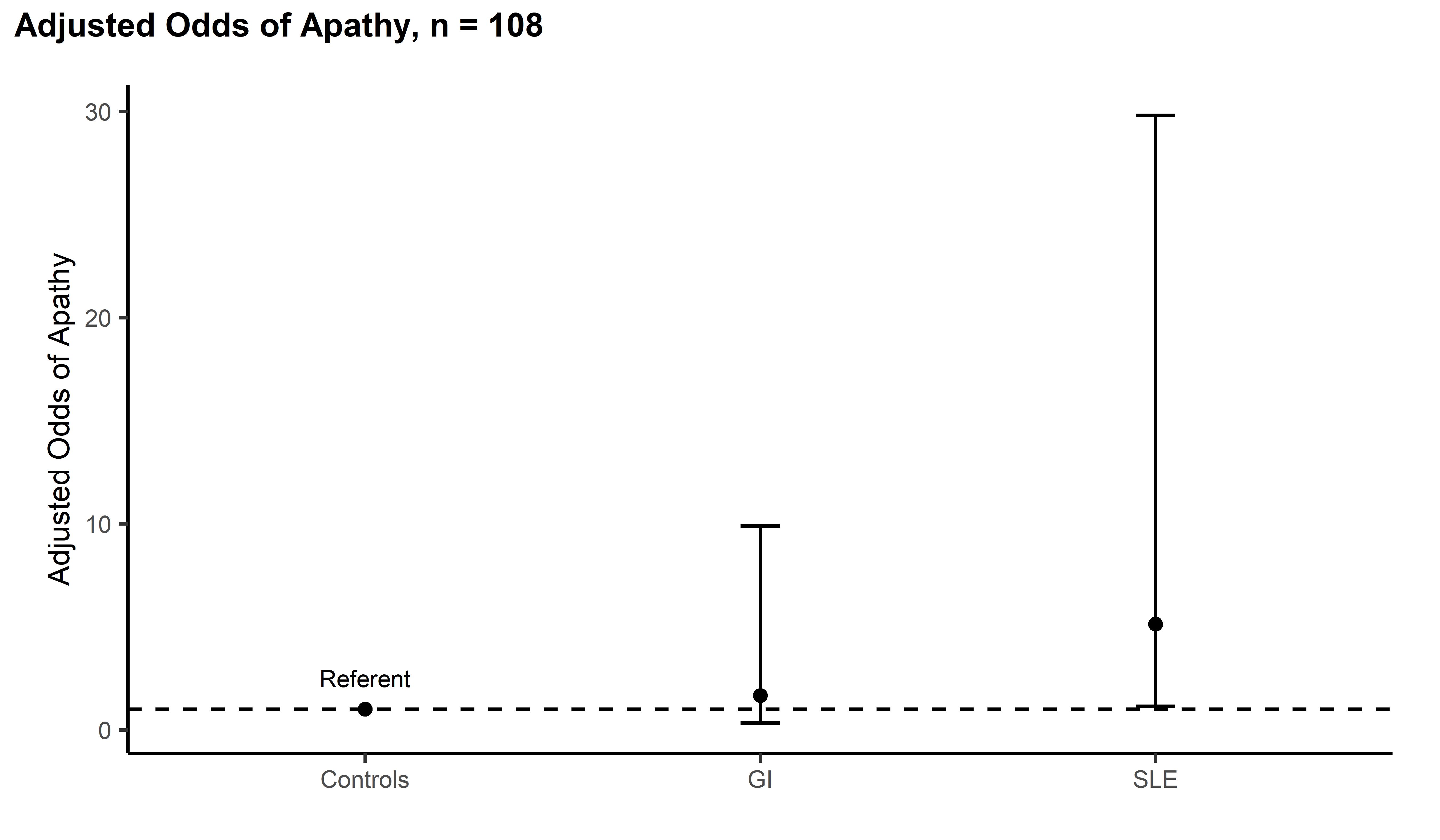 Adjusted Odds of Apathy by Group
Adjusted Odds of Apathy by Group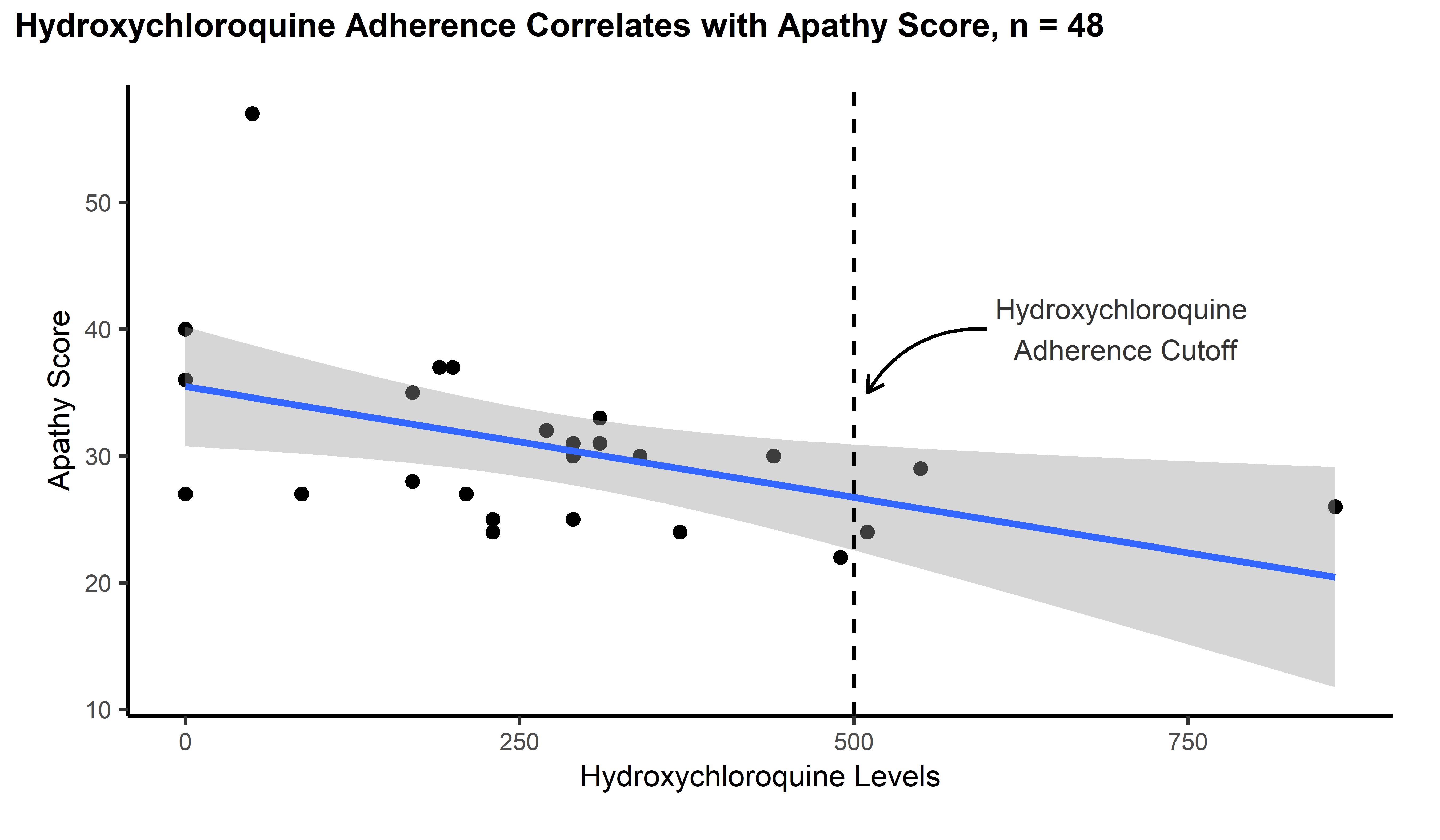 Apathy association with Hydroxychloroquine levels
Apathy association with Hydroxychloroquine levels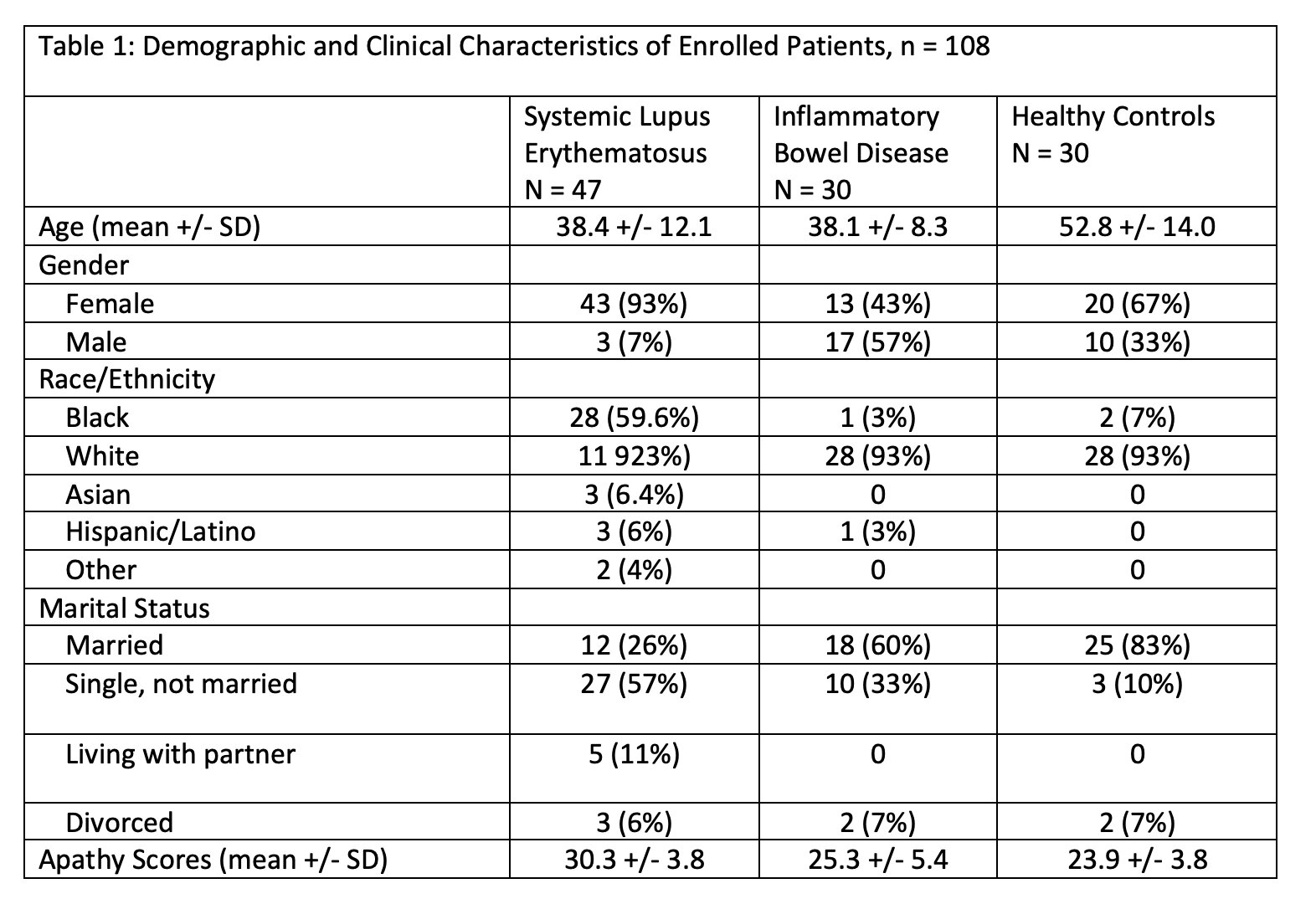 Demographics and Characteristics of Enrolled patients
Demographics and Characteristics of Enrolled patientsDisclosures: M. Putman, AstraZeneca, AbbVie/Abbott, Novartis; D. Gazeley, None; I. Mbonu, None.

