Back
Poster Session C
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (1486–1517) Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster III
1502: Assessment of Perceptions and Practices Regarding the Collaborative Management of Patients with Psoriatic Arthritis Among US Dermatology and Rheumatology Teams
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- ES
Evan Siegel, MD
Arthritis and Rheumatism Associates
Potomac, MD, United States
Abstract Poster Presenter(s)
Evan Siegel1, Amit Garg2, Jeffrey Carter3, Laura Simone4 and Marykate Nelson5, 1Georgetown University School of Medicine, Washington, DC, 2Zucker School of Medicine at Hofstra/Northwell, Lake Success, NY, 3PRIME Education, Boynton Beach, FL, 4PRIME Education, Omaha, NE, 5PRIME Education, Drexel Hill, PA
Background/Purpose: The optimal care of psoriatic arthritis (PsA) requires effective collaboration between rheumatology and dermatology teams. We executed an initiative to identify gaps and inform team-based improvements in PsA co-management.
Methods: Surveys on clinical practice trends and challenges were administered to 14 clinical teams (7 rheumatology and 7 dermatology practices, which were regionally paired). The paired rheumatology and dermatology teams then engaged in an interactive educational session, led by expert faculty, to review their survey data and set action plans.
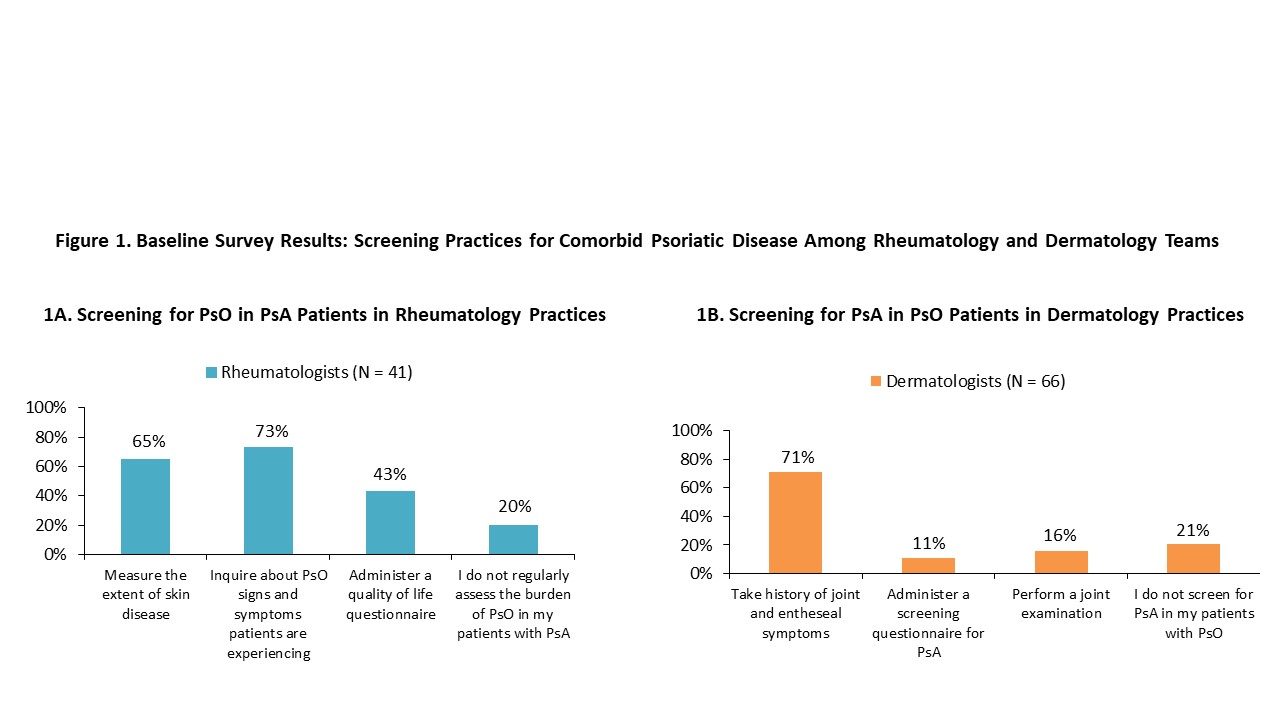
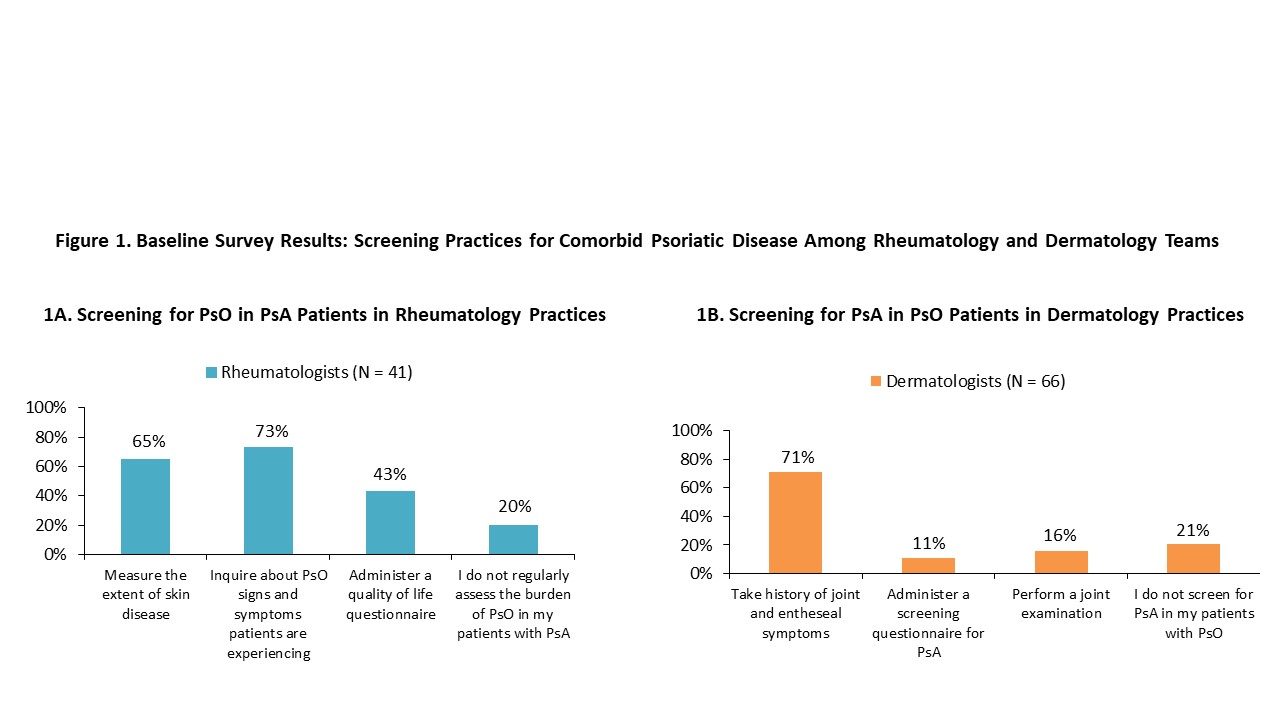
Results: Surveys were completed by 41 rheumatology healthcare professionals (HCPs) (32% physicians) and 66 dermatology HCPs (25% physicians) with an average of 8 years caring for patients with psoriatic disease (PsD). Results from these surveys revealed challenges in the comprehensive management of PsD. For example, 72% of dermatology HCPs were unsure how many of their psoriasis (PsO) patients had been diagnosed with PsA. One-half of rheumatology HCPs listed "differentiating PsO from other skin conditions" as a top challenge in managing patients with PsD, and 54% of dermatology HCPs answered "differentiating PsA from other joint pain conditions." Only 36% of rheumatology HCPs and 12% of dermatology HCPs reported high confidence in performing these actions. Only approximately one-fourth of survey respondents reported that they always educate their PsA/PsO patients about the risks and symptoms of comorbid PsD. PsO screening practices among rheumatology HCPs and PsA screening practices among dermatology HCPs were inadequate, with one-fifth not screening at all (Figure 1).
Survey data also revealed that collaboration between these specialties is inadequate. Less than one-half of rheumatology HCPs (48%) reported that they collaborate with a dermatologist as soon as a PsA patient exhibits skin symptoms. Only 58% of dermatology HCPs reported that they collaborate with a rheumatologist as soon as a PsO patient exhibits joint symptoms. Only 34% of rheumatology HCPs collaborated with dermatologists in the management of their PsA patients with diagnosed PsO or complaints of skin symptoms; only 50% of dermatology HCPs collaborated with rheumatologists in the management of their PsO patients with diagnosed PsA or complaints of joint symptoms. Suboptimal proportions of respondents were implementing specific collaborative strategies prior to the educational session (Figure 2). The resources most frequently reported to be needed to adopt these strategies were additional education and updated technology/electronic medical record (EMR) systems. The most commonly reported areas rheumatology and dermatology teams planned to address following the educational session were early screening and identification, timely referrals, and improved co-management between these specialty teams.
Conclusion: These survey findings reveal suboptimal screening for PsD and inadequate collaboration between rheumatology and dermatology care teams in the management of this disease. Future educational initiatives and real-world system changes are needed to further close these gaps in care.
.jpg)
Disclosures: E. Siegel, AbbVie/Abbott, Bristol-Myers Squibb(BMS), Eli Lilly, Janssen, UCB; A. Garg, AbbVie/Abbott, Janssen, Pfizer, UCB, Asana Biosciences, Incyte; J. Carter, None; L. Simone, None; M. Nelson, None.
Background/Purpose: The optimal care of psoriatic arthritis (PsA) requires effective collaboration between rheumatology and dermatology teams. We executed an initiative to identify gaps and inform team-based improvements in PsA co-management.
Methods: Surveys on clinical practice trends and challenges were administered to 14 clinical teams (7 rheumatology and 7 dermatology practices, which were regionally paired). The paired rheumatology and dermatology teams then engaged in an interactive educational session, led by expert faculty, to review their survey data and set action plans.
Results: Surveys were completed by 41 rheumatology healthcare professionals (HCPs) (32% physicians) and 66 dermatology HCPs (25% physicians) with an average of 8 years caring for patients with psoriatic disease (PsD). Results from these surveys revealed challenges in the comprehensive management of PsD. For example, 72% of dermatology HCPs were unsure how many of their psoriasis (PsO) patients had been diagnosed with PsA. One-half of rheumatology HCPs listed "differentiating PsO from other skin conditions" as a top challenge in managing patients with PsD, and 54% of dermatology HCPs answered "differentiating PsA from other joint pain conditions." Only 36% of rheumatology HCPs and 12% of dermatology HCPs reported high confidence in performing these actions. Only approximately one-fourth of survey respondents reported that they always educate their PsA/PsO patients about the risks and symptoms of comorbid PsD. PsO screening practices among rheumatology HCPs and PsA screening practices among dermatology HCPs were inadequate, with one-fifth not screening at all (Figure 1).
Survey data also revealed that collaboration between these specialties is inadequate. Less than one-half of rheumatology HCPs (48%) reported that they collaborate with a dermatologist as soon as a PsA patient exhibits skin symptoms. Only 58% of dermatology HCPs reported that they collaborate with a rheumatologist as soon as a PsO patient exhibits joint symptoms. Only 34% of rheumatology HCPs collaborated with dermatologists in the management of their PsA patients with diagnosed PsO or complaints of skin symptoms; only 50% of dermatology HCPs collaborated with rheumatologists in the management of their PsO patients with diagnosed PsA or complaints of joint symptoms. Suboptimal proportions of respondents were implementing specific collaborative strategies prior to the educational session (Figure 2). The resources most frequently reported to be needed to adopt these strategies were additional education and updated technology/electronic medical record (EMR) systems. The most commonly reported areas rheumatology and dermatology teams planned to address following the educational session were early screening and identification, timely referrals, and improved co-management between these specialty teams.
Conclusion: These survey findings reveal suboptimal screening for PsD and inadequate collaboration between rheumatology and dermatology care teams in the management of this disease. Future educational initiatives and real-world system changes are needed to further close these gaps in care.
.jpg)
Disclosures: E. Siegel, AbbVie/Abbott, Bristol-Myers Squibb(BMS), Eli Lilly, Janssen, UCB; A. Garg, AbbVie/Abbott, Janssen, Pfizer, UCB, Asana Biosciences, Incyte; J. Carter, None; L. Simone, None; M. Nelson, None.

