Back
Poster Session C
Systemic lupus erythematosus (SLE)
Session: (1440–1485) SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
1466: Cardiovascular Risk Assessment in Patients with Systemic Lupus Erythematosus: Comparison Between QRISK and aGAPSS Scores
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SS
Savino Sciascia, MD
University of Turin
Torino, Turin, Italy
Abstract Poster Presenter(s)
Alice Barinotti1, Massimo Radin1, Irene Cecchi2, Silvia Grazietta Foddai1, Simone Baldovino1, Elisa Menegatti1, Daniela Rossi1, Vittorio Modena1, Dario Roccatello1 and Savino Sciascia2, 1University of Turin, Turin, Italy, 2University of Turin, Torino, Italy
Background/Purpose: Cardiovascular diseases (CVDs) represent one of the most life-threatening conditions that can affect SLE patients. Assessing the potential CVD risk of these patients is stilla challenge and an important aspect in the clinical practice. Recently the QRISK3 score has attempted to encompass for SLE augmented thrombotic risk by adding items (such as corticosteroid use) that are missing in traditional CVD risk scores. The aim of this work was to apply and compare the QRISK3 and the adjusted Global AntiPhospholipid Syndrome Score (aGAPSS), a validated score to assess CVD and overall thrombotic risk in aPL positive patients, in a cohort of SLE patients with and without a concomitant diagnosis of APS.
Methods: During a period of 6 months (Sep 2019 – Feb 2020) 25-84 years old patients with a confirmed diagnosis of SLE (2019 ACR/EULAR classification criteria) and/or a diagnosis of SAPS (Sidney criteria) were recruited. QRISK3 has been calculated using the official online calculator (https://qrisk.org/). aGAPSS has been calculated using the validated point values based on aPL profile and independent risk factors: aCL=5, aβ2GPI=4, LA=4, aPS/PT=3, hyperlipidemia=3, hypertension=1.
Results: The analysis included a cohort of 142 SLE patients: 34 SAPS (23.9%) and 108 SLE patients without APS (76.1%), with a mean age of 48±12.9 (SAPS=51.6±12.8/SLE without APS=46.9±12.8). Table 1 summarizes patients characteristics. When focusing on cerebrovascular/coronary events, we found a statistical significance with respect to aGAPSS (pt with event =10.1±6.2 vs pt without event=5.8±6.1; p=0.007), but not QRISK3. Also, a significant association was observed between the occurrence of these events and high risk aGAPSS: p=0.03 for aGAPSS≥8, p=0.01 for aGAPSS ≥9, p=0.008 for aGAPSS ≥10. Moreover, the aGAPSS but not the QRISK3 resulted to strongly correlate with the occurrence of any thrombotic event, both at the uni- and multivariate analysis (univariate: pt with event =8.17±7.1 vs pt without event= 5.41±5.6; p=0.012 / multivariate: p=0.009) (Figure 1). The same was observed for gender: male gender resulted to correlate with the occurrence of any thrombotic event at both uni- and multivariate analysis (p=0.017 and p=0.03, respectively). Finally, when focusing on aPL profile, regardless the diagnosis, we found a statistical significance only with respect to aGAPSS (aPL+ =9.6±6.3 vs aPL- = 4.1±5.1; p< 0.001).
Conclusion: By encompassing factors that can contribute to CVD development in complex/autoimmune diseases, QRISK3 has been shown to be more accurate than traditional risk score in predicting SLE patients CVD risk. Nonetheless, the results of this analysis showed how the aGAPSS still seems to be the most valuable tool for this purpose when facing SLE patients. Moreover, the significance observed when focusing on patients' aPL profile, suggests that adding this item to the QRISK3 could be a useful strategy to improve the management.
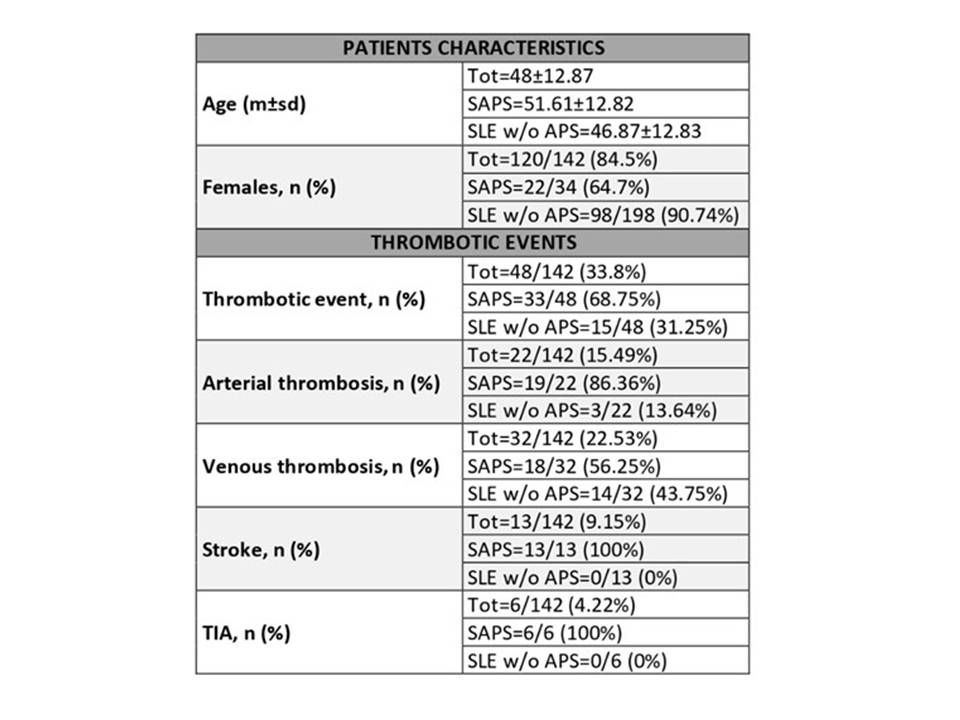 Table 1. Main demographic and clinical features of the patients included in the study.
Table 1. Main demographic and clinical features of the patients included in the study.
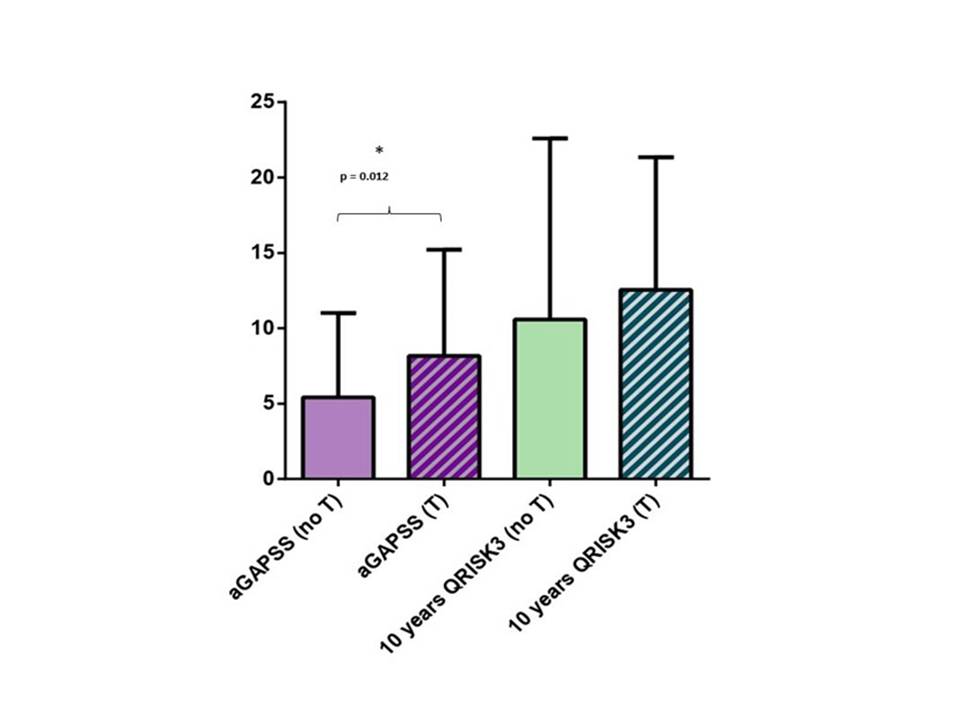 Figure 1. Mean aGAPSS and QRISK3 scores among the patients included in the study and divided according to previous thrombotic events status (both arterial and venous).
Figure 1. Mean aGAPSS and QRISK3 scores among the patients included in the study and divided according to previous thrombotic events status (both arterial and venous).
Disclosures: A. Barinotti, None; M. Radin, None; I. Cecchi, None; S. Foddai, None; S. Baldovino, None; E. Menegatti, None; D. Rossi, None; V. Modena, None; D. Roccatello, None; S. Sciascia, None.
Background/Purpose: Cardiovascular diseases (CVDs) represent one of the most life-threatening conditions that can affect SLE patients. Assessing the potential CVD risk of these patients is stilla challenge and an important aspect in the clinical practice. Recently the QRISK3 score has attempted to encompass for SLE augmented thrombotic risk by adding items (such as corticosteroid use) that are missing in traditional CVD risk scores. The aim of this work was to apply and compare the QRISK3 and the adjusted Global AntiPhospholipid Syndrome Score (aGAPSS), a validated score to assess CVD and overall thrombotic risk in aPL positive patients, in a cohort of SLE patients with and without a concomitant diagnosis of APS.
Methods: During a period of 6 months (Sep 2019 – Feb 2020) 25-84 years old patients with a confirmed diagnosis of SLE (2019 ACR/EULAR classification criteria) and/or a diagnosis of SAPS (Sidney criteria) were recruited. QRISK3 has been calculated using the official online calculator (https://qrisk.org/). aGAPSS has been calculated using the validated point values based on aPL profile and independent risk factors: aCL=5, aβ2GPI=4, LA=4, aPS/PT=3, hyperlipidemia=3, hypertension=1.
Results: The analysis included a cohort of 142 SLE patients: 34 SAPS (23.9%) and 108 SLE patients without APS (76.1%), with a mean age of 48±12.9 (SAPS=51.6±12.8/SLE without APS=46.9±12.8). Table 1 summarizes patients characteristics. When focusing on cerebrovascular/coronary events, we found a statistical significance with respect to aGAPSS (pt with event =10.1±6.2 vs pt without event=5.8±6.1; p=0.007), but not QRISK3. Also, a significant association was observed between the occurrence of these events and high risk aGAPSS: p=0.03 for aGAPSS≥8, p=0.01 for aGAPSS ≥9, p=0.008 for aGAPSS ≥10. Moreover, the aGAPSS but not the QRISK3 resulted to strongly correlate with the occurrence of any thrombotic event, both at the uni- and multivariate analysis (univariate: pt with event =8.17±7.1 vs pt without event= 5.41±5.6; p=0.012 / multivariate: p=0.009) (Figure 1). The same was observed for gender: male gender resulted to correlate with the occurrence of any thrombotic event at both uni- and multivariate analysis (p=0.017 and p=0.03, respectively). Finally, when focusing on aPL profile, regardless the diagnosis, we found a statistical significance only with respect to aGAPSS (aPL+ =9.6±6.3 vs aPL- = 4.1±5.1; p< 0.001).
Conclusion: By encompassing factors that can contribute to CVD development in complex/autoimmune diseases, QRISK3 has been shown to be more accurate than traditional risk score in predicting SLE patients CVD risk. Nonetheless, the results of this analysis showed how the aGAPSS still seems to be the most valuable tool for this purpose when facing SLE patients. Moreover, the significance observed when focusing on patients' aPL profile, suggests that adding this item to the QRISK3 could be a useful strategy to improve the management.
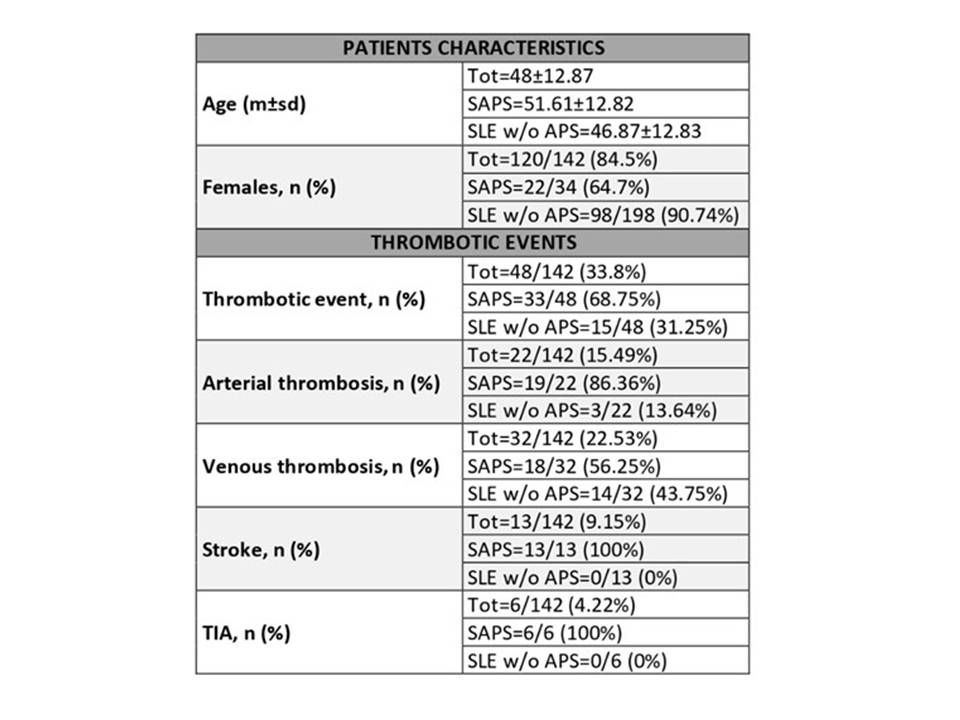 Table 1. Main demographic and clinical features of the patients included in the study.
Table 1. Main demographic and clinical features of the patients included in the study.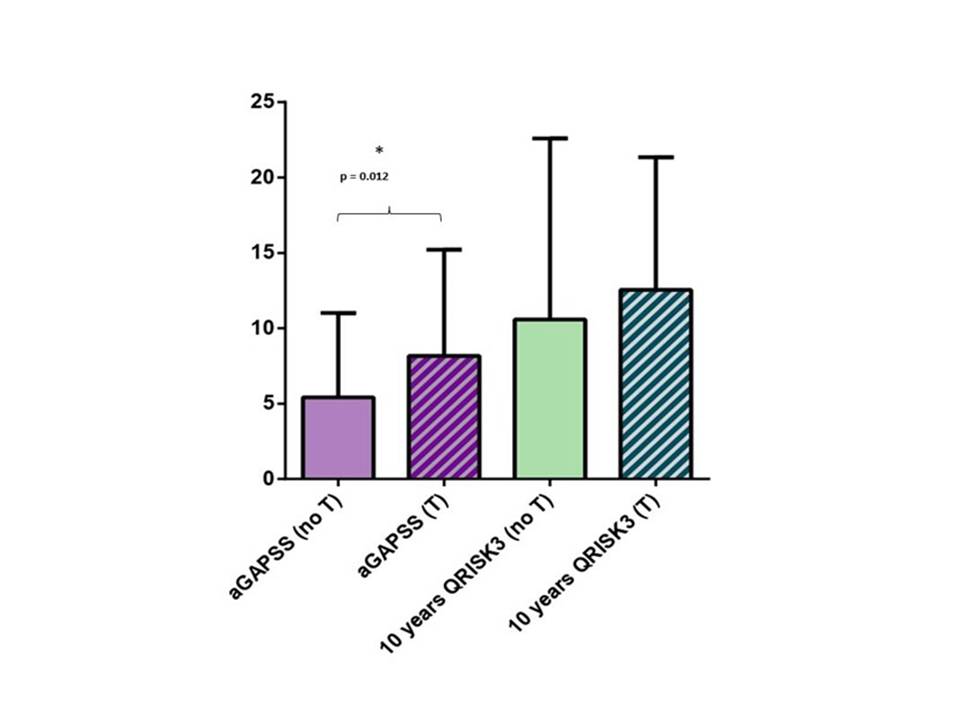 Figure 1. Mean aGAPSS and QRISK3 scores among the patients included in the study and divided according to previous thrombotic events status (both arterial and venous).
Figure 1. Mean aGAPSS and QRISK3 scores among the patients included in the study and divided according to previous thrombotic events status (both arterial and venous).Disclosures: A. Barinotti, None; M. Radin, None; I. Cecchi, None; S. Foddai, None; S. Baldovino, None; E. Menegatti, None; D. Rossi, None; V. Modena, None; D. Roccatello, None; S. Sciascia, None.

