Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1186–1214) Epidemiology and Public Health Poster II
1206: Association Between Different Alcoholic Beverages and Serum Urate Level: A Cross-Sectional Study Using Large Medical Checkup Data
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SF
Sho Fukui, MD, MPH
Kyorin University Hospital
Tokyo, Japan
Abstract Poster Presenter(s)
Sho Fukui1, Masato Okada2, Mahbubur Rahman3, Takehiro Nakai2, Hiromichi Tamaki2, Hiroki Matsui4, Atsushi Shiraishi5, Mitsumasa Kishimoto6, Hiroshi Hasegawa7, Takeaki Matsuda7 and Kazuki Yoshida8, 1Kyorin University Hospital, Tokyo, Japan, 2St. Luke's International Hospital, Tokyo, Japan, 3Graduate School of Public Health, St. Luke’s International University, Tokyo, Japan, 4Clinical Research Support Office, Kameda Medical Center, Kamogawa, Japan, 5Emergency and Trauma Center, Kameda Medical Center, Kamogawa, Japan, 6Kyorin University School of Medicine, Yokohama, Japan, 7Kyorin University, Tokyo, Japan, 8Brigham and Women's Hospital, Boston, MA
Background/Purpose: Alcohol consumption is associated with increased serum urate levels. However, data regarding the differences in the extent of the association between various types of alcoholic beverages have been limited. We aimed to assess the difference in serum urate levels between types of alcoholic beverages when their intakes were standardized for their ethanol content.
Methods: We conducted a cross-sectional study using large medical checkup data obtained between 2012 and 2021. The unit of each beverage was standardized to a standard drink which included 20 g of ethanol (500 ml of beer, 167 ml of sake[Japanese rice wine], 100 ml of shochu [Japanese spirit], 208 ml of wine, and 62.5 ml of whiskey). Specific alcohol beverage-dominant groups or a mixed-alcohol group were determined based on the beverage that accounted for 75% or more of the total ethanol consumption. The association between serum urate and the main alcohol beverage was analyzed using the multivariable linear regression model which included the interaction of alcohol consumption and dominant alcohol beverage types. In all analyses, age, body mass index, kidney function, medical conditions (hypertension, diabetes, and dyslipidemia), smoking status, daily physical activity, exercise level, and dietary habits were adjusted as covariates, and analyses were stratified by gender. Relationships between serum urate and the amount of daily alcoholic beverages were flexibly visualized by cubic splines with knots by 5, 35, 65, and 95 percentiles.
Results: A total of 78,170 participants included in this study. The mean age was 47.6 (SD 12.8) years, 36471 (46.7%) were male and 41,699 (53.3%) were regular alcohol drinkers (Figure 1). Beer dominant group showed strong positive associations between alcohol consumption and serum urate level based on multivariable linear regression along with interaction effect (marginal effect: 0.14 [0.12, 0.17]; p < 0.001 in male, 0.24 [0.21, 0.27]; p < 0.001 in female). When compared with beer-dominant groups, the model with interaction term revealed significant differences in the relationship between serum urate and alcohol consumption in sake, shochu-dominant and mixed-group of males (Sake -0.09 [-0.15, -0.02]; p = 0.004, Shochu -0.08 [-0.12, -0.05] ; p < 0.001, Mixed -0.09 [-0.12, -0.05]; p < 0.001) and in all other beverage groups of females (Sake -0.19 [-0.29, -0.09]; p < 0.001, Shochu -0.12 [-0.18, -0.07]; p < 0.001, Wine -0.11 [-0.16, -0.06]; p < 0.001, Whiskey -0.18 [-0.29, -0.06]; p = 0.002, Mixed -0.15 [-0.20, -0.11]; p < 0.001) (Figure 2). Restricted cubic splines showed different patterns in the relationship between serum urate and ethanol intake by alcohol beverages (Figure 3).
Conclusion: This large cross-sectional study observed the extent of relationship between serum urate and ethanol intake was different between alcoholic beverages. Higher beer consumption was consistently associated with a higher SU, whereas sake showed only modest associations in both males and females.
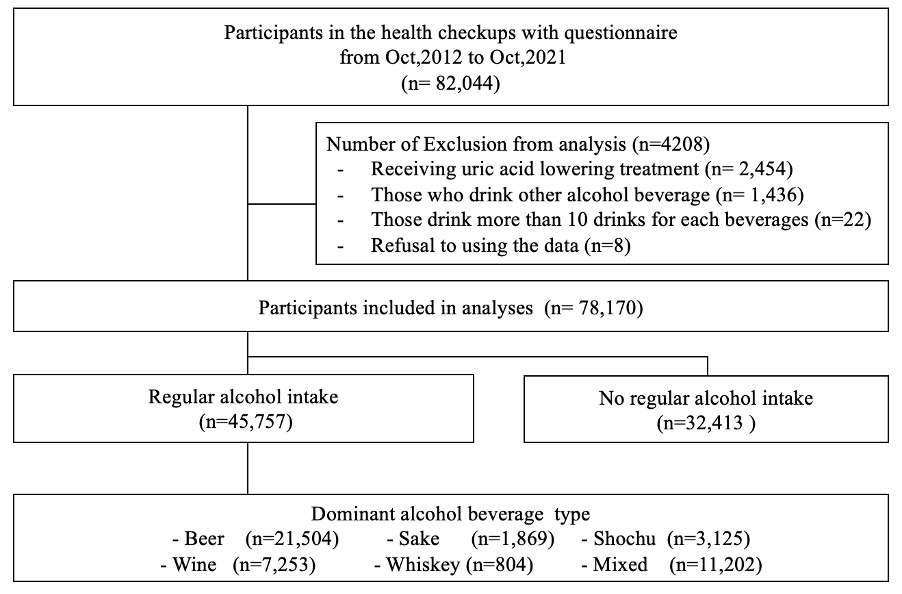 Figure 1. Flow chart of inclusion and exclusion of participants
Figure 1. Flow chart of inclusion and exclusion of participants
.jpg) Figure 2 Types of Dominant Alcohol Beverages and Predicted serum urate
Figure 2 Types of Dominant Alcohol Beverages and Predicted serum urate
SD, Standard drink
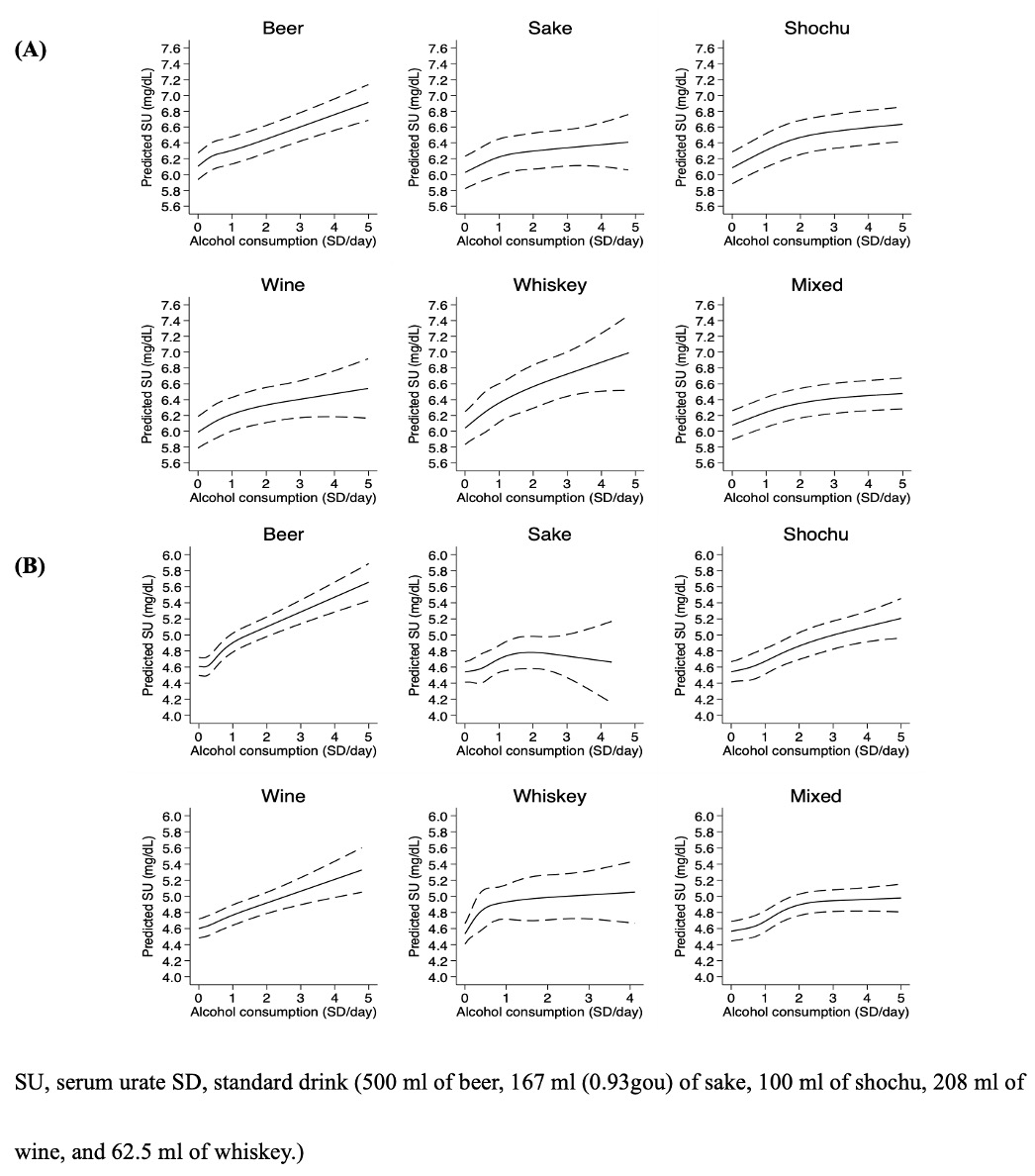 Figure 3. Predicted serum urate and alcohol consumption in each dominant alcohol beverage type using restricted cubic spline with knots by percentile (5, 35, 65, 95) in (A) Male and (B) Female.
Figure 3. Predicted serum urate and alcohol consumption in each dominant alcohol beverage type using restricted cubic spline with knots by percentile (5, 35, 65, 95) in (A) Male and (B) Female.
Disclosures: S. Fukui, None; M. Okada, None; M. Rahman, None; T. Nakai, None; H. Tamaki, None; H. Matsui, None; A. Shiraishi, None; M. Kishimoto, AbbVie, Amgen, Astellas BioPharma, Asahi-Kasei Pharma, Ayumi Pharma, Bristol-Myers Squibb(BMS), Celgene, Chugai, Daiichi-Sankyo, Eisai, Eli Lilly, Gilead, Janssen, Kyowa Kirin, Novartis, Ono Pharma, Pfizer, Tanabe-Mitsubishi, Teijin Pharma, UCB; H. Hasegawa, None; T. Matsuda, None; K. Yoshida, None.
Background/Purpose: Alcohol consumption is associated with increased serum urate levels. However, data regarding the differences in the extent of the association between various types of alcoholic beverages have been limited. We aimed to assess the difference in serum urate levels between types of alcoholic beverages when their intakes were standardized for their ethanol content.
Methods: We conducted a cross-sectional study using large medical checkup data obtained between 2012 and 2021. The unit of each beverage was standardized to a standard drink which included 20 g of ethanol (500 ml of beer, 167 ml of sake[Japanese rice wine], 100 ml of shochu [Japanese spirit], 208 ml of wine, and 62.5 ml of whiskey). Specific alcohol beverage-dominant groups or a mixed-alcohol group were determined based on the beverage that accounted for 75% or more of the total ethanol consumption. The association between serum urate and the main alcohol beverage was analyzed using the multivariable linear regression model which included the interaction of alcohol consumption and dominant alcohol beverage types. In all analyses, age, body mass index, kidney function, medical conditions (hypertension, diabetes, and dyslipidemia), smoking status, daily physical activity, exercise level, and dietary habits were adjusted as covariates, and analyses were stratified by gender. Relationships between serum urate and the amount of daily alcoholic beverages were flexibly visualized by cubic splines with knots by 5, 35, 65, and 95 percentiles.
Results: A total of 78,170 participants included in this study. The mean age was 47.6 (SD 12.8) years, 36471 (46.7%) were male and 41,699 (53.3%) were regular alcohol drinkers (Figure 1). Beer dominant group showed strong positive associations between alcohol consumption and serum urate level based on multivariable linear regression along with interaction effect (marginal effect: 0.14 [0.12, 0.17]; p < 0.001 in male, 0.24 [0.21, 0.27]; p < 0.001 in female). When compared with beer-dominant groups, the model with interaction term revealed significant differences in the relationship between serum urate and alcohol consumption in sake, shochu-dominant and mixed-group of males (Sake -0.09 [-0.15, -0.02]; p = 0.004, Shochu -0.08 [-0.12, -0.05] ; p < 0.001, Mixed -0.09 [-0.12, -0.05]; p < 0.001) and in all other beverage groups of females (Sake -0.19 [-0.29, -0.09]; p < 0.001, Shochu -0.12 [-0.18, -0.07]; p < 0.001, Wine -0.11 [-0.16, -0.06]; p < 0.001, Whiskey -0.18 [-0.29, -0.06]; p = 0.002, Mixed -0.15 [-0.20, -0.11]; p < 0.001) (Figure 2). Restricted cubic splines showed different patterns in the relationship between serum urate and ethanol intake by alcohol beverages (Figure 3).
Conclusion: This large cross-sectional study observed the extent of relationship between serum urate and ethanol intake was different between alcoholic beverages. Higher beer consumption was consistently associated with a higher SU, whereas sake showed only modest associations in both males and females.
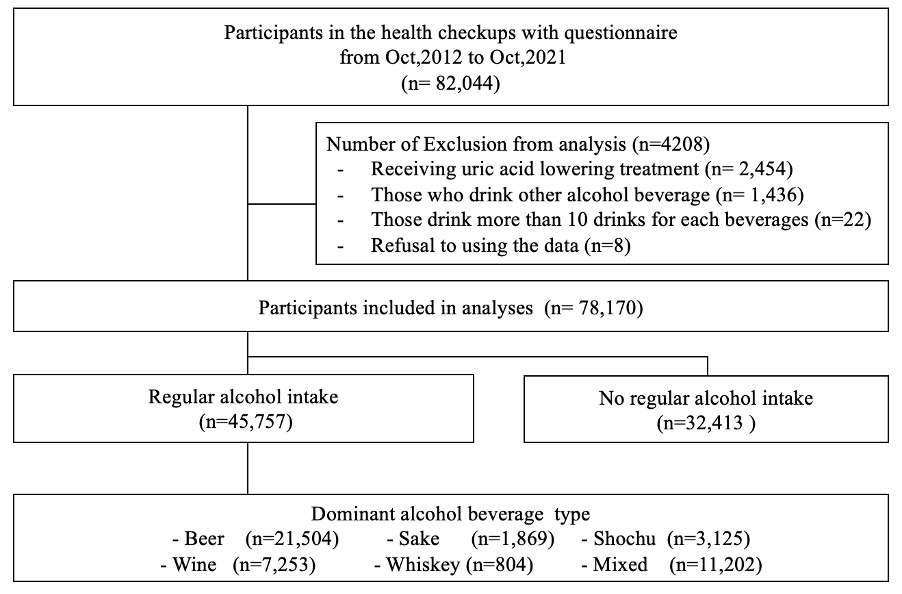 Figure 1. Flow chart of inclusion and exclusion of participants
Figure 1. Flow chart of inclusion and exclusion of participants.jpg) Figure 2 Types of Dominant Alcohol Beverages and Predicted serum urate
Figure 2 Types of Dominant Alcohol Beverages and Predicted serum urateSD, Standard drink
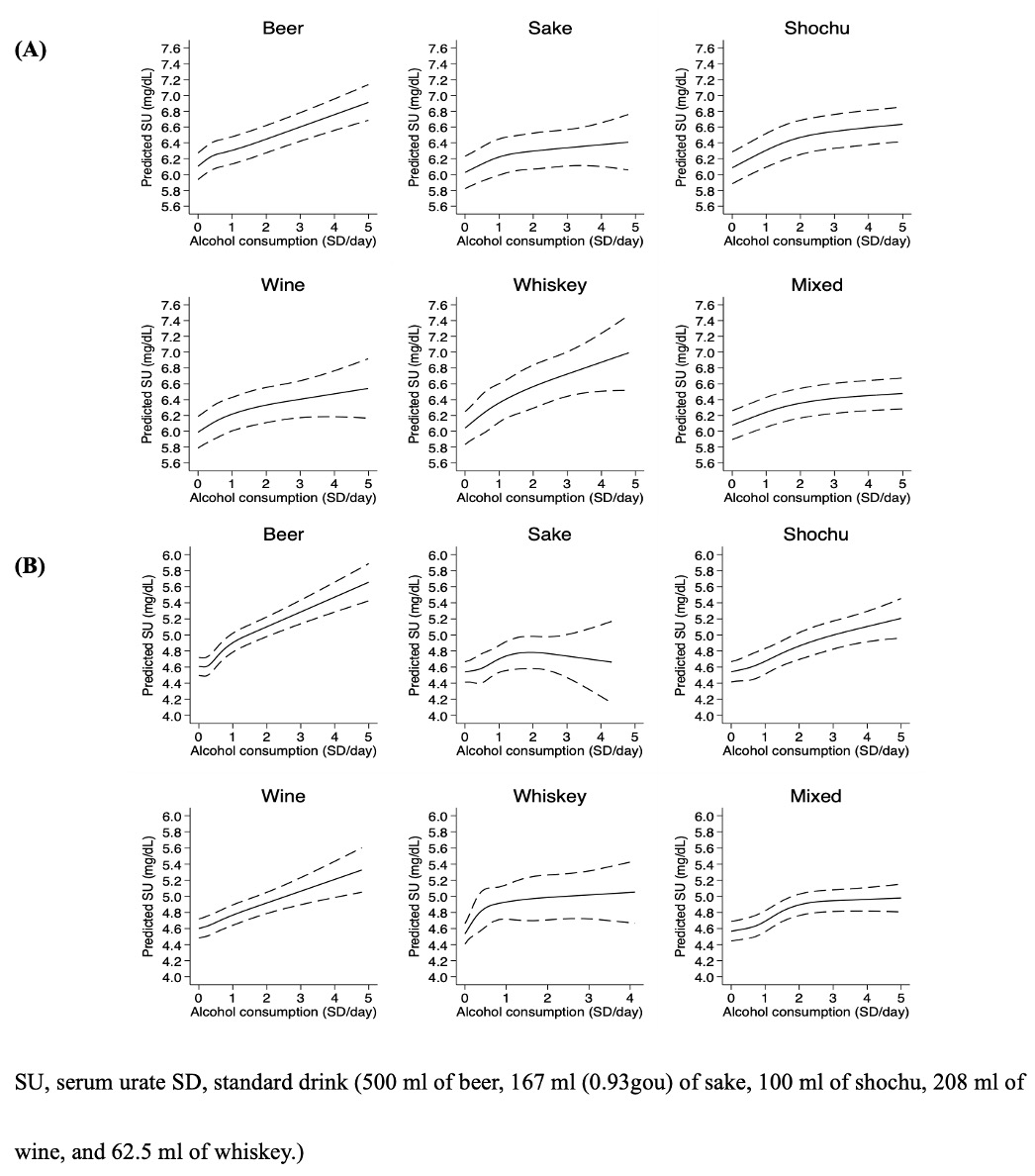 Figure 3. Predicted serum urate and alcohol consumption in each dominant alcohol beverage type using restricted cubic spline with knots by percentile (5, 35, 65, 95) in (A) Male and (B) Female.
Figure 3. Predicted serum urate and alcohol consumption in each dominant alcohol beverage type using restricted cubic spline with knots by percentile (5, 35, 65, 95) in (A) Male and (B) Female.Disclosures: S. Fukui, None; M. Okada, None; M. Rahman, None; T. Nakai, None; H. Tamaki, None; H. Matsui, None; A. Shiraishi, None; M. Kishimoto, AbbVie, Amgen, Astellas BioPharma, Asahi-Kasei Pharma, Ayumi Pharma, Bristol-Myers Squibb(BMS), Celgene, Chugai, Daiichi-Sankyo, Eisai, Eli Lilly, Gilead, Janssen, Kyowa Kirin, Novartis, Ono Pharma, Pfizer, Tanabe-Mitsubishi, Teijin Pharma, UCB; H. Hasegawa, None; T. Matsuda, None; K. Yoshida, None.

